Introduction
Anemia is a pathophysiological condition in which there is a marked reduction in the hemoglobin content of blood from the reference concentrations or in the number of red blood cells or defective maturation of red blood cells (Grewal, Reference Grewal2010; Lin et al., Reference Lin, Wei, Zhu, Wang, Su, Feng and Yang2018). It affects all age groups, but pregnant women and children are more vulnerable (Obai et al., Reference Obai, Odongo and Wanyama2016; Lin et al., Reference Lin, Wei, Zhu, Wang, Su, Feng and Yang2018). Anemia, during pregnancy, is a commonly encountered medical disorder associated with adverse effects on the mother and the fetus (Sharma and Shankar, Reference Sharma and Shankar2010). Several exploratory studies estimated that anemia is currently affecting over 1.62 billion people of the world, a population of which 56 million are pregnant women (Balarajan et al., Reference Balarajan, Ramakrishnan, Ozaltin, Shankar and Subramanian2011). Stevens et al. (Reference Stevens, Finucane, De-Regil, Paciorek, Flaxman, Branca, Peña Rosas, Bhutta and Ezzati2011) reported that the global prevalence of anemia in pregnant women is 38%. The significant burden of anemia is born in Asia and Africa were estimated that 60% and 52% of pregnant women, respectively, are anemic, and between 1% and 5% are severely anemic (Leenstra et al., Reference Leenstra, Kariuki, Kurtis, Oloo, Kager and TerKuile2004). Anemia during pregnancy is more prevalent at 43% and 56% in developing countries compared with 9% and 18% in developed countries, respectively (Balarajan et al., Reference Balarajan, Ramakrishnan, Ozaltin, Shankar and Subramanian2011; Abriha et al., Reference Abriha, Yesuf and Wassie2014). Usually, anemia is defined as a hemoglobin level <11.0 g/dl (Obai et al., Reference Obai, Odongo and Wanyama2016). Previous studies have reported that anemia in pregnancy has several contributing factors. Among them iron deficiency is the cause of 75% of anemia cases globally (Gebre and Mulugeta, Reference Gebre and Mulugeta2015; Shams et al., Reference Shams, Ahmad and Wadood2017). Insufficient intake and poor bioavailability of iron-rich foods also have significant contributions to the onset of anemia during pregnancy (Cusick et al., Reference Cusick, Mei, Freedman, Looker, Ogden, Gunter and Cogswell2008; Shams et al., Reference Shams, Ahmad and Wadood2017). About 1000 mg of iron is required during per-pregnancy (Milman et al., Reference Milman, Bergholt, Byg, Erikson and Gradual1999). Anemia in pregnancy is considered a risk factor for poor pregnancy outcomes such as preterm birth (Levy et al., Reference Levy, Fraser, Katz, Mazor and Sheiner2005), low birth weight (Banhidy et al., Reference Banhidy, Acs, Puho and Czeizel2011), fetal impairment, and maternal and fetal deaths (Haas and Brownlie, Reference Haas and Brownlie2001). Poverty is one of the risk factors for iron deficiency in pregnant women (Bodnar et al., Reference Bodnar, Cogswell and Scanlon2002). In Bangladesh, previously conducted different studies and estimating the prevalence found as 37% (Chowdhury et al., Reference Chowdhury, Ahmed, Jebunessa, Akter, Hossain and Shahjahan2015), 40% (Hyder et al., Reference Hyder, Persson, Chowdhury, Lönnerdal and Ekstro2004), 54% and 56.52% (Rahman et al., Reference Rahman, Nessa, Yesmin, Rahman and Rahman2018), 58.9% (Ahmed et al., Reference Ahmed, Mamun, Mahmud, Farzana, Sathi, Biswas, Datta and Ahmad2019), and 63% (Ahmed et al., Reference Ahmed, Mahmuda, Sattar and Akhtaruzzaman2003) of anemia among pregnant women. Therefore, it indicates that a substantial variation in the prevalence of anemia exists within a country. Despite the known consequences of anemia in pregnancy, there is scanty information on the ubiquity of anemia in pregnant women in Bangladesh. Several published studies on the prevalence and associated risk factors of anemia in pregnancy have received antenatal care (ANC) at the different levels of the health care system. Most of the studies were secondary and tertiary health care facilities in private hospitals and some are primary health care levels in government hospitals. Information from the literature indicated that there were no published studies that have addressed to compare the prevalence and associated risk factors of anemia in pregnant women attending ANC at government and private hospitals. The prevalence of anemia in pregnancy varies in women with different socioeconomic conditions, diets, lifestyles, or health-seeking behaviors across different cultures. Anemia during pregnancy is more prevalent especially in poverty, improper nutrition, living in unhygienic conditions, lack of education, women unemployment, lack of health care facilities, and no knowledge of antenatal care. Most of the study subjects were housewives and more than half of the pregnant women were secondary school education level. Most of the women are afforded a low status in society, and their daily health needs were unnoticed. In addition, existing health facilities may not be available to women in need. Besides, lack of education and understanding about health-related issues contribute to delays in seeking care for managing life-threatening pregnancy complications. Generally, pregnant women in the rural area of Bangladesh receive ANC from the community health care center or government hospitals due to poverty. However, to the best of our knowledge, there is no other study that has ever been conducted in the area we are investigating regarding the prevalence of anemia during pregnancy. Therefore, this study aimed to determine the prevalence of anemia and associated risk factors among pregnant women attending ANC at government and private hospitals in different areas in Bangladesh.
