Introduction
The Coronavirus disease 2019 (COVID-19) is spreading rapidly throughout the world. By 9 September 2020, 27,784,361 people have been infected by COVID-19; moreover, 902,762 of these patients have died. 1 Lung is the primary organ which the COVID-19 virus affects and leads to pneumonia, an acute respiratory distress syndrome (ARDS). In ARDS patients, overexpression of pro-inflammatory cytokines, such as interleukin, and macrophage inflammatory protein have been seen. This process is called ‘cytokine storm’. 1 COVID-19 infects the lower respiratory system, and the lung’s response to this infection is recruiting macrophages and monocytes leading to inflammation, this response causes widespread damage to the lung’s airways. Reference Liu, Li and Liu2
Activating cytokines leads to the migration of macrophages and monocytes to parts of lung infected with the COVID-19 virus. Endothelial cells play a key role in the inflammation process. After irradiating these cells with low radiation doses (0.01–2 Gy), the monocyte adhesion is significantly enhanced, and the mechanism of this phenomenon activates tumor necrosis factor-α after irradiation. Reference Tay, Poh, Rénia, MacAry and Ng3
For mammalian cells, hyper-radiosensitivity and induced radioresistance are determined below 0.3 Gy and in the dose range of 0.3 Gy to 0.6 Gy, respectively. Reference Schröder, Kriesen, Paape, Hildebrandt and Manda4 In our study, investigations on using low-dose radiation as a treatment for COVID-19 were evaluated, eventually these studies were compared with risk of lung cancer during performed dose for the treatment of COVID-19 in radiation therapy.
In this paper, we review the available literature on the use of low-dose radiation in improving inflammation and pneumonia. Hence, in vivo and in vitro studies evaluating the anti-inflammatory effects of low-dose radiation on different cell lines and animals, as well as twelve recent clinical studies, in which the effects of low-dose radiotherapy in the treatment of patients with coronavirus disease has been evaluated. The results of most of these clinical studies have not yet been published. Published paper for this literature review were identified by searching PubMed database from 1940 onwards with the following Medical Subject Heading terms ‘pneumonia’, ‘COVID-19’, ‘coronavirus’, ‘inflammation, ‘low dose Radiotherapy’. Articles in English language were reviewed.
In vivo and In vitro Studies
The anti-inflammatory effect of radiation on the lungs is through modulation of cytokine and adhesion molecule expression on activated endothelial cells and leukocytes and on nitric oxide (NO) production and oxidative burst in activated macrophages and native granulocytes. The highest efficiency was reported at doses of 0.3–0.7 Gy. Reference Rödel, Keilholz, Herrmann, Sauer and Hildebrandt6
In addition, the in vitro studies suggest that low-dose radiation therapy (LD-RT) has a potent anti-inflammatory effect, inhibiting leukocyte–endothelium interactions at doses <0.7 Gy. In contrast, inflammatory and degenerative bone diseases in humans are treated with doses ranging from 0.3 to 1.5 Gy. Thus, using lower doses in the range 0.1–0.3 Gy could maximise anti-inflammatory effects and minimise toxicity. Reference Rodel, Frey and Gaipl5
In vivo studies indicated that the effects of LD-RT on decreasing inflammation are realised by the effects of these radiations on endothelial cells, mononuclear cells and macrophages. The doses used in these studies were in the range of 0.3–1 Gy. Studies on animals whose lungs have been directly affected by bacterial and viral pneumonia have indicated that low-dose application has been able to significantly decrease mortality in animals that received low doses in one fraction in comparison to those which did not receive the dose. Reference Lieberman, Hodes and Leopold8–Reference Baylin, Dubin and Gobbel11
The Effects of Low-Dose Radiation on the Immune System
