A growing body of evidence from naturalistic longitudinal studies attests to an adverse impact of post-partum depression on the quality of the early mother—infant relationship and on the course of child socio-emotional development (Reference Murray, Cooper and GoodyerMurray & Cooper, 2003). Child cognitive development also has been found in some studies to be adversely affected (Reference Cogill, Caplan and AlexandraCogill et al, 1986; Reference Hay, Pawlby and SharpHay et al, 2001), although whether this effect applies reliably to low-risk samples and endures is uncertain (Reference Murray, Hipwell and HooperMurray et al, 1996b ; Reference Kjurstens and WolkeKjurstens & Wolke, 2001). The disruption to the early mother—infant relationship associated with maternal depression is, at least in part, responsible for the adverse child outcomes (Reference Murray, Cooper and GoodyerMurray & Cooper, 2003). Although intervention studies have shown a significant benefit of treatment in terms of maternal mood changes (Reference Holden, Sagovsky and CoxHolden et al, 1989; Reference Wickberg and HwangWickberg & Hwang, 1996; Reference Appleby, Warner and WhittonAppleby et al, 1997; Reference O'Hara, Stuart and GormanO'Hara et al, 2000), it has not been determined whether an early elevation of maternal mood leads to a corresponding improvement in the mother—infant relationship and improved child developmental progress. In order to address this question, a controlled treatment study was conducted.
METHOD
Treatments
A community sample of women with DSM—III—R (American Psychiatric Association, 1987) major depressive disorder were identified (for further details, see Reference Cooper, Murray and WilsonCooper et al, 2003, this issue). They were assigned randomly to either routine primary care or to one of three index interventions: non-directive supportive counselling, cognitive—behavioural therapy (CBT) or a brief psychodynamic psychotherapy; the nature of these treatments is described in Cooper et al (Reference Cooper, Murray and Wilson2003, this issue).
Assessments
Assessments were made before treatment, immediately after treatment (i.e. at 4.5 months post-partum) and at 18 months and 5 years post-partum by trained assessors unaware of the treatment group to which the women had been assigned. In addition to the assessment of maternal mood outlined in Cooper et al (Reference Cooper, Murray and Wilson2003, this issue), several assessments were made of the mother—infant relationship and of the dimensions of child developmental progress.
Post-treatment outcomes
Four-month outcomes
Early maternal management of infant behaviour, and problems in the mother—infant relationship. A checklist was devised specifically for this project, covering the mother's experience of managing infant behaviour difficulties (feeding, sleeping, crying) and problems in the mother's relationship with the infant (infant demands for attention, separation problems, difficulties with playing and general difficulties in relating to the infant). The mothers rated possible difficulties on a four-point severity scale (from ‘not at all’ to ‘a great deal’) before treatment and immediately after treatment.
Mother—infant interactions. Videotapes of the mother and infant interacting in a 5-min face-to-face play session at the 8- and 18-week post-partum assessments (i.e. before treatment and at the end of treatment) were rated by an independent assessor using the global rating scales devised by Murray et al (Reference Murray, Fiori-Cowley and Hooper1996a ). This rating system, in common with others used to assess the quality of engagement between mothers with depression and their infants (e.g. Reference Tronick, Als and BrazeltonTronick et al, 1980; Reference Cohn, Matias, Tronick, Tronick and FieldCohn et al, 1986; Reference Field, Healy and GoldsteinField et al, 1990) includes micro-analytical assessment of maternal responsiveness to the infant's cues. The principal dimension assessed is that of general sensitivity (including consideration of maternal warmth, acceptance and responsiveness), a measure found to discriminate between women with and without depression in community samples in the UK (Reference Murray, Fiori-Cowley and HooperMurray et al, 1996a ).
The face-to-face interactions were videotaped in the home. When the infant was in an alert and calm state, the mother sat opposite the infant and was asked to play with him or her. The video camera was positioned to film over the mother's shoulder in order to obtain a full-face image of the infant, and the mother's full-face image was filmed simultaneously, reflected in a mirror placed adjacent to the infant.
Eighteen-month outcomes
Later infant emotional and behavioural problems. At 18 months post-partum all the women were interviewed using the Behavioural Screening Questionnaire (BSQ; Reference Richman and GrahamRichman & Graham, 1971), modified for use with this age group (Reference MurrayMurray, 1992). This measure includes infant difficulties such as sleep disturbance, feeding problems, separation problems and excessive temper tantrums, and it has been found to distinguish between infants of mothers with and without depression (Reference MurrayMurray, 1992).
