Introduction
Poor mental health is being reported at increasingly younger ages, and there has been much focus traditionally on affective disorders and anxiety (Caspi et al., Reference Caspi, Houts, Ambler, Danese, Elliott, Hariri and Ramrakha2020; Merikangas et al., Reference Merikangas, He, Burstein, Swanson, Avenevoli, Cui and Swendsen2010). However, there is growing recognition of the importance of psychotic phenomena in youth. Psychotic experiences (PE), the subclinical expressions of psychotic symptoms, occur in the absence of a psychotic disorder and mainly concern auditory (both verbal and non-verbal) and, less commonly, visual hallucinatory experiences (HE) (Kelleher, Harley, Murtagh, & Cannon, Reference Kelleher, Harley, Murtagh and Cannon2011). PE are most prevalent during late childhood, with 17% of 9–12 year olds within the general population reporting these phenomena (Kelleher et al., Reference Kelleher, Connor, Clarke, Devlin, Harley and Cannon2012a), and a further 12% of children and adolescents reporting auditory hallucinations specifically (Maijer, Begemann, Palmen, Leucht, & Sommer, Reference Maijer, Begemann, Palmen, Leucht and Sommer2018). A growing body of research suggests that PE are not only homotypically or inevitably linked to psychotic disorders (Healy et al., Reference Healy, Brannigan, Dooley, Coughlan, Clarke, Kelleher and Cannon2019), but also represent markers of vulnerability for a range of psychopathology and poorer functional outcomes into adulthood (Carey et al., Reference Carey, Gillan, Healy, Dooley, Campbell, McGrane and Cannon2021). PE have also been shown to be associated with suicidality and substance abuse in young people (Cederlöf et al., Reference Cederlöf, Kuja-Halkola, Larsson, Sjölander, Östberg, Lundström and Lichtenstein2017; Honings, Drukker, Groen, & van Os, Reference Honings, Drukker, Groen and van Os2016; Kelleher, Cederlöf, & Lichtenstein, Reference Kelleher, Cederlöf and Lichtenstein2014). For the majority of young people (75–90%), PE are transient in nature (Calkins et al., Reference Calkins, Moore, Satterthwaite, Wolf, Turetsky, Roalf and Gur2017), but, in those for whom PE persist, greater risk of adverse outcomes have been shown (Calkins et al., Reference Calkins, Moore, Satterthwaite, Wolf, Turetsky, Roalf and Gur2017). The recurrence of PE therefore may be indicative of a more serious underlying psychopathological process.
Early childhood development, which includes physical, social and cognitive development, strongly influences mental health and well-being throughout the lifespan and is critical for influencing a child's developmental trajectory (Irwin, Siddiqi, & Hertzman, Reference Irwin, Siddiqi and Hertzman2007). Early childhood represents a critical time for the early detection of risks for later psychopathology (Green et al., Reference Green, Tzoumakis, Laurens, Dean, Kariuki, Harris and Carr2019). Cognitive variances in early life lead to a very high risk of not only developmental issues for children, but also social-emotional and behavioural problems at later ages (Carter, Briggs-Gowan, & Davis, Reference Carter, Briggs-Gowan and Davis2004), and should be signalled for clinical intervention.
Investigations of early childhood development and its role in predicting later schizophrenia have been carried out using birth cohorts and data linkage approaches but less research has been carried out with HE as the outcome. Motor deficits during development likely represent an endophenotype for schizophrenia (Burton et al., Reference Burton, Hjorthøj, Jepsen, Thorup, Nordentoft and Plessen2016). Clarke et al. (Reference Clarke, Tanskanen, Huttunen, Leon, Murray, Jones and Cannon2011), in a study analysing data from the Finnish population register, found that delayed milestones in infancy significantly increased the risk of a later diagnosis of schizophrenia, in a dose–response manner. Cannon et al. (Reference Cannon, Caspi, Moffitt, Harrington, Taylor, Murray and Poulton2002), in analyses from a New Zealand birth cohort study, found that subtle but significant impairments in neuromotor, language and cognitive development were detectable from age 3 in children who reported psychotic symptoms at age 11 and were also detectable in individuals later diagnosed with schizophreniform disorder (but not depression, anxiety or mania) at age 26. However, developmental data were not available before the age of 3. Hameed et al. (Reference Hameed, Lingam, Zammit, Salvi, Sullivan and Lewis2018) showed that a decline in early social and communication skills over the first 4 years of life, and a declining pattern of fine motor skills in males, was predictive of later PE (at age 12 years) in a UK birth cohort.