The effects of low-dose radiation (above or below 1 Gy) on the immune system are controversial. Animal studies show that low-dose irradiation (more than 1 Gy) may lead to immunosuppression. Doses above 1 Gy result in deficiency of haematopoietic stem cells, accelerated cell cycling of bone marrow precursors, decreased cell viability of mature blood cells and suppression of blood leukocyte levels. Reference Yagunov, Tokalov, Chukhlovin and Afanassiev12,Reference Seed, Inal and Dobson13 Blood samples of radiology workers ranging from 21 to 57 years who are exposed to long-term low ‘dose reveal that some immunological parameters such as levels of T lymphocytes, IgA, IgG and IgM are decreased. Reference Godekmerdan, Ozden, Ayar, Gursu, Ozan and Serhatlioglu14
Single fraction or chronic low dose with total doses below 1 Gy has been performed recently. The results show that low doses 0.5 or 1 Gy to dendritic cells (DCs) have not had significant effects on dendritic cells cytokine release and T cell proliferation. Reference Jahns, Anderegg and Saalbach15 Irradiation of dendritic cell at 0.02–1.0 Gy shows that the highest proliferation capacity of T cells occurs at 0.05 Gy through released cytokine by dendritic cells. In contrast, this range of irradiated dose has not had any effects on the maturation of dendritic cells. Reference Shigematsu, Adachi and Koike-Kiriyama16
Clinical Aspects of Low-dose Radiation
The use of Roentgen rays with a dose of 100–150 Roentgen in the treatment of pneumonia in children has been studied long time ago. The results indicated that the use of this radiation in low doses can be effective in the treatment of this disease. Reference Oppenheimer17 The application of ionising radiation in the treatment of pneumonia has been studied since the beginning of the last century. The results of this study showed that the use of low doses was able to decrease mortality in these patients like other methods including serum therapy and drug treatments. The use of low doses with a mean of 50 Roentgen has been effective in the treatment of most patients suffering from pneumonia. Reference Calabrese and Dhawan18 In some countries, such as Germany, low-dose radiotherapy is applied as an acceptable remedy method for the treatment of nonmalignant diseases such as inflammatory, degenerative, hyperproliferative, functional and vascular diseases. Reference Seegenschmiedt, Micke and Willich19
The results of in vitro study of human lung tissue against 0.5–1 Gy radiation showed that this low dose could significantly decrease the secretion of interferon-gamma and increase the secretion of interleukin-10 in comparison to the control group that did not receive a dose. Thus, this series of events leads to the stimulation of macrophages in the lung tissue. The overall results of this study indicated that low doses could stimulate macrophages for eliminating tissue inflammation. Reference Meziani, Robert, Mordant and Deutsch20
Suggested Dose for COVID-19
The mentioned articles suggested different low doses for the treatment of pneumonia resulting from COVID-19. It was recently suggested that LDRT with a single acutely delivered dose to the lungs of 0.3–1 Gy of low-linear energy transfer radiation could be used to treat COVID-19 pneumonia with very low risk and avoiding normal tissue toxicities, this report is proposed 0.1 Gy or 0.07–2 Gy to the chest region for COVID-19-related pneumonia. This value of dose is derived from the historical use of ionising radiation for pneumonia. Reference Kirkby and Mackenzie21
It was also suggested that a priming dose with a few mGy followed by a single dose of 0.1, 0.18 or 0.25 Gy could be used to treat COVID-19 pneumonia. A dose of 0.25 Gy was selected because it is lower than the maximum dose of 0.26 Gy/year from natural background radiation in Ramsar, Iran. This background dose in Ramsar is much higher than the global average; however, doctors in the area have not reported an increase in the incidence of cancers such as leukaemia. In addition, there was no significant difference in haematological parameters such as red and white blood cell counts, mean corpuscular volume and mean platelet volume in individuals living in this area compared to areas that received a much lower dose than Ramsar. Therefore, it is recommended to use doses higher than 0.3 Gy for the anti-inflammatory effects of radiation with low doses in order to be effective. Reference Ghadimi-Moghadam, Haghani and Bevelacqua22,Reference Ghiassi-Nejad, Mortazavi, Cameron, Niroomand-Rad and Karam23