Infant attachment. Infant attachment to the mother was assessed at 18 months in the research unit using the Ainsworth Strange Situation Procedure (Reference Ainsworth, Blehar and WatersAinsworth et al, 1978). Trained independent assessors made ratings using the ABCD system.
Infant cognitive development. Infant cognitive development was assessed at 18 months in the research unit using the Mental Development Index of the Bayley Scales of Infant Development (Reference BayleyBayley, 1969).
Five-year outcomes
Child emotional and behavioural problems
-
(a) Maternal reports: at 5 years post-partum, mothers completed the self-report Rutter A2 Scale (Reference Rutter, Tizard and WhitmoreRutter et al, 1970); this is a reliable and well-validated questionnaire identifying child behaviour problems of clinical significance.
-
(b) Teacher reports: the children's teachers completed the Pre-school Behaviour Checklist (PBCL; Reference McGuire and RichmanMcGuire & Richman, 1988); this questionnaire has been widely used in research and has been found reliably to identify significant child behaviour problems in the context of pre-school and reception classes.
Child cognitive development. The McCarthy Scales of Children's Abilities (Reference McCarthyMcCarthy, 1972), a general measure of children's cognitive development, were administered in the research unit.
Data analysis
Initially, the effect of treatment on outcome was assessed. Generalised linear models were used to analyse the individual measures of the mother—child relationship and child outcome that were dichotomous or normally distributed, controlling for pre-treatment measures of the outcome variable where appropriate. The outcome measures that had distributions that were positively skewed were analysed using Kruskal—Wallis one-way analysis by ranks, and the median differences between the controls and each of the treated groups were calculated using the Hodges—Lehmann estimator. Further models were fitted to explore the effect of treatment after controlling for social adversity (which was possibly unbalanced between the treatment groups, as well as being thought to be related to outcome) and other potentially relevant baseline covariates: conflict concerning motherhood, maternal age (under age 25 years defined as young) and education (up to ‘O’ level or GCSE defined as low), the gender of the child and, for assessments at 4.5 months, the baseline Edinburgh Postnatal Depression Scale (EPDS; Reference Cox, Holden and SagovskyCox et al, 1987) score. Interactions between baseline covariates and treatments also were considered. Covariates and their interactions were retained in the model if they reached a significance of P<0.05. Linear regression was used to analyse maternal sensitivity, which was assumed to be normally distributed. The binary variables created for the measures of emotional and behavioural development, early problems in the mother—infant relationship and infant attachment were analysed using logistic regression. The adjusted odds ratios from the logistic regression models were converted to approximate relative risks using the method of Zhang & Yu (Reference Zhang and Yu1998), because the rates of depression were common (i.e. >10%; Reference Davies, Crombie and TavakoliDavies et al, 1998). The positively skewed distributions of the BSQ, Bayley, Rutter A2, PBCL and McCarthy scales were assumed to follow a gamma distribution.
A subgroup analysis for those women who had received therapy was conducted to investigate the effect of receiving treatment from a specialist as opposed to a non-specialist therapist.
All statistical analyses were performed using the SAS program package (version 8.02, SAS Institute, Cary, NC).
RESULTS
Four-month outcomes
Emotional and behavioural development
Early management of infant behaviour. As can be seen from Table 1, before treatment, in each of the four groups, around half of the women reported the presence of a moderate or marked difficulty with some area of infant behaviour. After the treatment period, of the women who had reported experiencing difficulty before treatment, just under half of those in the non-directive counselling, CBT and control groups still reported a problem. More women in the psychodynamic therapy group continued to experience difficulties after treatment. A logistic regression of behavioural management problems at 4.5 months revealed there to be no treatment effects after controlling for the significant effect of reported problems prior to treatment (see Table 2). Furthermore, after controlling for the presence of social adversity and baseline EPDS scores, the treatment effects still were found to be non-significant.
