The Zero Suicide framework in healthcare is a system-wide approach to care after a suicide attempt with the goal that no suicides should occur when a person is in contact with the health service.Reference Mokkenstorm, Kerkhof, Smit and Beekman1 It is predicated on seven elements: lead, train, identify, engage, treat, transition and improve. These elements of clinical care rely on systematic protocols that should involve ongoing risk screening and assessment, collaborative safety planning, access to evidence-based suicide-specific care, focus on lethal means reduction, consistent engagement efforts and support during high-risk periods.Reference Brodsky, Spruch-Feiner and Stanley2 The Zero Suicide framework has seen a rapid adoption, having been implemented in over 200 healthcare and behavioural health organisations worldwide by 2016.Reference Hogan and Grumet3 The Zero Suicide framework was substantially influenced by the Perfect Depression Care initiative,Reference Coffey4 of the Henry Ford Health System in Michigan, USA, which was shown to reduce the rate of deaths by suicide by 75% in the first 4 years of implementation.Reference Covington and Hogan5–Reference Hampton7 More recently, Centerstone in Tennessee reported a 65% reduction in the rate of deaths by suicide among patients treated for a variety of psychiatric conditions after implementing the Zero Suicide framework.Reference Hogan and Grumet3 However, initial evaluations have drawn criticism, owing to their observational nature, concerns about overstated outcomes and caution being expressed in comparing the Zero Suicide framework with the Perfect Depression Care model.Reference Coyne6,Reference Baker, Nicholas, Shand, Green and Christensen8 Despite the widespread rollout of Zero Suicide framework, there remains a lack of robust evidence for its effectiveness published internationallyReference Mokkenstorm, Kerkhof, Smit and Beekman1,Reference Coyne6 and we are not aware of any such research from Australia.
Implementation of the Zero Suicide framework at Gold Coast Mental Health and Specialist Services, Queensland, Australia
Although the Zero Suicide framework provides an overarching framework, it does not prescribe in detail the clinical components to be implemented. At Gold Coast Mental Health and Specialist Services (GCMHSS), a clinical suicide prevention pathway (SPP) based on Zero Suicide framework was rolled out in December 2016. Table 1 illustrates the tools and interventions comprising the SPP; they are listed in the order of their use following an individual's presentation to the hospital.
Table 1 Suicide prevention pathway (SPP) elements based on the Zero Suicide framework implemented at the Gold Coast Mental Health and Specialist Services
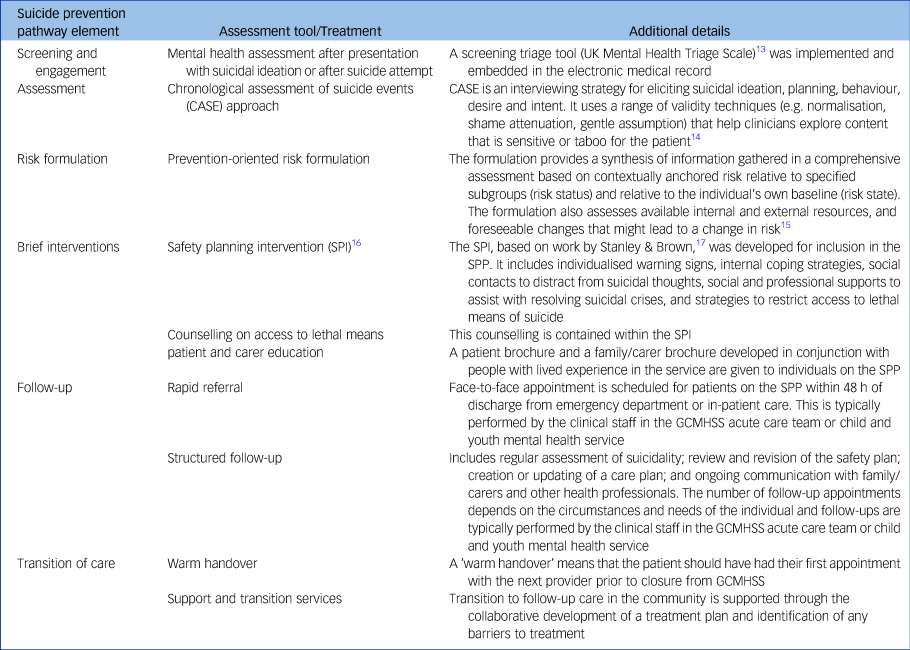
A concerted focus on training all GCMHSS clinical staff in the delivery of individual components of the SPP and developing attitudes, beliefs, confidence and skills in accord with the Zero Suicide framework, alongside a strong focus on cultural change and incorporation of Restorative Just Culture principles,Reference Dekker9 contributed to the rapid adoption of the new practices across GCMHSS.Reference Turner, Stapelberg, Sveticic and Dekker10
Reports on the Zero Suicide framework's efficacy have frequently focused on deaths by suicide. However, this metric has limitations as suicide deaths are relatively rare, making it challenging to ascribe statistical significance to clinically important associations or to build models that adequately consider possible confounders. Considering that a suicide attempt is one of the greatest risk factors for suicide completionReference Owens, Horrocks and House11 and that people with a suicide attempt share substantial clinical similarities with those who die by suicide,Reference Beautrais12 re-presentation with a suicide attempt provides an alternative outcome measure for suicide intervention studies.Reference Daigle, Pouliot, Chagnon, Greenfield and Mishara18,Reference Beautrais, Gibb, Faulkner and Mulder19