Methods
Study design and population selection
This is a cross-sectional, hospital-based study that was conducted at government and private hospitals from January to June 2019. These hospitals are located in two greater districts of Kushtia (Kushtia, Chuadanga, and Meherepur) and Jashore (Jashore, Jhenaidah, and Magura) of Bangladesh. Two regions were selected and the peoples are culturally almost the same in this study. The patriarchal society has resulted in the poor status of women in family and society. The population consists of ethnic Bengalis, the majorities are Muslim and reaming are Hindus or others. The study areas were separated into rural and urban areas, however, the main inequalities across wealth (between the rich and poor) and education. The study participants were healthy pregnant women who visited for ANC at two types of hospitals during the study period. Participants who were pregnant and fulfilled the inclusion criteria were included in the study. Each participant was enrolled only once on their first visit during the study period. Healthy pregnant women, who were greater than 19 years old, gave informed consent to provide information were included, while the participants who were seriously ill and did not want to give their information at the time of data collection were excluded from the study.
Facility setting
The pregnant women received ANC either from the government or from the private sector. In government hospitals, maternity health care, and community health clinic, the facilities for pregnant women are inadequate such as shortage of medical equipment, an unhygienic physical environment, scarcity of power, and potable water. Although the quality of maternal health services provided by the government institutions is poorer than desired, lower and middle-class pregnant women go here regularly due to less education and poverty. As a result, it is assumed that they are financially indigent or they do not have enough knowledge about health care. It is easy to deliver a pregnant woman at a community health clinic for a small amount of money, many times it is risky. In some cases, families take pregnant women to private clinics because of the nonavailability of services at the government hospitals, maternity health care, and community health clinic. Besides the public sector, the private for-profit providers and private not-for-profit basis (NGOs) have a significant number of tertiary-level hospitals providing high-quality services especially for the poor and vulnerable people including pregnant women. Generally, pregnant women of rural areas receive ANC from a government facility, while urban mothers prefer to use the services of private sectors. The health care delivery systems of Bangladesh have different types of health facilities that are available to cover pregnant women with different demographic and socioeconomic backgrounds from all over the country. Thus, data generated from these two types of hospitals may be considered a fair reflection of the whole pregnant women of the country.
Sample size and sampling procedures
The sample size for this study was calculated using the Kish Leslie formula. A single population proportion formula, [n = (Zα/2)2(1 − p)/d2], was used to estimate the sample size. In this particular area, there are no previous studies about the prevalence of anemia during pregnancy, and 50% prevalence of anemia in Bangladesh was used for sample size calculation. Considering 95% CI, 5% margin of error, the sample size will be 384, and the final sample size for this study was 424.
Data-collection instrument
Data on sociodemographic characteristics were collected using structured questionnaires. Each item of the questionnaire was prepared in English and then translated into the native language. Intending to get comments and feedback from the respondents, twenty sets of questionnaires were given during pilot testing. The questionnaire was then modified to bring clarity and improve the understandability and validity. We interviewed in a secure and confidential environment and then the result of biological tests was recorded from the patient obstetric file. Anemia is defined in pregnancy as Hb < 11 g/dl and also classified to mild (10.0–10.9 g/dl), moderate (7.0–9.9 g/dl), and severe (<7.0 g/dl) (Obai et al., Reference Obai, Odongo and Wanyama2016). Data were collected through face-to-face interviews with the pregnant women by the trained B.Sc nursing research students. Cronbach’s alpha is generally used to measure the internal consistency of questionnaires. Reliability of 0.7 or higher is required for the study instruments to continue with this research. According to Nunnally (Reference Nunnally1978), the value of Cronbach’s alpha closer to 1 indicates greater stability and consistency; however, the threshold value in most research studies is set at 0.60. After transforming the responses into constructs in SPSS and running the test, it is found that the Cronbach’s alpha value is more than 0.7 which means that all the instruments used in this research are reliable enough.