Table 1 Maternal reports of problems
| Assessment | Treatment group | n | Reporting problems before therapy | Still reporting problems after therapy (having reported a problem before therapy) | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | % difference1 | 95% CI | |||
| Behaviour-management problems | Control | 31 | 18 | 58 | 8 | 44 | ||
| Counselling | 40 | 19 | 47 | 9 | 47 | -3 | -35 to 29 | |
| Psychodynamic | 40 | 22 | 55 | 15 | 68 | -24 | -54 to 6 | |
| Cognitive—behavioural | 41 | 22 | 54 | 9 | 41 | 3 | -28 to 34 | |
| Relationship problems | Control | 31 | 23 | 74 | 19 | 83 | ||
| Counselling | 40 | 25 | 63 | 18 | 72 | 11 | -12 to 34 | |
| Psychodynamic | 40 | 24 | 60 | 12 | 50 | 33 | 8 to 58 | |
| Cognitive—behavioural | 41 | 29 | 71 | 12 | 41 | 42 | -18 to 66 | |
Table 2 Estimates of treatment effects
| Timing of assessment | Outcome variable | Treatment group | n | Per cent with adverse outcome | Model estimates | ||
|---|---|---|---|---|---|---|---|
| Relative risk | P | 95% CI | |||||
| 4 months | Behaviour-management problems1 | Control | 35 | 37 | |||
| Counselling | 43 | 35 | 0.91 | 0.77 | 0.42-1.58 | ||
| Psychodynamic | 43 | 44 | 1.21 | 0.52 | 0.62-1.87 | ||
| Cognitive—behavioural | 41 | 32 | 0.83 | 0.60 | 0.37-1.50 | ||
| Relationship problems2 | Control | 35 | 74 | ||||
| Counselling | 43 | 53 | 0.63 | 0.03 | 0.32-0.97 | ||
| Psychodynamic | 43 | 47 | 0.57 | 0.01 | 0.28-0.92 | ||
| Cognitive—behavioural | 41 | 39 | 0.46 | 0.002 | 0.20-0.81 | ||
| 18 months | Infant attachment3 | Control | 47 | 43 | |||
| Counselling | 39 | 41 | 0.96 | 0.89 | 0.54-1.46 | ||
| Psychodynamic | 40 | 52 | 1.23 | 0.86 | 0.76-1.68 | ||
| Cognitive—behavioural | 41 | 54 | 1.26 | 0.30 | 0.78-1.70 | ||
Early problems in the mother—infant relationship. Before therapy, the percentage of women reporting moderate or marked relationship problems (60-74%) was higher than the percentage reporting behavioural difficulties (see Table 1). After therapy, the percentage of women who were still experiencing relationship difficulties varied between the groups, with far fewer women in the control group reporting that they had resolved their relationship difficulties.
All three treatments were found to reduce significantly the risk of reporting a moderate or marked relationship problem, after the effect of reported pre-treatment relationship problems had been controlled for (see Table 2). The decreased risk associated with treatment remained after social adversity had been controlled for.
Mother—infant interactions
Mother—infant face-to-face interactions were assessed using the measure of maternal sensitivity at 2 and 4.5 months post-partum. From Fig. 1, it can be seen that for all groups the levels of maternal sensitivity increased to a comparable extent. In a regression analysis, the three treatments were found to be comparable with the control condition after the level of maternal sensitivity at 2 months had been controlled for. A secondary analysis that included the main effects of treatment and level of social adversity, along with their interaction (see Table 3), revealed that for women with low levels of social adversity those in the control condition had higher levels of sensitivity than women in the CBT or psychodynamic therapy groups. The effects were estimated as -0.46 for CBT (95% CI -0.76 to -0.15; χ2=8.56; d.f.=1; P=0.003) and -0.39 for psychodynamic therapy (95% CI -0.68 to -0.11; χ2=7.26; d.f.=1; P=0.007). No significant difference was found between the control condition and non-directive counselling (-0.23, 95% CI -0.53 to 0.07; χ2=2.21; d.f.=1; P=0.14). For women with high social adversity, those who received non-directive counselling were found to have higher levels of maternal sensitivity than the women in the control condition (0.46; 95% CI -0.03 to 0.89; χ2=4.36; d.f.=1; P=0.04). There were found to be no treatment effects for CBT (0.07; 95% CI -0.78 to 0.23; χ2=1.14; d.f.=1; P=0.29) or psychodynamic therapy (0.09; 95% CI -0.25 to 0.95; χ2=1.33; d.f.=1; P=0.25).