Most studies in this area have focused on childhood and adolescence, with research showing that cognitive and motor dysfunction at this age is also associated with PE (Carey et al., Reference Carey, Dooley, Gillan, Healy, Coughlan, Clarke and Cannon2019, Reference Carey, Gillan, Healy, Dooley, Campbell, McGrane and Cannon2021; Mollon et al., Reference Mollon, David, Morgan, Frissa, Glahn, Pilecka and Reichenberg2016). A lag in cognitive development from age 8 years has been detected in children who later report PE (Gur et al., Reference Gur, Calkins, Satterthwaite, Ruparel, Bilker, Moore and Gur2014). However, whether differences in developmental trajectory can be noted from infancy remains unclear. Questions pertaining to whether there is an association between early childhood developmental delays and poorer outcomes also remain.
Using data from Gen1 and Gen2 of the Raine study, our study addressed the following aims:
(1) To determine if early childhood development in separate or multiple domains of development in the first 3 years of life is associated with HE in childhood and adolescence.
(2) To compare these associations with those of early childhood development and anxiety/depression in childhood and adolescence.
(3) To investigate whether the presence of early childhood developmental delays are associated with recurrence of HE in adolescence, which is a marker for poorer outcomes.
Methods
Participants
Ethical approval for the study was granted by the University of Western Australia Human Research Ethics Committee (HREC).
Data were taken from The Raine Study, a pregnancy cohort study that began in 1989, in which 2900 pregnant women were enrolled with an average recruitment age of 18 weeks of gestation, from the public antenatal clinic at the major obstetric hospital in Perth, Western Australia, and nearby private practices. The ongoing study has followed 2446 infants born over a 3-year period, with numerous follow-up assessments in childhood and adolescence. Inclusion criteria for mothers' participation in the study included gestational age between 16 and 20 weeks, proficiency in English and an intention to remain in Western Australia so to allow for long-term participation. Demographic and social information of parents/guardians was collected throughout the study. The rate of attrition in the Raine study is 29% from age 1 year to age 17 years (Straker et al., Reference Straker, Mountain, Jacques, White, Smith, Landau and Eastwood2017). Participants are representative of the general Western Australian population at the time of recruitment and into infancy (Straker et al., Reference Straker, Mountain, Jacques, White, Smith, Landau and Eastwood2017).
Measures
Early childhood development
The Infant Monitoring Questionnaire (Bricker, Squires, Kaminski, & Mounts, Reference Bricker, Squires, Kaminski and Mounts1988) (IMQ; now known as the Ages and Stages Questionnaire) was completed by parents/guardians at ages 1, 2 and 3 years. The IMQ is a screening tool for monitoring early childhood development in five broad domains: communication, gross motor, fine motor, adaptive (problem-solving) and personal-social. A 35-item version of the IMQ was administered at ages 1 and 2 years, and a 30-item version was administered at age 3 years. Upon agreement with the authors, age 1 and age 2 IMQ data were condensed to 30-items for standardisation within the analyses, due to the inclusion of one item that is 150 developmental quotient in each domain. This item was therefore removed from each domain at age 1 and age 2 years, and no significant differences were noted. Parents were asked to assess their child's behaviour by domain, and score ‘yes’ if the child does behave in such way, ‘sometimes’ if the child occasionally behaves in such way or ‘no’ if the child does not behave in such way. Higher scores indicate better development. The IMQ contain age-specific developmental items. The IMQ has good criterion validity, sensitivity, specificity and test–retest reliability (Bricker et al., Reference Bricker, Squires, Kaminski and Mounts1988). The IMQ also has good criterion validity when compared with the Bayley Scales of Infant Development, and the Stanford–Binet Intelligence Test (r = 0.89) (Bricker & Squires, Reference Bricker and Squires1989) and is endorsed for use by the American Academy of Pediatrics (Schonhaut, Armijo, Schönstedt, Alvarez, & Cordero, Reference Schonhaut, Armijo, Schönstedt, Alvarez and Cordero2013).