The aim of this paper is to report on the efficacy of the SPP with respect to reducing re-presentations with a suicide attempt following an initial attempt. As certain subgroups have an elevated risk of repeated suicide attempts, for example those with previous attemptsReference Beautrais20 or those diagnosed with borderline personality disorder,Reference Schneider, Wetterling, Sargk, Schneider, Schnabel and Maurer21,Reference Gunderson and Ridolfi22 the efficacy of the SPP with respect to these high-risk subgroups will be specifically explored.
A novel aspect to this work is that we embrace the fact that an individual may present with a suicide attempt multiple times. Traditional approaches limit analysis to the first subsequent event and either its occurrence within a certain time frame (relative risks or logistic regression models) or the time to that first subsequent event (e.g. Cox proportional hazards analysis). Limiting analysis to the first recurrent suicide attempt ignores both a considerable amount of information and the clinical nature of the attempt. However, recurrent events are by definition correlated, which violates the independence assumption required by traditional methods. A number of different statistical models have been developed for analysis of multiple event data. As this is a relatively new area of statistical analysis, there is no consensus on which may be the most appropriate for a given situation. In this paper, we present the results of six different models that we considered, a priori, to be suitable for analysis of suicide attempt events and use the consistency of their results to infer an appropriate model to predict suicide attempt recurrence. Although there is literature reporting time-to-event analyses with regard to first subsequent suicidal presentation or suicide,Reference Brent, Greenhill, Compton, Emslie, Wells and Walkup23,Reference Hawton, Zahl and Weatherall24 such studies are relatively uncommon, and we are unaware of other studies using time-to-recurrent-event analysis with respect to suicide attempts. However, the approach is highly relevant to suicide attempts in the evaluation of interventions that aim to delay time to re-presentation. Although novel with respect to analysis of repeated suicide attempts, time-to-recurrent-event analysis has been used in other areas of mental health research, such as self-harm.Reference Bennardi, McMahon, Corcoran, Griffin and Arensman25
Method
Context of the project
The Gold Coast Hospital and Health Service (GCHHS) is government-funded and serves approximately 560 000 people on the Gold Coast, Queensland, Australia. The GCHHS has two emergency departments and these are the most common access points for persons presenting with suicidal thoughts or behaviours. Gold Coast Mental Health and Specialist Services (GCMHSS) within GCHHS adopted the Zero Suicide framework in 2015.
Design
This project employs two designs, an initial observational cross-sectional design and a subsequent historical cohort design. In both cases re-presentation with a suicide attempt after a previous suicide attempt is the primary outcome.
Identification of suicide attempts
Presentations following a suicide attempt between 1 July and 31 December 2017 to GCHHS emergency departments were identified from the Emergency Department Information System (EDIS). A machine learning tool ‘Searching EDIS for Records of Suicidal Presentations’ (SERoSP)Reference Stapelberg, Sveticic, Hughes and Turner26 identified a total of 3417 suicidal and self-harm presentations. A team of trained research officers then reviewed the associated medical records contained in the Consumer Integrated Mental Health Application (CIMHA) and electronic medical record (eMR) to confirm suicide attempts. Cases were coded as a suicide attempt if they contained evidence of self-harming behaviour with intent to die, following literature-based definitionsReference De Leo, Burgis, Bertolote, Kerkhof and Bille-Brahe27 and the World Health Organization manual on surveillance and monitoring of suicide attempts and self-harm.28 This yielded 737 presentations with a suicide attempt, relating to 604 persons. An initial cross-sectional analysis investigated the relationship between being placed on the SPP and subsequent re-presentation with a suicide attempt within certain time frames.