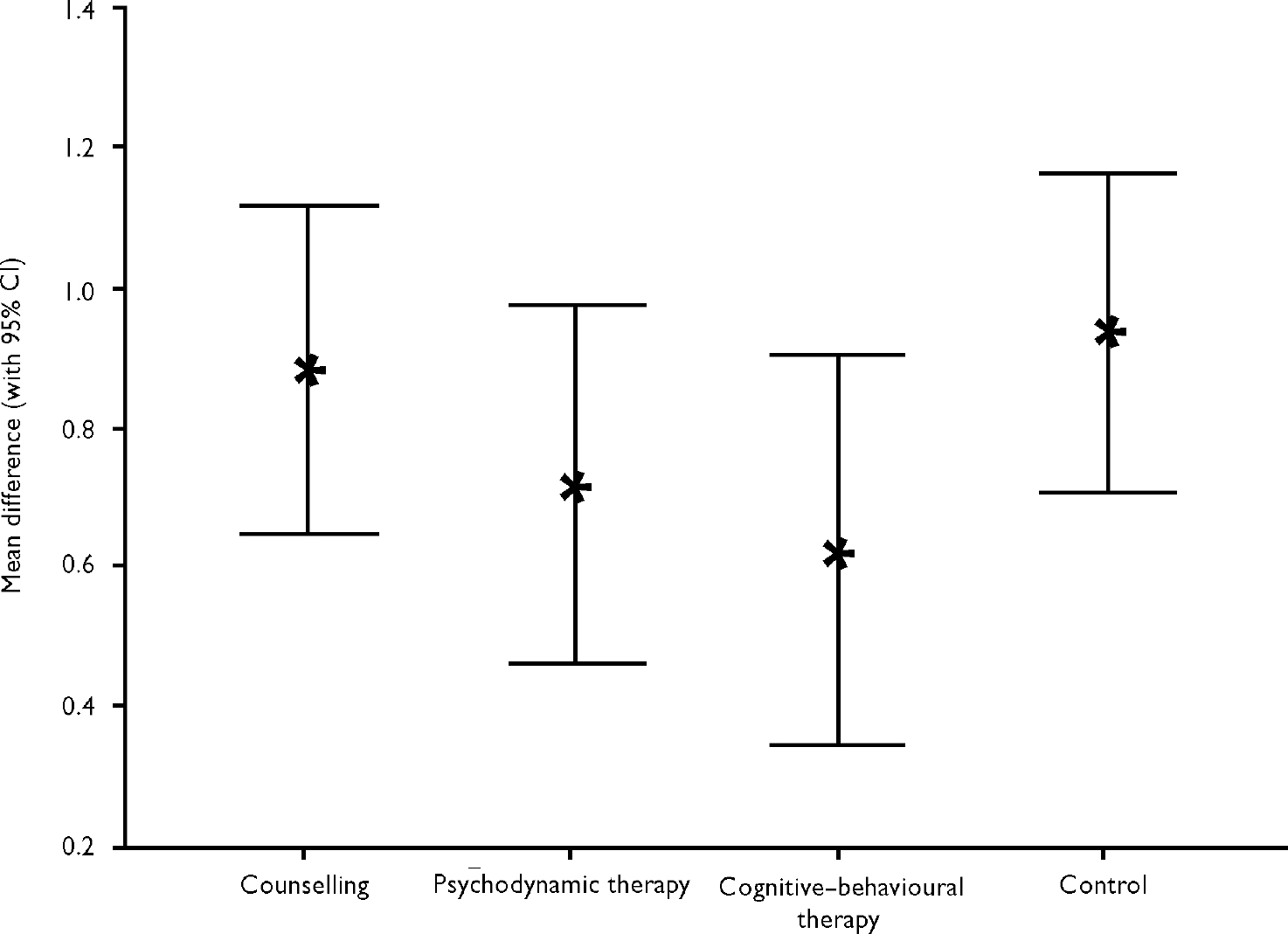
Fig. 1 Mean difference in maternal sensitivity: maternal sensitivity at 4.5 months minus maternal sensitivity before therapy.
Table 3 Estimates for models of maternal sensitivity
| Variable | Model estimates | |||
|---|---|---|---|---|
| Parameter estimate | s.e. | P | 95% CI | |
| Intercept | 2.79 | 0.19 | 2.4 to 3.16 | |
| Maternal sensitivity at 2 months | 0.24 | 0.07 | 0.001 | 0.1 to 0.39 |
| Counselling | -0.23 | 0.15 | 0.14 | -0.53 to 0.07 |
| Psychodynamic therapy | -0.39 | 0.15 | 0.007 | -0.68 to -0.11 |
| Cognitive—behavioural therapy | -0.46 | 0.16 | 0.003 | -0.76 to -0.15 |
| Social adversity | -0.91 | 0.19 | <0.0001 | -1.27 to -0.54 |
| Social adversity × counselling | 0.69 | 0.27 | 0.01 | 0.16 to 1.22 |
| Social adversity × psychodynamic | 0.04 | 0.34 | 0.19 | -0.63 to 0.71 |
| Social adversity × CBT | 0.73 | 0.30 | 0.02 | 0.14 to 1.33 |
Eighteen-month outcomes
Later infant emotional and behavioural problems
At 18 months post-partum the BSQ was administered to the mothers as an interview. The BSQ scores showed an indication of the difference between the groups (Kruskal—Wallis=9.04; d.f.=3; P=0.03). The median differences show that the infants of control mothers tended to score higher than those of mothers in any of the three treatments (see Table 4). A generalised linear model was fitted, which assumed that the BSQ scores followed a gamma distribution. Compared with the control group, after controlling for social adversity and the significant effect of maternal age, the effect of treatment was significant for non-directive counselling (χ2=12.19; d.f.=1; P=0.001), with the psychodynamic therapy and CBT conditions also showing some indication of an improvement compared with the control condition (χ2=4.06, d.f.=1, P=0.03 and χ2=3.52, d.f.=1, P=0.06, respectively). Younger women (under 25 years) reported more problematic behaviour in their infants than did older women (χ2=3.84; d.f.=1; P=0.05). For younger women, the increased BSQ expected scores were estimated to be: 4.5 (95% CI 3.4-6.3) for non-directive counselling, 5.7 (95% CI 4.4-7.9) for psychodynamic therapy, 6.1 (95% CI 4.7-8.4) for CBT and 8.3 (95% CI 6.2-12.2) for controls. For women aged 25 years and over, the expected BSQ scores were estimated to be 3.7 for the non-directive counselling group (95% CI 3.0-4.7), 4.6 for the psychodynamic therapy group (95% CI 3.8-5.8), 4.9 for the CBT group (95% CI 4.0-6.1) and 6.3 for the control group (95% CI 5.1-8.0).
