Many find inspiration and meaning in Nietzsche's famous words, ‘What does not destroy me, makes me stronger’. The theory behind these words is the stress inoculation hypothesis, which attempts to predict an individual's reaction to a stressful event on the basis of their past experiences.Reference Meichenbaum and Novaco1 Specifically, this hypothesis posits that experiencing manageable stressors may improve an individual's ability to cope with future stressors by providing a context in which to practise effective coping skills and build a sense of mastery over stressors.Reference Updegraff, Taylor and Miller2 This in turn could enhance resilience – broadly defined as positive psychological adaptation to adversityReference Southwick, Litz, Charney and Friedman3 – and reduce later vulnerability to poor mental health outcomes.Reference Meichenbaum and Novaco1,Reference Seery, Leo, Lupien, Kondrak and Almonte4 However, whether this holds true when individuals are later exposed to traumatic stressors, specifically for some of the most common and debilitating stress-related clinical conditions such as major depressive disorder (MDD) or post-traumatic stress disorder (PTSD), remains open to debate.Reference Hammen5,Reference Yehuda6
Manageable versus traumatic stressors
Traumatic stressors are different from manageable stressors in that manageable stressors are typically less severe, allowing most individuals to engage in coping efforts without exceeding their capacity to manage such stressors. For example, someone who has lost their job may find certain strategies (e.g. problem-solving, physical exercise and social support) helpful in managing the stress of unemployment; in turn, this experience could provide a template for coping effectively with later stressors. If the later stressor were, say, another episode of unemployment, this would be an example of direct tolerance – a type of inoculation where the prior stressor is the same as the later exposure.Reference Southwick, Litz, Charney and Friedman3 Conversely, if the later stressor were a divorce, this would be an example of cross tolerance – a type of inoculation where the prior stressor is different from the later exposure. As illustrated in these examples, both prior and later exposures are manageable stressors. According to the inoculation hypothesis, this would increase the likelihood of successful initial coping and subsequent inoculation against stress-related disorders such as MDD and/or PTSD.
Compared with manageable stressors, traumatic stressors (e.g. rape, combat) are more extreme in nature and can overwhelm an individual's ability to cope effectively by inducing emotional distress that exceeds what they can independently manage and/or exhausts the capacity of the stress response system.Reference Van der Kolk, McFarlane and Weisaeth7 Literature suggests that prior stressors, particularly those that are traumatic and unmanageable, can increase risk for later psychiatric disorders such as PTSD and/or MDD.Reference Breslau, Chilcoat, Kessler and Davis8 For example, individuals with maladaptive cognitive vulnerabilities (e.g. negative attentional bias) developed in response to earlier stressors may more readily develop future psychiatric disordersReference Farb, Irving, Anderson and Segal9 – as consistent with a stress sensitisation model. This model is similar to the concepts of ‘kindling’ and/or ‘weathering’, in which earlier vulnerability to psychopathology triggered by initial stressful experiences is posited to decrease the threshold of stress exposure required for developing subsequent psychopathology.Reference Monroe and Harkness10 However, previous work has also shown that prior trauma exposure alone does not predict later PTSD, except among those who developed PTSD after the prior exposure.Reference Breslau, Peterson and Schultz11,Reference Cougle, Resnick and Kilpatrick12 If someone has experienced a prior stressor but did not develop a psychiatric disorder such as PTSD and/or MDD, this suggests that they successfully managed this stressor from a psychological perspective (e.g. seeking support, establishing daily routines, finding meaning) and may thus be prepared to cope successfully with future traumatic exposures – as consistent with the inoculation hypothesis. However, these hypotheses require further investigation in trauma-exposed populations.