The IMQ was scored as per the instructions in the manual (Squires, Reference Squires1993) and the suggested cut-off scores were used to define low-functioning infants and normal-functioning infants in each domain (see online Supplementary Table S3). Scoring below this cut-off was labelled as ‘Delay’, while scoring above this cut-off was labelled as ‘Average’. A further measure of low functioning was calculated based on scores within the lowest 10th percentile for each domain. The data were also dichotomised and labelled as ‘Low’ (⩽10 percentile) and ‘Average’ (⩾11 percentile).
Childhood/adolescent outcomes: hallucinatory experiences and anxiety/depression
The Child Behaviour Checklist (CBCL)/Youth Self-Report (YSR) (Achenbach, Reference Achenbach1991; Achenbach & Edelbrock, Reference Achenbach and Edelbrock1983) are questionnaires used to measure emotional and behavioural problems in children and adolescents, and contain comparable items (Achenbach, Dumenci, & Rescorla, Reference Achenbach, Dumenci and Rescorla2002). They include eight scales: anxious/depressed, depressed, somatic complaints, social problems, thought problems, attention problems, rule-breaking behaviour and aggressive behaviour. For the purpose of the current analyses, we use CBCL/YSR data collected at ages 10 years (parent-report) and 14 and 17 (self-report) years.
HE were indexed by two items on the ‘thought problems’ subscale of the CBCL/YSR, ‘I hear sounds or voices that other people think aren't there’ (item 40) and ‘I see things that other people think aren't there’ (item 70). These items have been found to have good predictive power for measuring PE (Kelleher et al., Reference Kelleher, Harley, Murtagh and Cannon2011). HE were considered as the endorsement of ‘somewhat/sometimes true’ or ‘very true/often true’ for either or both items, at one or more of the three time-points. Subgroups of those with transient experiences (reported at one time-point only) and recurrent experiences (reported at more than one time-point) were also created.
Anxious/depressed symptomology was determined using standardised t-scores from the CBCL/YSR anxious/depressed subscale. A cut-off point for t-scores over and including 70 was applied, deemed to be clinically significant by Achenbach (Reference Achenbach1991). Participants with a t-score of ⩾70 at one or more of the three time-points (ages 10, 14 and 17 years) and who had never reported PE were assigned to the anxious/depressed group for comparison.
Covariates
Covariates entered in the analyses included child's age (in months) at the time of their developmental assessment; maternal highest qualification, birthweight, sex at birth and family income at the time of the developmental assessments. Maternal highest qualification was measured when the participants were aged 8 years and was scaled from 0 to 8, and ranged from no qualification to postgraduate diploma/higher degree. Family income was measured at ages 1, 2 and 3 years and was based on five categories (less than $7000, $7000–11 999, $12 000–23 999, $24 000–35 999 and more than $36 000).
Statistical analysis
Participants were divided into the HE group (those who reported PE at any time-point) and the anxious/depressed group (those who scored above the cut-off on the CBCL/YSR at any time-point). Controls were defined as those who did not report HE nor had anxious/depressed symptoms above the cut-off at any time-point. The HE group was subdivided into those with transient HE (those who reported HE at one time-point only) and recurrent HE (those who reported PE at either two or three time-points).
The HE and anxious/depressed groups were compared to control participants on demographic characteristics using independent t tests and a chi-squared test. Raw IMQ scores were converted to z-scores, in order to standardise each version administered at ages 1, 2 and 3 years. The data were analysed using complete case approaches.
Using Stata ver. 16 (StataCorp, 2009), we fitted a series of mixed-effect logistic models with a random effect accounting for the within-subject variance. We report the main effects of early childhood development in the first 3 years of life and later outcomes in childhood and/or adolescence. The exposure variables were the five subscales of the IMQ (communication, gross motor, fine motor, adaptive and personal-social) at ages 1, 2 and 3 years and the primary outcome variables were HE and anxious/depressed group membership. This approach allowed for the identification of associations between developmental scores and HE or anxious/depressed symptoms by detecting unique variances within the scores after accounting for within- and between-subject variance. Each of the aforementioned covariates was adjusted for throughout all of the analyses.