Table 4 Summary statistics for the non-normally distributed outcome variables

| Timing of assessment | Outcome variable | Treatment group | n | Median | IQR | Range | Median difference | (95% CI) |
|---|---|---|---|---|---|---|---|---|
| 18 months | BSQ | Counselling | 46 | 4 | 3 | 0-11 | -2 | (-3 to -1) |
| Psychodynamic | 42 | 4 | 5 | 0-11 | -1 | (-3 to 0) | ||
| Cognitive—behavioural | 42 | 5 | 4 | 0-13 | -1 | (-2 to 0) | ||
| Control | 48 | 6 | 3 | 1-15 | ||||
| Bayley scale | Counselling | 46 | 114 | 32 | 64-150 | -2 | (-11 to 6) | |
| Psychodynamic | 42 | 118 | 19 | 78-150 | 1 | (-6 to 7) | ||
| Cognitive—behavioural | 42 | 116 | 24 | 73-150 | 0 | (-7 to 7) | ||
| Control | 48 | 116 | 18 | 85-150 | ||||
| 5 years | Rutter A2 scale | Counselling | 33 | 9 | 7 | 3-33 | -1 | (-3 to 2) |
| Psychodynamic | 28 | 10 | 6 | 4-35 | 0 | (-3 to 3) | ||
| Cognitive—behavioural | 31 | 8 | 5 | 0-16 | -3 | (-5 to 0) | ||
| Control | 35 | 11 | 6 | 1-28 | ||||
| PBCL | Counselling | 26 | 3 | 6 | 0-14 | 0 | (-2 to 2) | |
| Psychodynamic | 28 | 4 | 4 | 0-12 | 0 | (-2 to 2) | ||
| Cognitive—behavioural | 29 | 4 | 5 | 0-11 | 0 | (-2 to 2) | ||
| Control | 33 | 3 | 4 | 0-24 | ||||
| McCarthy scale | Counselling | 33 | 107 | 22 | 54-148 | -1 | (-9 to 7) | |
| Psychodynamic | 32 | 108 | 11 | 50-125 | 0 | (-7 to 6) | ||
| Cognitive—behavioural | 35 | 111 | 21 | 69-145 | 2 | (-6 to 10) | ||
| Control | 39 | 108 | 17 | 50-140 |
Infant attachment
The rates of secure (B) and insecure (A, C and D) attachment were similar for all four groups and no significant differences were found between the treated groups and the control condition (see Table 2). After controlling for social adversity, the treatment effects remained insignificant.
Cognitive development
At 18 months post-partum, scores on the measure of child cognitive development, the Mental Development Index of the Bayley Scales (see Table 4), were similar for the four groups (Kruskal—Wallis=0.78; d.f.=3; P=0.85). A generalised linear model, which assumed that the scores followed a gamma distribution, revealed there to be no significant treatment effects after controlling for social adversity and the significant adverse effects of young maternal age (χ2=6.13; d.f.=1; P=0.01), low maternal education (χ2=7.67; d.f.=1; P=0.006) and male gender (χ2=7.73; d.f.=1; P=0.005).