The PREDICT study, 2010 earthquake/tsunami and hypotheses of the current study
The main objective of the current study was to test the inoculation hypothesis in an understudied Chilean population. In the midst of a multiwave, cross-national cohort study, the PREDICT study, one of the most powerful earthquakes on record, measuring 8.8 on the Richter scale, struck the coast of central Chile (27 February 2010). This disaster resulted in over 500 deaths, 12 000 injured, 800 000 displaced, and hundreds of thousands of buildings damaged or destroyed.Reference Santos, Byrnes and Lane13 The cities of Concepciόn and Talcahuano, where this cohort was based, were major urban areas that experienced most damage from the earthquake and its subsequent effects, including a tsunami that hit Talcahuano.Reference Santos, Byrnes and Lane13 Chile is particularly vulnerable to earthquakes and tsunamis owing to the country's geographic location on an arc of volcanos and fault-lines circling the Pacific Ocean, otherwise known as the Ring of Fire. Individuals in these high-risk locations are often exposed to recurrent disasters and are therefore likely to be at higher risk for developing post-disaster psychological problems such as PTSD and/or MDD.Reference Norris, Galea, Friedman and Watson14
Hypotheses of the current study
We sought to assess, among individuals with no pre-disaster psychiatric history of MDD or PTSD, whether a history of prior stressors was associated with psychiatric resilience, as evidenced by the absence of negative outcomes where otherwise expected – specifically, whether it protected against the post-disaster development of PTSD and/or MDD, two of the most common psychiatric reactions following disasters.Reference Norris, Galea, Friedman and Watson14 The three hypotheses are: (a) prior experience of a natural disaster will protect against developing post-disaster PTSD and/or MDD (i.e. direct tolerance); (b) prior experience of manageable stressors will protect against developing post-disaster PTSD and/or MDD (i.e. cross tolerance); and (c) there will be a dose–response negative relationship between the number of prior stressors and increased odds of post-disaster PTSD and/or MDD. This study will provide an unprecedented opportunity to answer these questions in an international setting, providing culturally and context-specific information about the risk factors associated with developing psychopathology after a disaster.
Method
Participants
The current analysis utilises two waves of data from the Chilean site of the PREDICT study (n = 1160), a cross-national prospective cohort study with the primary aim of predicting mental health outcomes in primary care attendees.Reference King, Weich, Torres-Gonzalez, Svab, Maaroos and Neeleman15–Reference Bottomley, Nazareth, Torres-González, Švab, Maaroos and Geerlings17 Participants over the age of 15 were recruited from 10 primary care centres within the national healthcare service (used by approximately 75% of the population) in the cities of Concepciόn and Talcahuano, Chile.Reference King, Weich, Torres-Gonzalez, Svab, Maaroos and Neeleman15 Of the 3000 participants who initially agreed to take part, 2839 completed the baseline pre-disaster assessment in 2003 and 1708 completed the post-disaster assessment in 2011, 1 year after the disaster occurred.Reference Fernandez, Vicente, Marshall, Koenen, Arheart and Kohn18 Because the inoculation hypothesis assumes that individuals have successfully coped with prior stressors (i.e. not developing PTSD and/or MDD), those with a pre-disaster MDD and/or PTSD diagnosis (according to the baseline Composite International Diagnostic Interview (CIDI) scores) were excluded. The exclusion and inclusion criterion used to obtain the analytic sample (n = 1160) are shown in Fig. 1.