Developmental time-specific investigations were then conducted using separate logistic regression models (at ages 1, 2 and 3 years, respectively) to investigate the association between early childhood development at specific ages and later HE or anxious/depressed symptoms.
Cumulative risk based on multiple domain delays was also calculated. Cut-off scores for the IMQ were applied at each year (ages 1, 2 and 3 years). Three categories were created, 0 domain delays (reference group), 1 or 2 domain delays and 3–5 (multiple) domain delays, where the outcome variables were HE and anxious/depressed. Cumulative risk at age 3 years based on scores within the lowest 10th percentile on each domain was also analysed.
All analyses were also performed to determine associations between the early childhood developmental scores and subgroups of HE, transient and recurrent.
Results
Of the 2446 participants who initially took part, data from n = 1101 participants were available for the present analysis. An attrition analysis is presented in online Supplementary Table S1. Those who were included in the present analysis were younger, had a higher birthweight and better overall development at age 2 years, as well as having mothers with higher qualifications, than those who were not included.
Hallucinatory experiences
The prevalence of HE was 11.1% in the overall cohort. Among the participants in the HE group (n = 228), 48% reported at age 17; 38% reported at age 14 and 14% at age 10 (parent-report). At age 10 years, auditory HE were reported at higher rates (83%) while at 14 years, visual HE were more prevalent (84%). At age 17 years, rates of auditory and visual HE were comparable (50% respectively), and 48% of those who reported HE at this age reported both. Transient experiences were reported in 82% of cases, while recurrent experiences were reported in 18% of cases. A total of n = 40 participants reported HE at two time-points, and a further n = 2 participants reported HE at three time-points.
Anxious/depressed
The prevalence of anxious/depressed symptoms at or above cut-off was 5.6% in the overall cohort. A total of n = 114 participants scored on or above cut-off at least once at ages 10, 14 or 17 years. Seven (6%) had symptoms at more than one time-point. A total of 32% had symptoms at age 17; 18% had symptoms at age 14 and 32% had symptoms at age 10. Of note, n = 43 (37.7%) of the anxious/depressed group also reported PE, and were therefore only included in the HE group.
No significant group differences in demographic characteristics were found between the HE and control groups, with the exception of maternal highest level of education (t = −3.80, p < 0.01) and family income at age 1 (t = −3.76, p < 0.01), where less maternal education and a lower family income at age 1 were noted for the HE group. No significant group differences were found between the anxious/depressed and control groups (see Table 1).
Table 1. Demographic characteristics for the HE group and anxious/depressed groups when compared to the control group

s.d., standard deviation.
a Some missing data.
Association between early childhood development and PE
Mean scores for the IMQ subscales at each age (1, 2 and 3 years) for the HE, anxious/depressed and control groups, including the subgroups of the HE group (transient and recurrent HE), are presented in online Supplementary Table S2.
In the overall random effects model, which accounted for development over the first 3 years of age, there was no significant association between any of developmental domains and HE. In the age-specific analysis, lower adaptive scores at age 1 year were associated with HE. At age 2 years, lower scores in 4 of the 5 developmental domains (with the exception of gross motor) were associated with HE. At age 3 years, lower scores in any of the five domains (communication, gross motor, fine motor, adaptive and personal-social) were associated with HE (see Table 2).
Table 2. Overall and age-specific developmental scores between ages 1 and 3 and risk of later HE (n = 228) [also subdivided into transient (n = 114) or recurrent (n = 42)] and anxiety/depression (n = 71) (compared with Controls (n = 802) (reference group is controls)

OR, odds ratio; CI, confidence intervals.
Bolded text represents analyses where 95% CI do not cross 1.
Odds ratios are adjusted for sex at birth, age, birthweight, maternal highest qualification and family income at each year.
These results are presented, stratified by gender, in Tables S4 and S5 of the online Supplementary materials.
Association between early childhood development and anxious/depressed symptoms
No significant associations between any of developmental domains and anxious/depressed symptoms were found. In the age-specific analysis, only lower gross motor scores at age 3 years were associated with anxious/depressed symptoms (see Table 2).