Five-year outcomes
Emotional and behavioural difficulties
At 5 years, child emotional and behavioural difficulties were assessed using maternal reports on the Rutter A2 Scale and teacher reports on the PBCL. The distribution of the Rutter A2 Scale scores was found not to differ between the four groups (Kruskal—Wallis=7.19; d.f.=3; P=0.07). However, there was some evidence from the median differences (see Table 4) that infants whose mothers had received CBT had lower scores compared with the infants of control mothers. A generalised linear model was fitted that assumed that the Rutter A2 Scale scores followed a gamma distribution. After controlling for the significant adverse effect of social adversity (χ2=9.55; d.f.=1; P=0.002), only an indication of a CBT treatment effect was found (χ2=3.61; d.f.=1; P=0.06). For women who did not experience a high level of social adversity, the mean Rutter A2 Scale scores were estimated to be 7.7 for the CBT group (95% CI 6.5-9.4), 9.5 for the non-directive counselling group (95% CI 8.0-11.6), 9.8 for the control group (95% CI 8.2-12.0) and 11.2 for the psychodynamic therapy group (95% CI 9.4-13.8). For women who had a high level of social adversity, the Rutter A2 Scale scores were estimated to be 10.2 for the CBT group (95% CI 7.8-14.4), 13.4 for the non-directive counselling group (95% CI 10.7-17.7), 13.9 for the controls (95% CI 11.1-18.6) and 16.8 for the psychodynamic therapy group (95% CI 12.1-26.5).
The distribution of scores on the teacher reports of child behavioural difficulties (PBCL), treated as a continuous measure (see Table 4), did not differ between the four groups (Kruskal—Wallis=0.10; d.f.=3; P=0.99). A generalised linear model, which assumed that the scores followed a gamma distribution, revealed there to be no significant treatment effects after controlling for the level of social adversity.
Cognitive development
At 5 years post-partum, scores on the measure of child cognitive development, the General Cognitive Index of the McCarthy Scales (see Table 4), similarly failed to differ between the four groups (Kruskal—Wallis=0.55; d.f.=3; P=0.91). A generalised linear model, which assumed that the scores followed a gamma distribution, showed no significant treatment effects after controlling for social adversity and the adverse effects of antenatal motherhood issues (χ2=3.60; d.f.=1; P=0.06) and a low level of maternal education (χ2=8.61; d.f.=1; P=0.003).
Specialist therapist effects
After controlling for pre-treatment measures, at 4 months there were found to be no specialist therapist effects for behavioural problems (relative risk=1.34; P=0.24; 95% CI 0.80-1.91), relationship problems (relative risk=1.23; P=0.36; 95% CI 0.76-1.68) or maternal sensitivity (specialist effect=-0.18; P=0.15; 95% CI-0.42 to 0.07).
At 18 months, specialists and non-specialists were found not to differ for BSQ score (median difference=0; P=0.82; 95% CI -1 to 1) or attachment (relative risk=0.97; P=0.90; 95% CI 0.61-1.36). Infants of mothers receiving treatment by specialists were found to have higher Bayley scores (median difference=14, P=0.0001; 95% CI 7-21).
At 5 years, no specialist effect was found for Rutter A2 (median difference=-1; P=0.18; 95% CI -3 to 1) or PBCL scores (median difference=0; P=0.92; 95% CI -1 to 2). Children of mothers receiving treatment by specialists were found to have higher McCarthy scores (median difference=10; P=0.002; 95% CI 4-15).
DISCUSSION
Mother—infant interventions
There has been a considerable volume of research to determine the effectiveness of interventions for difficulties in the mother—infant relationship in general (van Ijzendoorn et al, 1995; Reference FonagyFonagy, 1998; Reference Barlow and Stewart-BrownBarlow & Stewart-Brown, 2000). Few studies, however, have focused on samples of mothers with depression (Reference Lyons-Ruth, Connell and GrunebaumLyons-Ruth et al, 1990; Reference Gelfand, Teti and SeinerGelfand et al, 1996; Reference Cichetti, Rogosch and TothCichetti et al, 2000), and none has focused on post-partum samples.