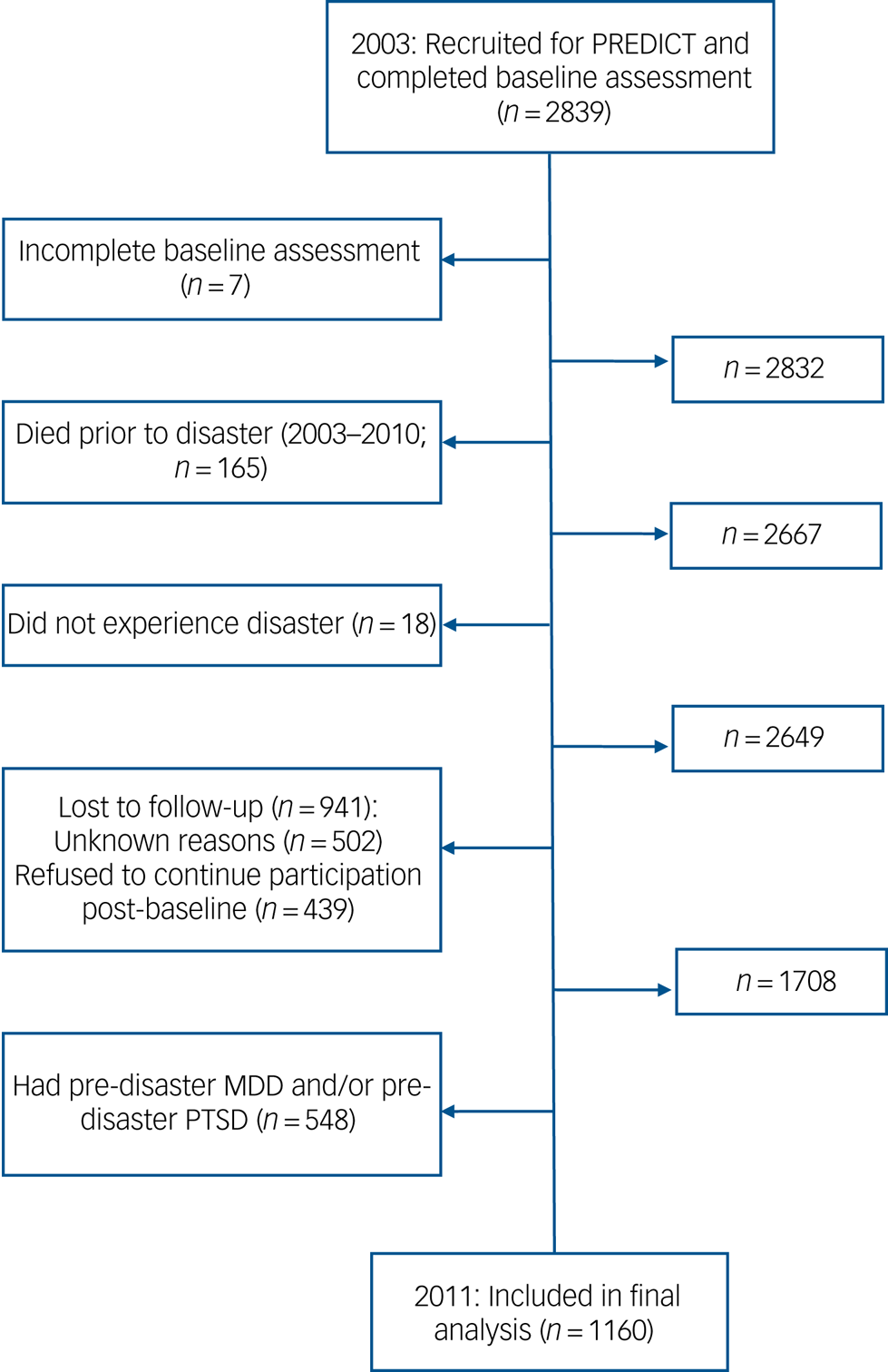
Fig. 1 Flow diagram of excluded/ineligible individuals: The PREDICT study (2003–2011).
MDD, major depressive disorder; PTSD, post-traumatic stress disorder.
Ethics statement
Written informed consent was obtained from all participants. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human participants/patients were approved by the Institutional Review Board at the University of Concepciόn. The current study utilises secondary analysis using de-identified data; therefore, institutional review board approval was not necessary.
Measurements
Dependent variables: post-disaster MDD and post-disaster PTSD (as measured in 2011)
The Composite International Diagnostic Interview (CIDI), Spanish version 2.119 was used to assess pre- and post-disaster MDD and PTSD. The CIDI is a fully structured psychiatric diagnostic instrument that assesses psychiatric disorders via computerised algorithms according to DSM-IV-TR criteria.Reference Robins, Wing, Wittchen, Helzer, Babor and Burke20 The CIDI has good psychometric properties, with excellent interrater reliability, good test–retest reliability and good validityReference Andrews and Peters21 and is used widely throughout the world.Reference Kessler and Ustun22 The CIDI is administered by lay interviewers and does not use outside informants or medical records.19 It also uses skip patterns to efficiently diagnose the presence/absence of a disorder, although this yields limited systematic symptom-level information and may reduce power by excluding individuals with subclinical diagnoses. The translated version of the CIDI is an official World Health Organization Spanish versionReference Vicente, Kohn, Rioseco, Saldivia, Levav and Torres23,Reference Vicente, Kohn, Rioseco, Saldivia, Navarrette and Veloso24 and has been validated in prior national studies conducted in Chile. A prior validation study found that each CIDI section showed moderate to excellent kappa estimates.Reference Vielma, Vicente, Rioseco, Castro, Castro and Torres25
The Depressive Disorders module (section E) of the CIDI was used to diagnose post-disaster MDD in the past 12 months (i.e. since the 2010 disaster occurred). These questions follow the DSM-IV-TR symptom criteria. A full description of this module can be found in supplementary Appendix 2, available at https://doi.org/10.1192/bjp.2020.88. In addition to the post-disaster MDD assessment, a modified version of the PTSD module of the CIDI (section F) Spanish version 2.119 was used to assess post-disaster PTSD. This module asks about all 21 PTSD symptoms from the DSM-IV-TR.26 It is important to note the details of the customisations to the post-disaster PTSD module. There are two major differences in the original PTSD module of the CIDI compared with the modified version. First, unlike the original PTSD module, the