For each of the 604 persons who presented with a suicide attempt between 1 July and 31 December 2017, all previous suicide attempt presentations since 1 January 2009 and subsequent suicide attempt presentations until 31 December 2018 were identified, providing a 10-year longitudinal history of suicide attempts for this cohort and including a total of 1534 suicide attempt presentations. This historical cohort data was used in a time-to-recurrent-event analysis. Analyses were based on presentations, rather than on individuals, as placement on the SPP related to a presentation rather than an individual and individuals may have presented with more than one suicide attempt within the observed time period.
Variables
For every suicide attempt event, it was recorded whether the person was placed on the SPP or not. Not all persons presenting to GCMHSS after a suicide attempt engaged with the SPP; reasons for not engaging typically included the individual declining follow-up care, residing outside the geographical catchment area or receiving follow-up from a different health service or private healthcare providers. In some cases, clinicians decide not to commence the SPP, for example owing to lack of familiarity with the protocol and confidence in the early phase of implementation, time pressures in the emergency department and clinical judgement about the likely benefits of placing someone on the SPP. Patients not commenced on the SPP after presentation with a suicide attempt may still receive certain components of the SPP and follow-up care (e.g. risk formulation, safety planning and telephone follow-up on discharge) but not the structured face-to-face follow-up that is mandated in the SPP.
Patients are typically placed on the SPP following the initial assessment by a mental health clinician in the emergency department or, when receiving in-patient care, during their admission. The date of discharge – either from emergency department or in-patient care – was considered as the starting point in the analysis of subsequent re-presentations with a suicide attempt within 7, 14, 30 or 90 days. The date of discharge was also considered when measuring the length of placement on the SPP for in-patients. On average, individuals were placed on the SPP for 15.6 days, with no significant difference in this duration between those admitted to in-patient care and those discharged following their emergency department presentation (Gold Coast Mental Health and Specialist Services, unpublished data. Note that due to strict confidentiality of this material we can not release any further details, apart from data vetted by our Ethics Committee and disseminated in peer-review publications.)
For each individual on the SPP, patient identification number, date and time of presentation, age, gender (male/female), Indigenous status (yes/no), triage notes, method of suicide attempt, destination after presentation to the emergency department (admitted to hospital for at least 24 h/discharged), and primary and secondary diagnoses according to the ICD-10-AM,29 were extracted from EDIS. Additionally, ICD diagnostic codes (F60–F69 ‘Disorders of adult personality and behaviour’, recorded as a primary or secondary diagnosis) at any engagement with GCMHSS were used to identify persons with personality disorders.
Statistical analysis
Descriptive statistics were used for demographic and clinical data of the person associated with each presentation. Comparisons were made between the characteristics of presentations that led to the person being placed, or not placed, on the SPP. The chi-squared (χ2) test, Fisher's exact test or t-test were used as appropriate. Re-presentation proportions within 7, 14, 30 and 90 days were compared between initial presentations associated with being placed on the SPP or not. Relative risks and their 95% confidence intervals were calculated. All analyses were performed using Microsoft Excel and Stata 15 for Windows.
Time-to-recurrent-event analyses
Time-to-recurrent-event analyses were conducted in which suicide attempt was modelled as a recurrent event for all suicide attempt presentations from 1 January 2009 to 31 December 2018, associated with the 604 persons who presented with a suicide attempt between 1 July 2017 and 31 December 2017.
As there is no consensus on the most appropriate method for modelling recurrent events,Reference Amorim and Cai30–Reference Schukken, Bar, Hertl and Gröhn32 six models were used: (a) the Anderson–Gill counting process (AG–CP); (b) Prentice–Williams–Petersen total time (PWP–TT); (c) Prentice–Williams–Petersen gap time (PWP–GT); (d) Weibull gamma shared frailty (shared frailty); (e) multilevel mixed effects parametric (mixed effects); and (6) Cox proportional hazards shared frailty (Cox shared frailty). Details of these models and the rationale for using a variety of models are provided in the supplementary material, available at https://doi.org/10.1192/bjp.2020.190.