Analysis of data
Statistical analysis was performed using SPSS software. Data from the questionnaire were analyzed descriptively and are presented as frequencies and means ± standard deviation (SD). Binary logistic regression was used to identify the factors associated with anemia among the subjects. We used AORs as a measure of association, with a 95% CI. In every case, P-value was set at < 0.05 for statistical significance.
Ethical considerations
Ethical permission was taken from the Faculty of Biological Sciences, Islamic University, Kushtia-7003, Bangladesh. Respondents were informed about the research objectives, methods, and techniques of the study. We collected their signature or thumb impression on the informed consent form. The data were coded, and the identities of the respondents were kept confidential. Subjects had the right to withdraw at any time was emphasized. The interviews were conducted in strict privacy within the hospital premises to maintain confidentiality.
Results
Sociodemographic characteristics
A total of 424 pregnant women receiving hospital-based ANC were included in the study. Among the study subjects, 233 received ANC in the government hospital and 191 in the private hospital. Majority, 220 (51.90%) of the study participants were found in the 20–25 age group and only 18 (4.20%) were found to be 36 or more than 36 years old. More than half of the participants, 226 (53.30%) lived in rural area and 198 (46.70%) pregnant women were in urban area. Most of pregnant women were housewife 384 (90.60%). Among all the participants, 225 (53.20%) pregnant women attended secondary school and 67 (15.80%) completed their graduation. The average (mean ± SD) monthly incomes (US$) of the study subjects in government and private hospitals were 222.74 ± 110.07 and 258.77 ± 146.63, respectively, are significantly (P < 0.01) higher in attending in private hospitals (Table 1).
Table 1. Sociodemographic characteristics of the study participants
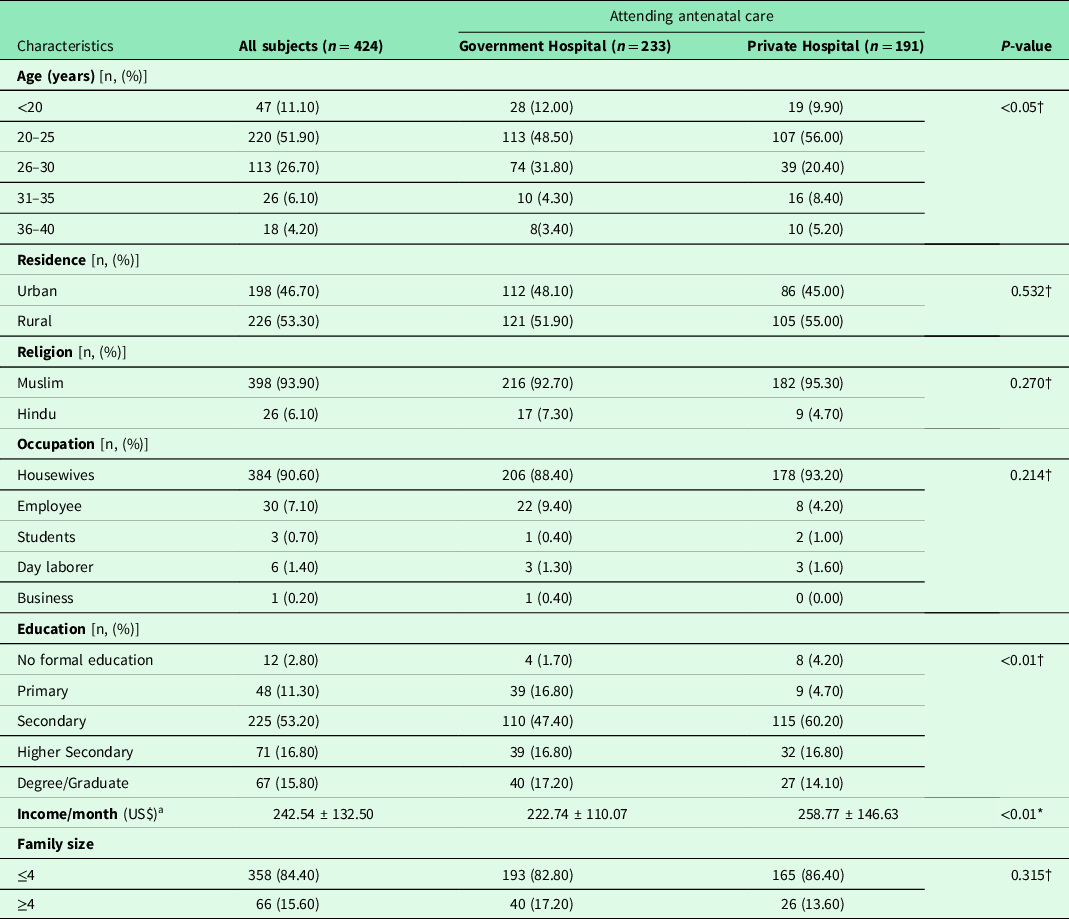
Data are presented as amean ± SD. *P- and † P-values were from the independent sample-t test and the chi- squared test, respectively.