Association between early childhood development and transient and recurrent HE
No significant associations between any of developmental domains and transient HE were found. In the age-specific analysis, lower adaptive scores at ages 1, 2 and 3 years, as well as lower fine motor scores at age 3 years, were significantly associated with transient HE.
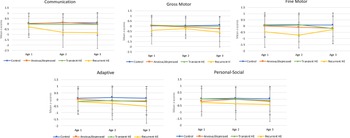
Lower communication scores in the first 3 years were associated with recurrent HE. In the age-specific analysis, lower gross motor and fine motor scores at age 1 year were significantly associated with recurrent HE. At age 2 years, lower scores in 4 of the 5 developmental domains (with the exception of gross motor) were associated with recurrent HE. At age 3 years, lower scores in 4 of the 5 early childhood development domains (communication, gross motor, adaptive and personal-social) were significantly associated with recurrent HE. All data are presented in Fig. 1.

Fig. 1. Longitudinal unadjusted mean z-scores with standard deviation bars for each developmental domain (ages 1, 2 and 3 years) for all groups.
Cumulative risk based on multiple domain delays
Based on cut-off scores, having 3–5 developmental domain delays at age 2 led to an almost 5-fold increased risk for HE (adjusted odds ratio 4.86, 95% confidence interval 1.69–14.05, p = 0.004). Having 1–2 developmental domain delays at age 3 led to an almost 2-fold increased risk for HE and having multiple domain delays increased the risk of HE over 3-fold (see Table 3). Among young people who reported recurrent HE, 30.9% had developmental domain delays at age 2 years and 40.5% had developmental domain delays at age 3 years.
Table 3. Cumulative risk for later HE (n = 228) [Transient (n = 114) or recurrent (n = 42)] and anxiety/depression (n = 71) based on number of developmental delays (below cut-off) at ages 1, 2 and 3 years for each group

a Subgroups of the HE group.
In the percentile analysis, delays (lowest 10th percenile for all participants) in 1–2 domains led to over a 2-fold increase risk for HE, while delays in multiple domains led to over a 3-fold increased risk for HE (see Table 4). For the HE subgroups, delays (by percentile) in 1–2 developmental domains led to over a 2-fold increased risk for transient HE. Delays in 3–5 developmental domains led to over a 7-fold increased risk for recurrent HE.
Table 4. Cumulative risk for later HE (transient or recurrent) and anxious/depressed based on number of domain delays at age 3 years for each group

OR, odds ratio; CI, confidence intervals.
Statistically significant results (p < 0.05) are presented in bold text.
a Subgroups of the HE group.
Multiple developmental domain delays did not lead to a significant increase in cumulative risk for anxious/depressed symptoms, in either the cut-off or percentile analysis.
Discussion
In this study, we examined longitudinally the association between early childhood development and HE in childhood and adolescence in a population-based, representative sample of young people. Participants who reported HE in childhood and/or adolescence showed lower early developmental scores from ages 1 and 2 years on a range of measures. By age 3 years, lower scores in any of the five developmental domains were significantly associated with the risk of later reporting HE. Cumulative risk based on multiple (3–5) domain delays at age 3 years led to over a 3-fold increased risk for HE. For those participants who would later report clinically significant anxious/depressed symptomology, no association was found for overall development over the first 3 years, with the exception of gross motor scores at age 3, and there was also no increased cumulative risk based on multiple domains delays.
Further analyses within the HE group showed that when subdividing the group by transient and recurrent experiences, lower adaptive scores at ages 1, 2 and 3 years were specifically associated with transient HE. Delays in 1 or 2 developmental domains at age 3 years led to over a 2-fold increased risk for transient HE. Stronger effects were found for those who reported recurrent HE, in that a greater number of associations were found with early developmental scores compared to those who only reported HE at one time-point in childhood or adolescence. Both at ages 2 and 3 years, lower scores in 4 of the 5 developmental domains were associated with recurrent HE. At age 3 years, over 40% of the recurrent HE group had at least one developmental delay, as measured by cut-off scores. Multiple (3–5) domain delays led to over a 7-fold increased risk. These findings convey the strong associations between poorer early childhood development and mental health outcomes later in life. Our findings indicate a specific risk associated with the psychosis spectrum, and a strong association with recurrent HE throughout childhood and adolescent development.