The predictor variable of primary interest was the person being placed on the SPP (SPP, no = 0, yes = 1). Other variables considered were gender (female = 0, male = 1), age (decades), a diagnosis of personality disorder (personality disorder, no = 0, yes = 1), Indigenous status, defined as identifying as Aboriginal and/or Torres Strait Islander (Indigenous, no = 0, yes = 1), the number of previous suicide attempts (n), method of suicide attempt (overdose = 1, other = 0), admitted to hospital (no = 0, yes = 1) and year the suicide attempt occurred (year). As a small number of persons was known to re-present many times, it was considered that this might unduly skew effect estimates of predictors in favour of the attributes of the overrepresented individuals. To test this possibility, models were run using the full data-set and then truncated at various suicide attempt presentation frequencies based on the relative contribution of events by individuals. A truncation point of 5 offered the most robust modelling of the effects of frequently re-presenting individuals while still demonstrating all factors significantly predicting time to re-presentation observed at other truncation points. This truncation point is consistent with others reported in similar time-to-recurrent-event analyses.Reference Schukken, Bar, Hertl and Gröhn32
Graphs of predicted hazards against time to re-presentation were plotted for specific values of variables associated with significant hazard ratios. The hazard is the instantaneous probability that a suicide attempt event occurs at a particular time, given that a suicide attempt has not already occurred to that time.Reference Cleves, Gould and Marchenko33 The hazard ratio (HR) is the ratio of the hazard under one condition as compared with an alternative, e.g. being on the SPP versus not being on the SPP.
For each model type, each possible covariate was added to a model containing SPP status. Those with P ≤ 0.10 were included in all possible combinations and retained in the final model if consistently P < 0.05. Plausible interactions were tested (SPP × personality disorder, SPP × Indigenous status, SPP × order (whether it was a person's first or subsequent suicide attempt) and SPP × age) and retained in the model if P < 0.05. Where a covariate was shown to be significant in one of the model types, it was included in all for comparison purposes. Regression diagnostics including calculation of variance inflation factors to test for collinearity were undertaken. Where appropriate, the proportional hazards assumption was checked for all covariates using Schoenfeld residuals.
Ethics and consent
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The project was recognised as a quality activity by the Gold Coast Hospital and Health Service Human Research Ethics Committee (HREC) on 10 October 2018 (reference LNR/2018/QGC/47473) and did not require consent from patients.
Results
Population description
There were 737 suicide attempt presentations between July and December 2017. Demographic and clinical characteristics of patients associated with each presentation were similar between those who were placed on the SPP and those who were not (Table 2). The exceptions were persons presenting having a diagnosis of a personality disorder and having had a previous suicide attempt. People with personality disorder were far less likely (P = 1.5 × 10−8) to be associated with subsequent placement on the SPP than those who did not have such a diagnosis, and people with a first suicide attempt were more likely to be placed on the SPP (P = 0.01).
Table 2 Description of presentations with suicide attempts July–December 2017, by placement on the suicide prevention pathway
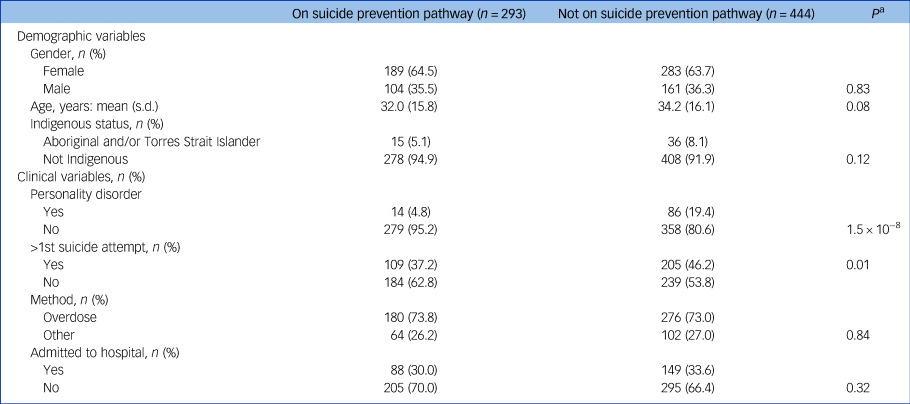
a. P-values were derived from χ2-tests or t-tests, as appropriate.