Obstetric and maternal characteristics
Among all pregnant women, 225 (53.10%) were multigravid, half of the pregnant women were without child, 213 (50.20%), and women with one child, 145 (34.20%). More than half of the pregnant women, 293 (69.10%) were in third trimester (gestational age more than 24 weeks). The gestational age of the study subjects was 3.90%, 18.80%, and 77.30% in attending government hospitals and 3.10%, 37.70%, and 59.20% in attending private hospitals in first, second, and third trimesters, respectively. Except abortion, all obstetric and maternal characteristics were found at different levels of significance between the participants attending the two types of hospital (Table 2).
Table 2. Obstetric and maternal characteristics of the study participants

†P-value was from the chi-squared test.
Medical and physical characteristics
The average BMI (mean ± SD) of the study subjects were attending in government and private hospitals was 19.33 ± 2.47 and 21.76 ± 3.18 kg/m2, respectively, which is significantly (P < 0.001) higher in attending in private hospitals (Table 3). Most of the study subjects’ body temperature (°C), pulse rate (bpm), blood pressure (mmHg), and conjunctival color were normal and have no medical illness (Table 3).
Table 3. Medical and physical findings of the study participants

aMean ± SD, *P- and †P-values were from the independent sample-t test and the chi-squared test, respectively.
Dietary characteristics
Everyday, animal products and green leafy vegetables consumption by participants was 136 (32.10%) and 368 (86.80%). More than half of the participants, 216 (50.90%) consume fruits after meal. More than half, 244 (57.5%) of the pregnant women took Fe supplement at the time of the study. The dietary habits showed different levels of significance between the study groups (Table 4).
Table 4. Dietary characteristics of study participants

†P-value was from the chi-squared test.
Prevalence and severity of anemia
Among the pregnant women who were receiving ANC, 265 (62.5%) were anemic according on their hemoglobin (Hb) levels and the rest of 159 (37.50%) did not show anemia (Table 4). The prevalence of anemia of the participants in attending in government hospitals was 160 (68.70%) and private hospitals was 105 (55.0%). The prevalence of mild, moderate, and severe anemia in attending government hospitals was 28.30%, 36.90%, and 3.40% and in private hospitals was 14.70, 39.80, and 0.5%, respectively, and the differences were significant (P < 0.001) (Table 5). Among the anemic pregnant women, the severity of anemia was significantly associated with occupation (P < 0.001), monthly income (P < 0.01), and obstetrics factors such as gravid and birth interval (P < 0.05) and gestational age (Table 6).
Table 5. Prevalence and degree of anemia of study participants
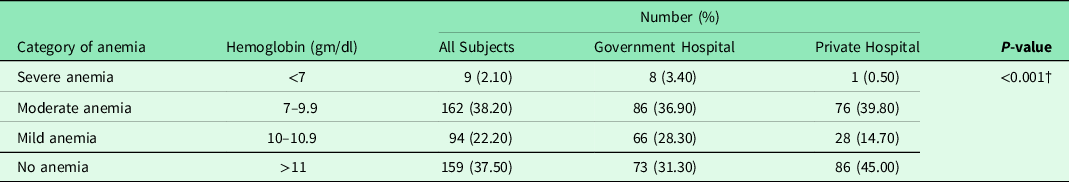
†P-value was from the chi-squared test.