Different treatment approaches
Clinical practice that deals specifically with the mother—infant relationship has developed into two distinct lines of work: (a) cognitive—behavioural approaches with an emphasis on ‘here and now’ observed behaviour and difficulties, at times combined with a problem-solving approach, aim to promote maternal feelings of competence in infant caretaking as well as to improve maternal sensitivity and the quality of mother—infant interactions, for example, through modelling or positive feedback (Reference Gelfand, Teti and SeinerGelfand et al, 1996; Reference Field, Murray and CooperField, 1997); and (b) psychodynamic approaches focus on the mother—infant relationship in terms of the mother's past history of relationships as the source of current problems (e.g. Reference FraibergFraiberg, 1981; Reference Cramer, Robert-Tissot and SternCramer et al, 1990). Theoretically, the mother's history of relationships is particularly relevant to the infant's developing attachment to the mother because it deals with the mother's representation of her own early attachment relationships — itself a strong predictor of infant attachment quality (Reference van Izendoorn, Juffer and Duyvesteynvan Izendoorn et al, 1995; Reference Steele, Steele and FonagySteele et al, 1996). Nevertheless, in studies aimed at preventing the development of insecure attachments, the modest positive results that have been achieved have come from short-term behaviourally focused treatments rather than from more intensive, long-term therapies working at the level of maternal representations (van Ijzendoorn et al, 1995). This is important because establishing whether different treatments are differentially effective not only is theoretically interesting but also has significant practical implications in terms of the skills, and therefore personnel and National Health Service resources, required to deliver the intervention. Any treatment that demands a high level of training in psychotherapy, and particularly psychodynamic work, will be limited in its availability. However, important practical implications would follow if it were shown that treatments deliverable by health visitors, found to be effective in bringing about early remission from depression (e.g. counselling), were also of benefit in terms of the mother—infant relationship and child development.
The current study
The current study addressed these questions by evaluating the impact of three brief psychological treatments, delivered in the home from 8 to 18 weeks post-partum, to a representative community sample of primiparous mothers with postnatal depresion. The study therapists included health visitors who received training in the CBT and counselling treatments, as well as specialist professional therapists representing each of the three treatment approaches. Assessments were made of the child's behavioural, emotional and cognitive development through infancy and at 5 years. The three study treatments — non-directive counselling, CBT and psychodynamic therapy — were found to bring about an early improvement in the EPDS measure of maternal mood (see Reference Cooper, Murray and WilsonCooper et al, 2003, this issue).
Findings of the current study
Positive findings
Treatment showed some short-term benefits in relation to the mother—child relationship and child outcome. First, at 4.5 months, compared with those who received routine primary care, mothers who received any of the interventions reported significantly fewer difficulties in their relationship with their infant, experiencing play, separation issues and the management of the infant's needs for their attention as being less problematic. In addition, in mothers who experienced social adversity, whose interactions with their infants were particularly poor, non-directive counselling produced a more sensitive pattern of mother—infant interactions than was apparent among those in the control group. There was evidence also of a positive benefit of non-directive counselling at 18 months in terms of maternal reports of infant emotional and behavioural problems, and some indication also of a possible benefit for the other two treatments.
It is worth noting that the outcomes that showed the clearest evidence for a beneficial effect of treatment (i.e. relationship problems at 4.5 months and emotional and behavioural problems at 18 months) were those that relied on maternal reports.
Negative findings
The majority of outcomes failed to show any benefit of the study interventions. The first concerned the mother's experience, immediately after treatment, of difficulties in the practical management of her infant (sleeping, feeding and crying problems), where there was a similar level of improvement over time for both the control and the treated groups. There are a number of possible explanations for this lack of treatment effect. First, it is possible that any initial problems the mothers experienced with their infants resolved spontaneously over time. This is particularly likely to be the case with crying problems. The peak age for persistent crying in UK populations is between 3 and 6 weeks, with a steady decline in the amount of time that infants cry thereafter (Reference St James-Roberts and PlewisSt James-Roberts & Plewis, 1996). By 4.5 months, when the first post-treatment assessment was made, it is likely that infant crying would have shown a significant spontaneous decline. Initial feeding problems also are likely to have settled down by this time. An alternative explanation is that the routine care provided by health visitors was effective in these particular areas of infant behaviour. The principal focus of routine health visiting is advice on the practical difficulties that women experience in the management of such infant problems, and it may be that in these particular respects the study interventions offered no significant advantage over routine health visitor practice.
With regard to infant attachment also there was no benefit of any of the treatments compared with the control condition. Influencing the nature of child attachment to the mother has generally proved difficult to achieve, even in samples without depression. A meta-analysis by van Ijzendoorn et al (1995) showed the overall effect size for 12 treatment studies to be only 0.17; and a subsequent study by Gelfand et al (Reference Gelfand, Teti and Seiner1996) with a clinically referred depression sample showed that treatment conferred no benefit in terms of overall rates of child security of attachment. The fact that the current treatments were brief and delivered early on in development, before the setting up of clear attachment responses, may have made the promotion of security particularly difficult to achieve.