modified version does not begin the interview with a complete enumeration of potentially traumatic events as operationalised by the DSM-IV-TR. Instead, participants were only asked whether they had or had not experienced the 2010 natural disaster (i.e. criterion A.1). If the participant did not endorse being in the 2010 disaster, they were screened out of the study. No other history of potentially traumatic events was assessed, to ensure that the assessment was measuring PTSD from the 2010 disaster only (i.e. only individuals with disaster-related PTSD were captured).Reference Fernandez, Vicente, Marshall, Koenen, Arheart and Kohn18
The second major difference in the modified PTSD module was that all the PTSD symptoms were anchored to assess PTSD symptoms due to the 2010 disaster only. This required minor modifications to all the questions, so that they referred directly to it. For example, a question used to measure avoidance symptoms reads: ‘Were you trying to force yourself to not think or talk about the earthquake/tsunami?’; and a question used to measure a symptom of re-experiencing is: ‘After the earthquake/tsunami, did you have nightmares?’. Note that all the assessment questions referenced the 2010 disaster when asking about PTSD symptoms.Reference Fernandez, Vicente, Marshall, Koenen, Arheart and Kohn18
Independent variables: pre-disaster stressors (as measured in 2003)
List of Threatening Experiences
The List of Threatening Experiences (LTE) is a 12-item dichotomous response questionnaire used to measure major categories of stressful life events (from the previous 6 months) involving moderate or long-term threat.Reference Brugha and Cragg27 Stressful events include: serious illness, injury or assault to self or close relative; death of parent, child, spouse/partner, close family friend or another relative (e.g. aunt, cousin, grandparent); marital or relationship separation; serious problem with a close friend, neighbour or relative; unemployment; recent job termination; major financial crisis; problems with the police (including a court appearance); and something of value lost or stolen.Reference Brugha and Cragg27 At the baseline assessment, participants indicated whether each of the 12 different stressful life events had occurred in the previous 6 months. The total score is the sum of the individual items (maximum score: 12).Reference Michalak, Tam, Manjunath, Yatham, Levitt and Levitan28 The LTE has been shown to have good psychometric properties, with excellent test–retest reliability, good interrater reliability and high concurrent validity.Reference Brugha and Cragg27 To examine dose–response relationships between the number of pre-disaster stressors and risk of post-disaster PTSD and/or MDD, the total score was categorised (0, 1, 2, 3, ≥4 stressors) on the basis of the distribution of the sample. Stressors captured by the LTE were conceptualised as ‘cross tolerance’ for the current study.
Prior disaster experience
In the CIDI baseline assessment, participants indicated whether they had previously experienced a natural disaster (i.e. any natural disaster prior to the 2010 earthquake/tsunami) as part of the ‘potentially traumatic events’ portion of the PTSD module of the CIDI. The disaster stressor captured was conceptualised as ‘direct tolerance’ for the current study.