Re-presentations with a suicide attempt: cross-sectional analysis
Persons who had a suicide attempt presentation between 1 July and 31 December 2017 were followed for 90 days; re-presentation rates within 7, 14, 30 and 90 days for persons placed on the SPP and those who were not are shown in Fig. 1. Of 444 presentations in which the person had not been placed on the SPP, 37, 50, 67 and 102 re-presented within 7, 14, 30 and 90 days respectively. Of 293 presentations in which the person had been placed on the SPP, 5, 10, 25 and 42 re-presented within 7, 14, 30 and 90 days, respectively. The relative risks of re-presentation when placed on the SPP compared with not being on the SPP were the following: within 7 days, RR = 0.29 (95% CI 0.11–0.75), P = 0.007; 14 days, RR = 0.38 (95% CI 0.18–0.78), P = 0.006; 30 days, RR = 0.55 (95% CI 0.33–0.94), P = 0.028; and 90 days, RR = 0.62 (95% CI 0.41–0.95), P = 0.027.

Fig. 1 Re-presentations with a suicide attempt at 7, 14, 30 and 90 days, by placement on the suicide prevention pathway (SPP).
Time-to-recurrent-event analysis
Time-to-event analysis was conducted on 1534 suicide attempt presentations, from 1 January 2009 to the censor date of 31 December 2018. These presentations constituted a history of up to 10 years for each of the originally identified 604 persons. Results of this analysis are shown in Table 3 and Fig. 2.
Table 3 Hazard ratio estimates for each time-to-event modela considered

HR, hazard ratio; SPP, suicide prevention pathway; >1st attempt, subsequent suicide attempt presentation compared with the first; AG–CP, Anderson–Gill counting process; PWP–TT, Prentice–Williams–Petersen total time; PWP–GT, Prentice–Williams–Petersen gap time; shared frailty, Weibull gamma shared frailty; mixed effects, multilevel mixed effects parametric; Cox shared frailty, Cox proportional hazards shared frailty.
a. Models shown are based on a truncation point of five suicide attempts.

Fig. 2 Hazard ratio estimates for each predictor variable in each model.
SPP, suicide prevention pathway; SA, suicide attempt; AG–CP, Anderson–Gill counting process; PWP–TT, Prentice–Williams–Petersen total time; PWP–GT, Prentice–Williams–Petersen gap time; shared frailty, Weibull gamma shared frailty; mixed effects, multilevel mixed effects parametric; Cox shared frailty, Cox proportional hazards shared frailty.
The number of suicide attempt presentations for an individual was found to be a significant time-to-event predictor across each model. Specifically, the first suicide attempt was associated with a lower hazard for re-presentation, whereas all subsequent presentations were each associated with higher hazards of similar values. Consequently, the ‘order’ variable was dichotomised to represent either the first (1) or a subsequent (2) suicide attempt event and renamed ‘>1st attempt’.
In addition to the SPP, four covariates (personality disorder; >1st attempt; age; and Indigenous status) were shown to significantly influence time to re-presentation with a suicide attempt. Placement on the SPP was associated with an HR < 1.0, meaning that it reduced the probability of a repeated suicide attempt after the initial attempt to approximately 65% of that of a person not on the SPP (the range was HR = 0.568–0.675, depending on the model). Conversely, being diagnosed with a personality disorder was associated with an increased hazard for a repeated suicide attempt presentation (by up to 2.7 times) compared with a person not diagnosed with personality disorder. Having had a preceding suicide attempt in the observation period (>1st attempt) was also associated with an increased hazard, compared with first-time presenters (detected in four out of six models). Being Indigenous increased the hazard of a repeated suicide attempt presentation by approximately 1.5 times, compared with not being Indigenous. Increasing age by 10 years decreased the hazard of a repeated suicide attempt by approximately 5–8%.