The present study has extended previous research on early childhood development and PE. Using the Denver Developmental Screening Test (which includes four measures of early development: fine and gross motor, social and communication skills), Hameed et al. (Reference Hameed, Lingam, Zammit, Salvi, Sullivan and Lewis2018) showed that declining communication and social skills in the first 4 years of life were significantly associated with PE at one time-point at age 12 years. Our study has extended these findings by measuring adaptive (problem-solving) skills, and by examining HE over three time-points in childhood and adolescence. In addition, we explored the comparison between the associations between poorer early development and later HE and clinically significant anxious/depressed symptomology as outcomes. Lower scores in gross motor development at age 3 years were associated with later clinically significant anxious/depressed symptomology. Although the co-occurrence of PE and anxiety/depression has been established (Wigman et al., Reference Wigman, Lin, Vollebergh, van Os, Raaijmakers, Nelson and Yung2011), our findings suggest that poorer development is driven by variability associated with psychosis spectrum symptomology rather than psychopathology more generally, a pattern that has also been shown in other studies (Cannon et al., Reference Cannon, Caspi, Moffitt, Harrington, Taylor, Murray and Poulton2002).
Our findings pertaining to early infant communication development and its relationship with HE, in particular recurrent HE, are in-line with those of Hameed et al. (Reference Hameed, Lingam, Zammit, Salvi, Sullivan and Lewis2018). Impairments in language abilities and the dysconnectivity of language networks have been a central topic in the research of cognitive dysfunction in psychosis, and are thought to contribute to the development of auditory hallucinations (Benetti et al., Reference Benetti, Pettersson-Yeo, Allen, Catani, Williams, Barsaglini and Mechelli2015). Altered white matter in language areas has also been seen in young people with PE (Dooley et al., Reference Dooley, O'Hanlon, Healy, Adair, McCandless, Coppinger and Frodl2020). Our results suggest that language and communication deficits may be detectable as early as the first year of life in young people at risk for psychosis.
Poorer early adaptive development or problem-solving skills were also associated with HE, and in particular, transient HE. The transient HE group were characterised by persistently lower scores in adaptive skills throughout the first 3 years. Reasoning, control and planning are core to adaptive development and delays in these areas have been described in the later stages of childhood in individuals who go on to develop schizophrenia (Reichenberg et al., Reference Reichenberg, Caspi, Harrington, Houts, Keefe, Murray and Moffitt2009). Transient HE, or once-off PE, are linked to poorer global functioning throughout adolescence and early adulthood (Healy et al., Reference Healy, Campbell, Coughlan, Clarke, Kelleher and Cannon2018).
The recurrent HE group had poorer developmental scores in both cognitive and motor domains throughout the first 3 years of life. Motor dysfunction may be reflective of a core feature of psychosis and schizophrenia. Psychomotor developmental deviations are more marked in those later diagnosed with schizophrenia, when compared those later diagnosed with bipolar disorder, and have an earlier onset (Parellada, Gomez-Vallejo, Burdeus, & Arango, Reference Parellada, Gomez-Vallejo, Burdeus and Arango2017). Keskinen et al. (Reference Keskinen, Marttila, Marttila, Jones, Murray, Moilanen and Jääskeläinen2015) hypothesised that delayed motor development may be a marker of other risk processes that interact with genetic liability for psychosis and schizophrenia. Murray et al. (Reference Murray, Jones, Moilanen, Veijola, Miettunen, Cannon and Isohanni2006) retrospectively found that individuals with schizophrenia had early delays in neuromotor milestones. Motor development therefore may be an important trait marker for recurrent HE, which is of important clinical utility, as young people with persistent symptoms have poorer functional outcomes (Healy et al., Reference Healy, Campbell, Coughlan, Clarke, Kelleher and Cannon2018), higher levels of stress reactivity (Collip et al., Reference Collip, Wigman, Myin-Germeys, Jacobs, Derom, Thiery and van Os2013) and are at greater risk of conversion to psychosis (Dominguez, Wichers, Lieb, Wittchen, & van Os, Reference Dominguez, Wichers, Lieb, Wittchen and van Os2011). Recurrence is thought to be indicative of a more serious underlying psychopathological process, and represents an important, early, non-specific marker of later mental health problems (Kelleher et al., Reference Kelleher, Keeley, Corcoran, Lynch, Fitzpatrick, Devlin and Harley2012b).