Confounding variables
Confounding variables were selected on the basis of the literature regarding known risk factors for pre-disaster stressors and post-disaster PTSD and MDD.Reference Friedman, Keane and Resick29–Reference Ozer, Best, Lipsey and Weiss31 These include age, gender and educational attainment. Age was collapsed into ‘middle-aged’ or ‘not middle-aged’ (i.e. 45–55 years old versus any other age), because subsequent post hoc analyses showed significant differences only between these two age groups. Education was collapsed into ‘illiterate/elementary school’ versus ‘high school/college’ for the same reason.Reference Fernandez, Vicente, Marshall, Koenen, Arheart and Kohn18
Statistical analyses
Loss to follow-up
As described in our previous work with these data,Reference Fernandez, Vicente, Marshall, Koenen, Arheart and Kohn18 there is potential for selection bias due to differential loss to follow-up in this longitudinal study design. To examine this possibility, χ2 and multivariable logistic regression analyses were conducted to examine the characteristics of those who were lost to follow-up (n = 941 (33.1% of the original sample); Fig. 1). The ‘lost to follow-up’ category included individuals who refused subsequent assessments post-baseline, died, or were lost to follow-up for unknown reasons. Among these 941 individuals, there were significantly more females than males (69% v. 30%; χ2 = 14.84, P < 0.001), more participants with a high-school/college education compared with those who were illiterate or had an elementary school education (73.4% v. 26.6%; χ2 = 11.89, P = 0.001), and more individuals who were not middle-aged relative to those who were middle-aged (83.5% v. 16.5%; χ2 = 4.71, P = 0.03). Multivariable logistic regression models predicting loss to follow-up replicated these findings (results not shown).Reference Fernandez, Vicente, Marshall, Koenen, Arheart and Kohn18 Additional sensitivity analyses examining the differences in the rate of other pre-disaster disorders among those who were and were not lost to follow-up are displayed in supplementary Appendix 1.
Inverse probability weighting
To mitigate the potential selection bias due to differential loss to follow-up, inverse probability censoring weights were calculated. To estimate the censoring weights, the predicted probability of not dropping out based on each participant's exposure (i.e. pre-disaster stressors) and confounder values (i.e. gender, age and education) were estimated using a multivariable logistic regression model. Weights were calculated for each participant as the inverse of this probability. Thus, the weights can be described as the number of participants who are like individual i (in terms of their exposure and confounder values) who would have been in the risk set at the post-disaster assessment in the absence of drop out. In sum, the inverse probability censoring weights create a pseudo-population had drop out been random (with respect to exposure and confounder values). Weights were stabilised to preserve the amount of information in the observed data and minimise variability.Reference Fernandez, Vicente, Marshall, Koenen, Arheart and Kohn18,Reference Robins, Hernan and Brumback32
To mitigate potential confounding bias, inverse probability exposure weights were calculated. To estimate the exposure weights, the probability of each individual's exposure (i.e. pre-disaster stressors) given their confounder values (i.e. gender, age and education) was modelled. The final weights can be described as a pseudo-population where each participant's exposure is independent of their measured confounders.Reference Cole and Hernan33 Weights were stabilised to preserve the amount of information in the observed data and minimise variability.Reference Fernandez, Vicente, Marshall, Koenen, Arheart and Kohn18,Reference Robins, Hernan and Brumback32
List of threatening experiences – questions about assault
It is worth noting that two of the LTE questions ask about assault to self (n = 204; 17.6%) or assault to others (n = 254; 21.9%). According to the DSM-IV-TR criteria, these experiences are considered potentially traumatic events and should not be considered as ‘manageable stressors’. Therefore, all analyses were conducted two ways: one set of analyses with all 12 of the items of the LTE (i.e. those presented in final tables) and another set of analyses with the two items about assault excluded. Results from both sets of analyses were not statistically different from each other (i.e. the confidence intervals overlapped and the point estimates only marginally changed). The similarity of results is likely due to the analytic sample used to operationalise ‘manageable stressors’. Further, given that the LTE has been validated as is (the full 12-item questionnaire), the questions regarding assault were kept for all analyses and we will continue to use the term ‘manageable stressors’ for continuity purposes and to accurately reflect the wording of the inoculation hypothesis.
Post hoc sensitivity analyses
It is important to note that post hoc sensitivity analyses excluding individuals with other pre-disaster disorders besides PTSD and MDD (e.g. alcohol misuse, anxiety disorders, dysthymia, non-affective psychotic disorders) did not substantially change the findings. Further, there were no significant interactions (either additive or multiplicatative) between prior disaster experience (before the 2010 earthquake/tsunami) and stressors. Our results are robust and the effect estimates did not vary substantially, these findings are available on request.
Analysis plan
As mentioned above, because the inoculation hypothesis assumes that individuals effectively manage their stressors to cope with subsequent adversity, those with a pre-disaster MDD or pre-disaster PTSD (according to the CIDI at the baseline assessment) were excluded.