Using the complete data-set, an interaction between SPP and >1st attempt was associated with an increased time to suicide attempt (HR = 1.6, P = 0.036). That is, there was a differentially greater effect of the SPP to increase time to suicide attempt re-presentation if the person was put on the SPP after their first suicide attempt presentation rather than after a subsequent presentation. The effect was similar in truncated data-sets (e.g. truncated at five presentations for the shared frailty model; HR = 1.5, P = 0.095) but was not included in the presented models (Table 3 and Fig. 2) because P > 0.05. For interest, however, its effect, if included, is demonstrated in Fig. 3(b). No other interactions tested were found to be potentially important. The apparent lack of an SPP × personality disorder interaction (e.g. HR = 1.1, P = 0.77 for the shared frailty model) was of interest owing to the observation that people with a personality disorder were less likely to be placed on the SPP (Spearman rank correlation −0.40, P < 0.001), which may have been the result of clinical decision-making (see Discussion).

Fig. 3 Population predicted hazards based on the Weibull gamma shared frailty model.
(a) Effect of the suicide prevention pathway (SPP) and first or subsequent suicide attempt (SA) presentations for a non-personality disorder, non-Indigenous, 29-year-old (50th centile) individual. The curves for 1st presentation not on the SPP and >1st presentation on the SPP are superimposed. (b) Effect of the SPP and first or subsequent suicide attempt presentations when an SPP × 1st presentation interaction (P = 0.095) was included in the model. Hazards are shown for a non-personality disorder, non-Indigenous, 29-year-old individual. (c) Effect of the SPP and diagnosis of personality disorder (PD) for a 1st presentation, non-Indigenous, 29-year-old individual. (d) Effect of the SPP and Indigenous status for a 1st presentation, non-personality disorder, 29-year-old individual. (e) Effect of the SPP and age (22 years, 25th centile; or 36 years, 75th centile) for a 1st presentation, non-personality disorder, non-Indigenous individual.
The relative relationships of factors influencing time to repeated suicide attempt are shown in Fig. 3. Different levels of each predictor variable are shown along with being placed on the SPP or not. These graphs also demonstrate how the hazard for a repeated suicide attempt decreases rapidly as the time from the previous attempt increases. Figure 3(a) shows that being placed on the SPP is essentially equivalent to the suicide attempt event being the first for an individual rather than a subsequent attempt (as is indicated by the curves being virtually superimposed). As noted earlier, the effect of an interaction between SPP and >1st attempt is shown in Fig. 3(b). Compared with Fig. 3(a), the curve for 1st presentation resulting in placement on the SPP is lower and the curve for >1st presentation resulting in placement on the SPP is higher, indicating that the SPP has a greater beneficial effect if applied at the first suicide attempt.
Being Indigenous and presenting with >1st attempt were positively correlated with a diagnosis of personality disorder (Spearman rank correlation 0.33, P < 0.001, and 0.24, P < 0.001 respectively). However, the variance inflation factors of 1.3 (SPP), 1.4 (personality disorder), 1.2 (Indigenous status) and 1.1 (>1st attempt) do not suggest that these correlations would unduly affect the HR estimates.
It should be noted that the effect of each predictor variable on time to a repeated suicide attempt is proportionally additive with the effects of other predictors in the model. This means that being on the SPP will reduce the hazard for a repeated suicide attempt equally in proportion for any individual. For example, being placed on the SPP will reduce the hazard to about 65% of the original hazard whether the presenting individual is an Indigenous person, a young person, a person with personality disorder or none of these.
Discussion
The Zero Suicide framework has gained international momentum in recent years while at the same time drawing criticism due to the lack of robust evidence-base supporting its effectiveness.Reference Mokkenstorm, Kerkhof, Smit and Beekman1,Reference Coyne6 In this paper we demonstrate a significant reduction in risk of repeated suicide attempts to approximately 65% of a natural risk in patients receiving a suite of interventions following the Zero Suicide framework.