Current Studies on Human for COVID-19
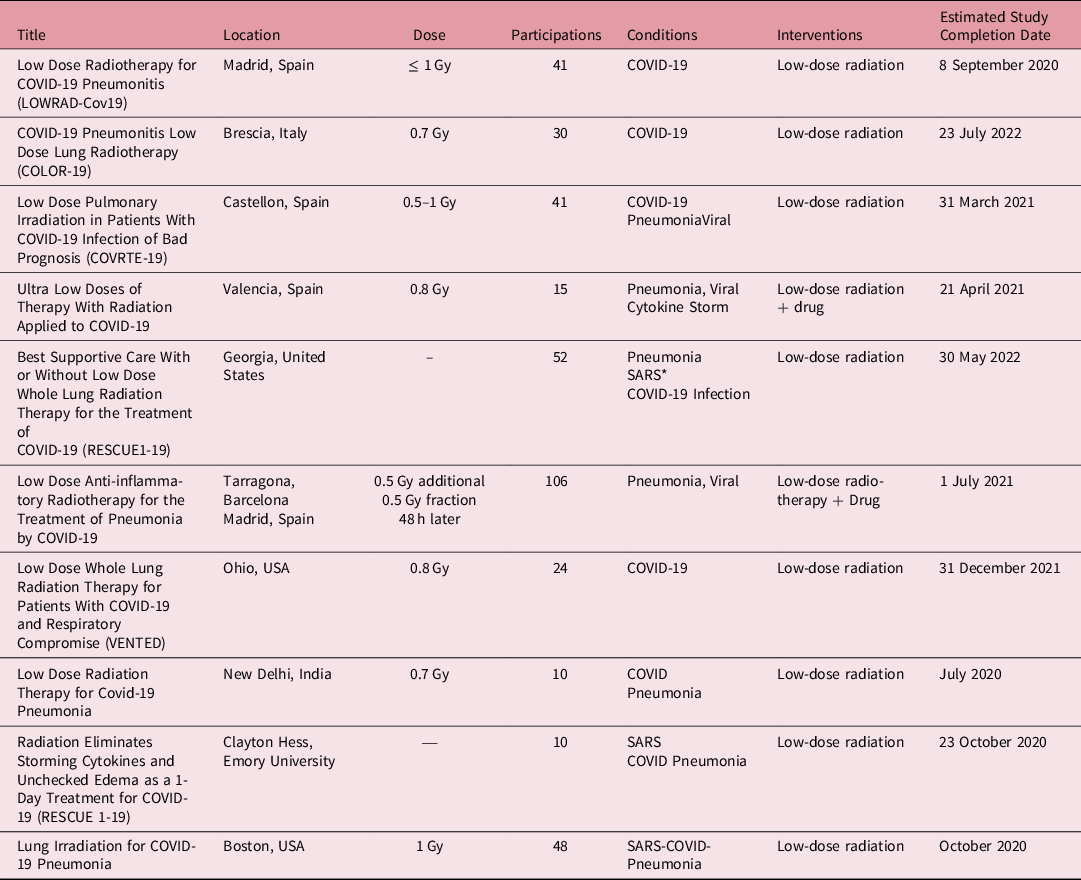
Currently, 12 different groups throughout the world are applying low doses in the treatment of COVID-19 in humans; however, 10 of these studies are not over yet. Table 1 summarises these studies. In these studies, after lung radiation with the recommended doses, patients are followed up; moreover, their results are evaluated in both primary and secondary outcomes. Primary outcomes related to the measurement of blood oxygen level, PaO2/FiO2 ratio (the ratio of arterial oxygen partial pressure to fractional inspired oxygen) and chest x-ray are in the period of one day to two weeks after radiation. Secondary outcomes included measurements of hospitalisation, day free of assisted mechanical aspiration, mortality are from a few weeks to a few months after irradiation. 24
Table 1. Studies are applying low doses in the treatment of COVID-19 in humans (*Severe Acute Respiratory Syndrome)
A clinical study was recently carried out on five patients with COVID-19 in the age range of 64–96 years, in which the patients’ lungs were exposed to 1.5 Gy of radiation in one fraction for 10–15 minutes. In four patients in the first 24 hours of exposure, their respiratory condition was quickly improved. The results of blood tests and imaging also confirmed the positive effect of low-dose radiation on COVID-19 treatment. Reference Hess, Buchwald and Stokes25
Another study of five patients with COVID-19 aged over 60 years who underwent national COVID-19 therapy protocols showed that using 0.5 Gy of radiation in one fraction led to the improvement of four patients in the first few days after exposure. In addition, they were discharged from the hospital with an average of 6 days, and no radiation toxicity was observed in these patients. Reference Ameri, Rahnama and Bozorgmehr26
Lung Cancer Risk Resulted from Radiation Therapy
According to articles previously published or are presently being published, the recommended dose for the treatment of COVID-19 pneumonia is in the range of 0.3–1.5 Gy; however, it is one of the controversies surrounding the use of low-dose ionising radiation in the COVID-19 treatment that can be discussed is the incidence of cancers such as lung, oesophagus and breast cancer.
Based on the present study, using BEIR VII model to estimate the risk of lung cancer at 0.5 Gy for patients with coronavirus disease aged 25, 45, 65 years and treated by low-dose radiation, the incidence of lung cancer can increase by 2.1%, 2.09% and 1.68%, respectively, for men, or almost three times for women. According to this model, with an increase in the dose received by the lungs, the risk of lung cancer increases linearly. Reference Kirsch, Diehn, Cucinoata and Weichselbaum27
Conclusion
A review of in vitro and in vivo studies showed that the use of low doses up to 1.5 Gy eliminates tissue inflammation and pneumonia by stimulating macrophages. Although completed clinical studies on the use of low doses in the treatment of COVID-19 are limited, the results of these studies have indicated that low-dose lung irradiation up to 80% has been effective in treating inflammation and pneumonia caused by COVID-19. The incidence risk of cancer resulting from ionising radiation may question the application of these radiations; nevertheless, calculations indicated that within the recommended dose range in clinical studies (up to 1 Gy), the risk of lung cancer did not remarkably increase. Since no definitive treatment has been found for COVID-19, it is recommended for patients with COVID-19 whose condition is deteriorating. Moreover, treatment protocols have not been able to help them. Thus, low-dose ionising radiation methods can be recommended to the patients and can make them aware of the risks of possible side effects from the radiation and the positive results that this method has had so far. It is hoped that ongoing clinical studies using this method will be completed as soon as possible, and their results will be positive in COVID-19 treatment.
Acknowledgements
None.
Financial Support
None.
Conflicts of Interest
None.