The study hypotheses utilised a series of marginal structural logistic models, with exposure and confounding inverse probability weights. To test direct tolerance, we examined whether a history of being in a disaster (prior to the 2010 disaster) protected against developing post-disaster PTSD and MDD. To test cross-tolerance, we examined whether a history of non-disaster stressors (i.e. total LTE score) protected against developing post-disaster PTSD and MDD. STATA/MP version 12 for Macintosh was used for data management and statistical analyses.34
Results
Descriptive information
Among the individuals with post-disaster PTSD (n = 106; Table 1) and post-disaster MDD (n = 167; Table 2), most were female, not middle-aged, had a high-school/college education and had not experienced a disaster prior to the 2010 earthquake/tsunami. The distribution of the LTE scores in all subsamples was positively skewed.
Table 1 Pre-disaster demographic and stressor information of sample with and without post-disaster PTSD: The PREDICT study, 2003–2011 (n = 1160)

LTE, List of Threatening Experiences; MDD, major depressive disorder; PTSD, post-traumatic stress disorder.
a. Among those with post-disaster PTSD, the mean LTE score was 1.9 (s.d. = 2.1).
b. Refers to whether the participant had experienced a disaster prior to the 2010 earthquake/tsunami.
Table 2 Pre-disaster demographic and stressor information of sample with and without post-disaster MDD: The PREDICT study, 2003–2011 (n = 1160)

LTE, List of Threatening Experiences; MDD, major depressive disorder; PTSD, post-traumatic stress disorder.
a. Among those with post-disaster MDD, the mean LTE score was 1.7 (s.d. = 1.6).
b. Refers to whether the participant had experienced a disaster prior to the 2010 earthquake/tsunami.
Marginal structural logistic regression models – PTSD
As shown in Table 3, model 1 tested the risk of PTSD associated with direct tolerance (i.e. prior disaster experience). Models 2 and 3 tested the risk of PTSD associated with cross tolerance (i.e. prior non-disaster stressor experience). Prior disaster exposure was not a significant predictor of post-disaster PTSD. On the other hand, for every unit increase in prior non-disaster stressors, the odds of developing post-disaster PTSD increased (OR = 1.21, 95% CI 1.08–1.37; P = 0.001; model 2). When these stressors were categorised, those who experienced ≥4 stressors (versus 0 stressors) had increased odds of developing post-disaster PTSD (OR = 2.77, 95% CI 1.52–5.04; P = 0.001; model 3).
Table 3 Marginal structural logistic regression analysesa of pre-disaster stressors predicting post-disaster PTSD: The PREDICT study, 2003–2011 (n = 1154)

LTE sum, List of Threatening Experiences summary score; Ref., reference value.
a. All models use stabilised inverse probability censoring and exposure weights (by gender, age and education) and robust standard error estimates.
b. Refers to whether the participant had experienced a disaster prior to the 2010 earthquake/tsunami.
Marginal structural logistic regression models – MDD
As displayed in Table 4, model 1 tested the risk of MDD associated with prior disaster experience. Models 2 and 3 tested the risk of MDD associated with prior non-disaster stressor experiences. Prior disaster exposure was not a significant predictor of post-disaster MDD (model 1). For every 1-unit increase in prior non-disaster stressors, the odds of developing post-disaster MDD increased (OR = 1.16, 95% CI 1.06–1.27; P = 0.001; model 2). When stressors were categorised, experiencing any number of stressors (relative to 0 stressors) significantly increased the odds of developing post-disaster MDD in a dose–response fashion (model 3).
Table 4 Marginal structural logistic regression analysesa of pre-disaster stressors predicting post-disaster MDD: The PREDICT study, 2003–2011 (n = 1154)

LTE sum, List of Threatening Experiences summary score; Ref., reference value.
a. All models use stabilised inverse probability censoring and exposure weights (by gender, age and education) and robust standard error estimates.
b. Refers to whether the participant had experienced a disaster prior to the 2010 earthquake/tsunami.
Discussion
The current study tested the applicability of the inoculation hypothesis on psychiatric vulnerability in an understudied international population who had experienced a natural disaster. To do so, we assessed whether a history of stressful life events among Chilean adults with no lifetime history of PTSD and/or MDD decreased the odds that a subsequent traumatic experience (i.e. exposure to an earthquake/tsunami) would trigger MDD and/or PTSD. Cumulatively, the findings did not support direct or indirect inoculation. In fact, the results were in the opposite hypothesised direction and are therefore reflective of the stress sensitisation model, which states that experiencing multiple stressors increases the probability of developing a psychiatric disorder (as opposed to more resilience, implied in the inoculation hypothesis).