Significant reductions in suicide attempt re-presentation rates were seen within 7, 14, 30 and 90 days after the initial attempt for people on the SPP compared with those not on the SPP. Being on the SPP was shown to be particularly efficacious in the first 14 days, which is probably due to the average duration of placement on the SPP being around 16 days, during which time the patient remains in active contact with the health service through face-to-face appointments. However, the continued effectiveness of the SPP after this period suggests a sustained effect of the suite of interventions delivered during those first 2 weeks. We note that the rates of repeated suicide attempts at 90 days were relatively high in both groups, compared with an average of 16% reported in earlier systematic reviews.Reference Owens, Horrocks and House11,Reference Carroll, Metcalfe and Gunnell34 The discrepancy could be partly explained by the limitations of the utilised project design; Owens et alReference Owens, Horrocks and House11 showed that low-quality studies showed more dispersed values around a higher median than high-quality studies (21 v. 15% repetition rates). Additional factors may be the use of presentation-based rather than person-based analysis, and the high levels of sensitivity in detecting suicide attempts in hospital administrative data through the use of a machine learning algorithm in our work.Reference Stapelberg, Sveticic, Hughes and Turner26,Reference Sveticic, Stapelberg and Turner35
Time-to-recurrent-event analysis was used to model the effect of the SPP and other covariates on time to re-presentation with a suicide attempt. Irrespective of the model used, results showed that being placed on the SPP led to a longer time to re-presentation compared with those not placed on the SPP. In addition, we were also able to show that people diagnosed with a personality disorder, Indigenous people, those presenting with their second or subsequent suicide attempt as opposed to their first, and younger people were associated with higher HRs, indicating an increased risk of re-presentation. This aligns with literature identifying Indigenous persons,Reference Elliott-Farrelly36 people diagnosed with personality disorder (especially borderline personality disorder)Reference Schneider, Wetterling, Sargk, Schneider, Schnabel and Maurer21,Reference Gunderson and Ridolfi22 and those with multiple past suicide attemptsReference Beautrais20,Reference Bergen, Hawton, Waters, Cooper and Kapur37 as having a heightened risk for suicide attempts.
The effects of the SPP act proportionately in reducing hazards for suicide attempt re-presentation for all patient groups in the study. For example, a person diagnosed with a personality disorder benefits proportionately from being placed on the SPP, as their hazard is reduced to 65% of their original hazard, and the hazard for a person not diagnosed with personality disorder is also reduced to 65%, even though the former begins with a higher natural hazard. This finding has an important practical implication as it was observed that people diagnosed with personality disorder were less likely to be placed on the SPP, possibly because clinicians assumed that the SPP would be less effective. Suicide attempts in people with personality disorder are frequently perceived to be communicative gestures or ambivalent in intent.Reference Gunderson and Ridolfi22,Reference Soloff, Fabio, Kelly, Malone and Mann38 As there was no SPP × personality disorder interaction, the SPP was seen to be equally effective in those with a diagnosis of personality disorder. We strongly recommend that all patients with personality disorder presenting with a suicide attempt be placed on the SPP.
Our demonstration of the efficacy of the SPP in first-time presenters makes it imperative for services to identify vulnerable individuals who have not previously presented and provide assertive outreach and clinical interventions for them. Such action may involve strengthening partnerships with referral sources such as the primary care sector and non-government services and improving screening. Furthermore, we can help prevent first presenters from becoming multiple presenters (who have a higher natural hazard) by placing all first-time presenters on the SPP. This would ensure gaining the benefits of the SPP and of being a first-time presenter simultaneously and take advantage of the possibility that the SPP has a greater beneficial effect if applied at the first suicide attempt.
Finally, we note that our work shows a significant reduction in risk of repeated suicide attempt that is larger than for other studies that have previously evaluated the outcomes of individual aftercare interventions.Reference Milner, Carter, Pirkis, Robinson and Spittal16,Reference Inagaki, Kawashima, Kawanishi, Yonemoto, Sugimoto and Furuno39 In this work, we measured the cumulative effect of a suite of interventions, which may act synergistically in terms of positive benefit, making comparison with studies of individual interventions challenging.
Limitations
This work focused on re-presentations with a suicide attempt as an indicator of the efficacy of the SPP. While there is a substantial relationship between the clinical profiles of suicide attempts, particularly those of high lethality, and deaths by suicide,Reference Beautrais12 it is recognised that the definitive measure of the SPP effectiveness will be a reduction in deaths by suicide.