Strengths of the study include the availability of very early developmental data from infancy from a population-based longitudinal birth cohort and the use of a robust and widely-used assessment of early childhood development, as well as the consistency of measures used across time-points. The HE group also included those with clinically significant anxious/depressed symptomology, due to the established co-occurrence (Kounali et al., Reference Kounali, Zammit, Wiles, Sullivan, Cannon, Stochl and Heron2014) and known overlap with psychopathology more generally (Trotta et al., Reference Trotta, Arseneault, Caspi, Moffitt, Danese, Pariante and Fisher2020). Kounali and colleagues also found that markers of abnormal neurodevelopment showed stronger association with PE, when compared to depression. However, limitations of the study should also be noted. The measurement of HE was confined to the self-report of two types of symptomology (namely, auditory and visual HE); however, these are the most common and validated in childhood community samples (Laurens, Hobbs, Sunderland, Green, & Mould, Reference Laurens, Hobbs, Sunderland, Green and Mould2012). HE were indexed by responses ‘somewhat/sometimes true’ or ‘very true/often true’ which may have been inflated prevalence rates. Furthermore, at age 10 years, a parent-report of HE was used which may have led to an underestimation of HE. The prevalence of clinically significant anxious/depressed symptoms might also be underestimated, particularly as a high proportion who also reported HE were counted within the HE group rather than the Anxious/depressed group as this was the main focus of our analysis. Within the analyses, the omission of parental psychopathology as a covariate must also be noted. This was not consistently measured throughout The Raine Study. Furthermore, the impact of multiple comparisons should be considered, particularly for the results in the anxious/depressed group. Finally, attrition rates within The Raine Study may have led to follow-up bias; however, this may have led to underestimation rather than over estimation of effect sizes since those who were lost to follow-up had poorer development at age 2 years.
In conclusion, our study has shown that cognitive and motor developmental delays can be detected from infancy in young people who go on to report HE in childhood and adolescence. Our findings are reminiscent of the ‘early insult’ theory in psychosis, where early genetic or environmental insults lead to aberrant brain development (Murray & Lewis, Reference Murray and Lewis1987) which is exacerbated thereafter by childhood trauma and adversity (Croft et al., Reference Croft, Heron, Teufel, Cannon, Wolke, Thompson and Zammit2019). Exploration of early childhood development as both a meaningful marker for later mental health outcomes and a viable critical period for early intervention is an exciting emerging area in psychosis research.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291721003883.
Acknowledgements
We are grateful to the Raine study participants and their families and we thank the Raine study staff for cohort coordination and data collection. The core management of the Raine study is funded by The University of Western Australia, Curtin University, Telethon Kids Institute, Women and Infants Research Foundation, Edith Cowan University, Murdoch University, The University of Notre Dame Australia and the Raine Medical Research Foundation. The study is funded by the National Health and Medical Research Council (NHMRC).
Author contributions
Each author contributed significantly to the manuscript. E. Carey (corresponding author) had full access to the data and had complete freedom to direct its analysis and reporting. C. Healy, A. Lin and M. Cannon were involved in the conception and design of the study, as well as the analysis of the data and interpretation of the results. Y. Perry, D. Gillan and A. Whitehouse contributed to the preparing and editing of previous drafts of the manuscript and the critical revision of important intellectual content. All authors gave their approval of the present version to be published.
Financial support
EC, CH and MC are funded by a European Research Council Consolidator Award to MC (724809 iHEAR). AL is funded by a National Health and Medical Research Council Career Development Fellowship (no. 1148793). YP is funded by a fellowship from the Giorgetta Charity Fund. AW is supported by an Investigator Grant from the National Health and Medical Research Council (no. 1173896).
Conflict of interest
None.
Role of the funder or sponsor
The funders had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data. The Raine study approved final manuscript and agreed upon its submission for publication.