Because a history of pre-disaster stressors increased the risk of developing post-disaster PTSD and/or MDD, it is likely that this Chilean sample experienced ‘stress sensitisation’. Stress sensitisation posits that a stressor will make an individual more vulnerable to the negative effects of subsequent stressors, rather than developing resilience.Reference Dienes, Hammen, Henry, Cohen and Daley35–Reference McLaughlin, Conron, Koenen and Gilman37 Therefore, an individual who has experienced several stressors in their lifetime will be at higher risk for developing a psychiatric disorder.Reference Nurius, Uehara and Zatzick36 This theory is supported by substantial literatureReference Breslau, Peterson and Schultz11,Reference Cougle, Resnick and Kilpatrick12 and has also been used to explain individual differences in the development, recurrence and maintenance of psychiatric disorders such as PTSD and/or MDD.Reference Harkness, Hayden and Lopez-Duran38,Reference Hankin, Badanes, Smolen and Young39
Unfortunately, the majority of research on PTSD has investigated risk associated with prior traumatic stressors, not manageable stressors.Reference Friedman, Keane and Resick29 This is especially true in populations outside of the USA. In the current study, results indicated that for every one-unit increase in pre-disaster stressors, the odds of developing post-disaster PTSD increased by 21%. However, when stressors were categorised, only participants who experienced ≥4 stressors (i.e. the highest category), relative to 0 stressors, had higher odds of developing post-disaster PTSD. This suggests that the number of prior manageable stressors needs to cross a severity threshold (≥4 stressors) to affect future vulnerability to PTSD.Reference Karam, Friedman, Hill, Kessler, McLaughlin and Petukhova40
In contrast to the PTSD literature, it is well-known that ‘non-traumatic’ psychosocial stressors play an essential role in the etiology of MDD.Reference Farb, Irving, Anderson and Segal9,Reference Monroe and Harkness10 Other literature in international high-trauma settings has suggested that manageable stressors can actually have a stronger impact than traumatic stressors on mental health outcomes.Reference Miller, Omidian, Rasmussen, Yaqubi and Daudzai41,Reference Newnham, Pearson, Stein and Betancourt42 These adversities may leave residual vulnerabilities in the individual, thus increasing the probability of developing MDD because of sensitisation.Reference Monroe and Harkness10 Furthermore, cumulative adversity tends to be more harmful than a single episode, owing to the depletion of coping resources over time.Reference McLaughlin, Conron, Koenen and Gilman37,Reference Kubiak43 This conceptualisation reflects the results of the current study, which indicated a dose–response relationship between the number of pre-disaster stressors and the risk of post-disaster MDD. These stressful events may be associated with depressionReference Harkness, Hayden and Lopez-Duran38 through behavioural (e.g. poor coping mechanisms), cognitive (e.g. negative attention biases, ruminationReference Farb, Irving, Anderson and Segal9,Reference Ruscio, Gentes, Jones, Hallion, Coleman and Swendsen44 ) and/or biological mechanisms (e.g. physiological stress response dysregulationReference McLaughlin, Conron, Koenen and Gilman37,Reference Hankin, Badanes, Smolen and Young39,Reference Fernandez, Loucks, Arheart, Hickson, Kohn and Buka45 ). Although these pathways were not included in the present study, they merit additional investigation in future longitudinal studies.
Strengths and limitations
The present study has some limitations worth noting. First, there is potential for measurement error of the exposure variables (i.e. pre-disaster stressors and pre-disaster PTSD and MDD). The primary concern is that the baseline examination was administered 7 years before the disaster (2003). New stressors that occurred between the baseline assessment and the earthquake (i.e. between 2003 and 2010) may have been missed. It is also possible that individuals developed pre-disaster PTSD and/or pre-disaster MDD during this 7-year period. Given that our analytic sample excluded individuals with any history of pre-disaster PTSD and/or MDD, those who had PTSD and/or MDD would be categorised as false negatives, leading to biased results.