Finally, with regard to infant and child cognitive development and child emotional and behavioural adjustment at both home and school at 5 years, no significant benefit of any of the treatments was evident. The apparently negative finding regarding cognitive development should, possibly, be viewed with caution. Reports of significant adverse effects of postnatal depression on cognitive development have been derived generally from high-risk samples (e.g. Reference Lyons-Ruth, Zoll, Connell, Tronick and FieldLyons-Ruth et al, 1986; Reference Hay, Pawlby and SharpHay et al, 2001). In the current study sample, drawn from a relatively low-risk population, the children's IQ scores at 18 months and 5 years among both controls and treated groups were within the range expected for a general population sample, and thus it can be argued that the issue of treatment preventing cognitive deficits did not obtain. This same argument cannot be made in relation to child emotional and behavioural adjustment: in this domain, adverse outcome in terms of increased rates of both internalising and externalising problems have been found to be associated with postnatal depression in low-risk as well as high-risk samples (Reference Sinclair and MurraySinclair & Murray, 1998; Reference Murray, Sinclair and CooperMurray et al, 1999; Reference Essex, Klein and MiechEssex et al, 2001). It appears, therefore, that although the intervention may have been of some benefit to the early mother—infant relationship and to the emotional and behavioural adjustment of the infant at 18 months, this benefit did not persist.
The question of whether treatment delivered by specialist therapists would be of greater benefit than that provided by non-specialists (including trained health visitors) was addressed in the current study. For none of the outcomes showing a significant benefit of treatment was there a difference between specialists and non-specialists. With regard to the other outcomes, an expertise effect was apparent only for cognitive performance (Bayley and McCarthy scales). The case for an overall benefit of specialist therapists is therefore not substantial.
Clinical implications
The fact that only limited, short-term benefits to the mother—infant relationships and child development accrued from the interventions suggests that, despite symptomatic improvement and initial gains in maternal care, underlying maternal vulnerabilities persisted. In order to prevent longer-term difficulties in child functioning, therefore, more-prolonged interventions may be required. Nevertheless, such treatment may not require high-level psychological expertise. Thus, we found no substantial evidence that specialist therapists were more effective than non-specialists; and although the study was not designed to compare the three interventions with each other, the clearest evidence to emerge for a benefit of treatment compared with routine care was for the counselling condition. On both these counts, as well as for reasons of availability and cost, health visitors appear to be well-placed to deliver such support.
Two further clinical implications of the current study should be noted. First, although the treatments were, in general, highly acceptable to the women concerned, a minority of mothers were reluctant to receive the home visiting support. Inspection of the outcomes and background characteristics of those refusing such interventions indicates that this population may be particularly at risk (Reference Murray, Woolgar and MurrayMurray et al, 2003). Related research suggests that forging positive relationships with those who may be distrustful of established professional services is a key therapeutic challenge that may be resolved ultimately only through the use of non-statutory volunteer or community support routes (Reference Egeland and EricksonEgeland & Erickson, 1990; Reference Harris, Brown and RobinsonHarris et al, 2000). Second, any intervention that is delivered only when women have already become depressed falls short of ideal practice. To date, studies aiming to prevent depression have, by and large, been unsuccessful, not least because take-up rates by vulnerable women have been poor (Reference Stamp, Williams and CrowtherStamp et al, 1995; Reference Buist, Westley and HillBuist et al, 1999; Reference Brugha, Wheatley and TaubBrugha et al, 2000; Reference Elliott, Leverton and SanjackElliott et al, 2000). The development and evaluation of preventive interventions therefore represents a further major challenge for researchers engaged in this clinical area.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Brief home-based psychological interventions are effective in significantly elevating mood in women with post-partum depression.
-
▪ Such interventions also bring about short-term improvement in some aspects of the early mother—infant relationship and child outcomes.
-
▪ Health visitors are effective in delivering home-based intervention to women in the post-partum period, and their training and practice should be extended to encompass the detection and management of mothers with postnatal depression.
LIMITATIONS
-
▪ The sample was one that was generally at low risk, and comprised only primiparous mothers; the generalisability of the findings to high-risk and multiparous populations is uncertain.
-
▪ The sample was underpowered to detect differences between the treatment groups.
-
▪ Although the efficacy of the interventions has been demonstrated for some outcomes, effectiveness studies are required to establish whether such benefits would be obtained in routine practice.
Acknowledgements
We are indebted to all the women and children who took part in this study. This research was carried out within the Cambridge University Department of Psychiatry. The initial trial was supported by a grant from Birthright. The 5-year follow-up was supported by the Medical Research Council. We are grateful to Angela Cameron, Sian Coker, Jenny Corrigal, Bridget Halnan, Sheelah Seeley and Claire Wilson for their help with carrying out the treatments, to Jill Butler, Janet Edwards, Alison Hipwell and Agnese Fiori-Cowley for their help with the assessments and to Matt Woolgar for his comments on the manuscript.








eLetters
No eLetters have been published for this article.