We could not identify whether a person who did not re-present during the follow-up period had died. Owing to the rarity of such instances, however, it is unlikely that these cases would contribute significantly to the observed difference in re-presentations. A data linkage project is planned to track the long-term outcomes of GCMHSS patients and hence measure the effect of placement on the SPP on deaths by suicide. Another limitation was that we were only able to detect people who presented or re-presented to the GCHHS catchment area. This has likely accounted for an under-enumeration of repeated suicide attempts, particularly given some estimates that less than 30% of people seek help at a hospital after engaging in suicidal behaviour.Reference De Leo, Cerin, Spathonis and Burgis40
As this work employed an observational design involving implementation of the SPP in a functioning health service there was obvious potential for ‘cross-contamination’ of elements of the SPP to treatment as usual. This might have occurred because clinicians used certain elements of the SPP in the treatment of patients not denoted as being placed on the SPP or because patients were placed on the SPP following a previous suicide attempt but not the current one. Further, some patients in the SPP group may not have completed all the elements of the SPP, particularly as the time frame from which the cohort of suicide attempt presentations was sourced (July to December 2017) was a relatively early period after the implementation of the SPP at GCMHSS in December 2016, and the desired fidelity to the full clinical protocol may have not yet been achieved. However, it should be noted that the above limitations related to potential cross-contaminations of the groups would tend to decrease the discriminating ability with respect to the effect of the SPP placement on repeat suicide attempts. As we still noted a beneficial effect of the SPP placement, we believe that this in fact enhances the reliability of our findings. At the same time, we acknowledge that the fact that this project tested for the effectiveness of the SPP as a suite of interventions, each exposed to a range of variables difficult to measure and subsequently control for, limits the potential for replicability of our findings in other contexts.
Although some of the measured differences in participants’ characteristics are shown in Table 2, a further limitation is that not all differences in clinical and personal characteristics can be measured and accounted for. Furthermore, we are aware of the potential lack of accuracy of the diagnostic codes used by emergency department staff, particularly in identifying individuals with personality disorders.Reference Howell, Wills and Johnston41
Finally, we acknowledge that the project design prevents making firm conclusions about the efficacy of the SPP, in that the observed relationships cannot be interpreted as causal. There is thus a requirement for future studies to use more robust designs to demonstrate causality, such as a randomised controlled trial (RCT). We note, however, that such designs might pose significant ethical challenges regarding randomisation and masking and would be challenging to implement pragmatically for evaluation of the SPP outcomes.
Future directions
It is hoped that the results of this work will inform the design and analysis of future evaluation studies in this field.
Future work might examine long-term trends in the balance between repeated suicide attempts, self-harm and death by suicide and how these are affected by the SPP. For example, among persons with a past suicide attempt, increased future presentations with suicidal ideation could, in fact, be indicative of improved help-seeking behaviour. It is therefore possible that placement on the SPP may result in a shift in the nature of subsequent presentations from more to less severe.
There are some indications that certain interventions that constitute key elements of the SPP may have particular ‘protective’ value in the long term (e.g. when safety planning is done well, in particular if it includes the family).Reference Stanley, Brown, Brenner, Galfalvy, Currier and Knox42 Assessing individual contributions of the elements of the SPP, including the effect of increased clinician time with patients or exposure to elements of other evidence-based interventions received during their engagement with the mental health service, remains a goal for future work. This is especially important because different services might implement different clinical assessment tools or interventions as part of a Zero Suicide framework. Method and lethality of suicide attempt is another area of interest, as some literature indicates that these have a differential impact on the frequency of subsequent suicidal behaviours.Reference Runeson, Tidemalm, Dahlin, Lichtenstein and Långström43
With many hospital and health services across Australia, and globally, adopting the Zero Suicide framework, a key recommendation is that a robust evaluation, including quantitative analysis methods used here, be incorporated as an integral component of a clinical pathway implementation. Future work should pivot to examining changes in rates of death by suicide as well as suicidal presentations and, if possible, adopt a design that can establish causal relationships between clinical service changes and these rates. Such work would require an all-of-services approach in a given region, including working with primary care providers and non-governmental service providers.
Supplementary material
Supplementary material is available online at http://doi.org/10.1192/bjp.2020.190.
Data availability
This study used data collected at Gold Coast Mental Health Specialist Service as part of clinical practice and used in the evaluation of its suicide prevention strategy.
Author contributions
Authors' contributions to this study were as follows: formulating the research questions – NJCS, KT, MW, JS; designing the study – NJCS, KT, JS; carrying out the study – NJCS, JS, KT, TG-A, AA-C, MW, SW-M, JS, IH, LL, CP, RK, NG, SW, MW; analysing the data – IH, JS, NJCS, TG-A; writing the article – NJCS, JS, IH, AA-C, TG-A, NG, DG, RK, LL, CP, HVE, SW, MW, SW-M, KT.
Declaration of interest
None.
ICMJE forms are in the supplementary material, available online at https://doi.org/10.1192/bjp.2020.190.












eLetters
No eLetters have been published for this article.