Similarly, there is potential for misclassification of the outcome variables (post-disaster PTSD and/or post-disaster MDD). Given that the post-disaster PTSD assessment was administered approximately a year after the disaster occurred (2011), there are some individuals who may have had disaster-related PTSD but their symptoms had resolved before the assessment took place. Conversely, individuals may have developed delayed-onset PTSD years after the disaster; these individuals would not have been captured as having disaster-related PTSD in our assessment. Fortunately, misclassification of post-disaster MDD is less likely given that the CIDI only assessed post-disaster MDD from the previous year (i.e. between the disaster occurrence and assessment). Another limitation is that the CIDI automatically generates dichotomised diagnoses because of its skip patterns; therefore, we were unable to examine participants with subclinical PTSD/MDD or to accurately measure PTSD/MDD symptoms.19 Excluding those with subclinical diagnoses may also have resulted in a loss of power. Future studies should use multiple time points before and after a disaster to more accurately examine the longitudinal course of PTSD and MDD.
Although the study was conducted in a longitudinal and prospective fashion, the results likely do not reflect causal relationships due to random error, potential type II error, unmeasured confounding, moderators or mediators. For example, the stressor questionnaire did not measure the individual's appraisal of the stressor, their coping response, the stressor's contextual meaning, the frequency/load of the stressful events and/or whether the person achieved complete mastery over the stressor.Reference Fernandez, Loucks, Arheart, Hickson, Kohn and Buka45 This information is pertinent to providing stronger evidence for the inoculation hypothesis – we strongly recommend that future studies examining stress response include these indicators.Reference Monroe46 Further, the LTE measured stressors from the 6 months prior to the baseline assessment. This is likely not a large enough time frame to capture the extent to which people may have experienced life stressors, which may have led to biased results. Finally, findings may not necessarily generalise to other populations outside of Chile.
Despite these limitations, the current study has many unique strengths. Analyses took advantage of a rare opportunity to study adults who had undergone a psychiatric and stressor evaluation in a large sample prior to exposure to one of the most powerful earthquakes in history, thus providing a clearer understanding of the pre-existing risk factors for developing PTSD and/or MDD.Reference Fernandez, Vicente, Marshall, Koenen, Arheart and Kohn18 This type of rich longitudinal data does not exist in the disaster literature.Reference Norris, Galea, Friedman and Watson14 Previous studies that have attempted to address these issues have been severely limited by small convenience samples, lack of diagnostic instruments and scarcity of pre-disaster information.Reference Updegraff, Taylor and Miller2,Reference Fernandez, Vicente, Marshall, Koenen, Arheart and Kohn18 The current study overcomes these limitations and allows for testing of hypotheses not previously possible using a methodologically robust study design. This information is critical to understanding variations in risk of PTSD and/or MDD, with the overall goal of identifying those who may need mental health treatment after a disaster.Reference Fernandez, Vicente, Marshall, Koenen, Arheart and Kohn18 By examining who has truly new-onset PTSD and MDD after a natural disaster, the causal mechanisms of these illnesses can be more accurately determined. Increased knowledge regarding the individual variations of these disorders is essential to inform targeted mental health interventions after a natural disaster, especially in under-studied populations.Reference Santos, Byrnes and Lane13
Supplementary material
Supplementary material is available online at http://doi.org/10.1192/bjp.2020.88.
Data availability
Authors have ongoing access to de-identified data.
Acknowledgements
We thank those who participated in this study and our colleagues in Chile, who graciously shared their data with us.
Author contributions
B.V., S.S. and R.K. conceptualised the study and collected the data. C.A.F., B.V., S.S and K.C.K obtained funding to analyse the data. C.A.F. and K.L.A. undertook the statistical analysis. C.A.F. wrote the first draft of the manuscript. K.W.C. wrote the second draft of the manuscript. S.L.B., R.K., K.L.A., B.D.L.M. and K.C.K. mentored C.A.F. and served on her dissertation committee. All authors contributed to the proofreading and final approval of the manuscript.
Funding
This work was supported by the National Institute of Mental Health (grant F31MH104000 to C.A.F. and grant 5T32MH017119-30 to K.C.K.) and FONDEF Chile (grants D021-1140 and 1110687 to B.V.).
Declaration of interest
None.
ICMJE forms are in the supplementary material, available online at https://doi.org/10.1192/bjp.2020.88.











eLetters
No eLetters have been published for this article.