Table 6. Association of risk factors and severity of anemia in pregnancy

†P-value was from the chi-squared test.
Factors associated with anemia
Binary logistic regression model was performed to identify the factors affecting maternal anemia. After adjusted by other variables, being age groups ranged from 20 to 25 years (AOR = 1.9, 95% CI: 1.05–3.59, P < 0.05) and from 26 to 30 years (AOR = 2.374, 95% CI = 1.187–4.747, P < 0.05), monthly family income 301–500 US$ (AOR = 2.761, 95% CI: 1.536–4.960, P < 0.01), attending government ANC (AOR = 2.025, 95% CI:1.268–3.233, P < 0.01) were independent risk factors for anemia. Parity (AOR = 1.925, 95% CI: 1.108–3.342, P < 0.05), gravid (AOR = 1.636, 95% CI: 1.053–2.540, P < 0.05), and contraceptive use [no contraception (AOR = 2.501, 95% CI: 1.598–3.916, P < 0.001)] were significantly associated with anemia. However, iron supplement was protective of anemia [no iron supplement (AOR = 0.649, 95% CI: 0.422–0.998, P < 0.05)] (Table 7).
Table 7. Effect of different risk factors on prevalence of anemia among pregnant women

Results were derived from binary logistic regression analysis. 1 = Reference; AOR = adjuster odds ratio; CI = confidential interval; a = mean ± SD. P < 0.05 statistically significant association for the adjusted odds ratio.
Discussion
The prevalence of anemia among pregnant women in this study was 62.5%. Out of 265 anemic subjects, 22.2% were mild, 38.2% moderate, and 2.1% were severely anemic. To our knowledge, this is the first study to compare the prevalence of anemia in two types of hospitals in Bangladesh. Maximum studies were conducted either at specialist or general hospitals and rural community-level hospitals in this area (Chowdhury et al., Reference Chowdhury, Ahmed, Jebunessa, Akter, Hossain and Shahjahan2015; Rahman et al., 2018; Ahmed et al., Reference Ahmed, Mamun, Mahmud, Farzana, Sathi, Biswas, Datta and Ahmad2019). We found that the prevalence of anemia among pregnant women attending ANC in government hospitals was 68.70% and private hospitals were 55.0%, and the difference was (P < 0.001) significant (Table 1). Participants attending government hospitals (AOR = 2.02, 95% CI: 1.26–3.23, P < 0.01) were 2.02 times higher risk of anemia than attending private hospitals (Table 7). This result indicates that patients attending government hospitals were not well concerned about their health, and as a result, the chance of getting anemic is higher than the patients attending private hospitals. This finding is similar to a study conducted in Uganda (Obai et al., Reference Obai, Odongo and Wanyama2016) and Ethiopia (Jufar and Zewde, Reference Jufar and Zewde2014). The ANC management is like any other case, but more frequent visits are required (Sharma and Shankar, Reference Sharma and Shankar2010).The prevalence of mild, moderate, and severe anemia in attending government hospitals was 28.30%, 36.90%, and 3.40% and in private hospitals was 14.70%, 39.80%, and 0.5%, respectively, which differences were (P < 0.001) significant (Table 5). Most of the severe anemic patients were from the government hospital. These patients have very poor socio-economic conditions. As a result, they cannot afford the treatment that was advised. In this study, among the participants, the majority of anemic cases were moderately anemic, 38.32% followed by 22.2% mild and 2.10% were severely anemic. The severe anemia recorded in this study is similar to the 2% reported in Ilesha and Rivers State of Nigeria (Komolafe et al., Reference Komolafe, Kuti, Oni and Egbewale2005; Geraldine and Paul, Reference Geraldine and Paul2012). Another study at Marie Stops clinic, Dhaka city, Bangladesh showed no severe anemic subjects (Chowdhury et al., Reference Chowdhury, Ahmed, Jebunessa, Akter, Hossain and Shahjahan2015). Our study has shown converse findings compared with those of Bangladeshi studies because the majority of subjects of our study leaving in rural areas and suffering from poverty and a higher prevalence of iron deficiency anemia (Bodner et al., Reference Bodnar, Cogswell and Scanlon2002). The results of our study showed that subjects with lower per capita family income were more anemic than the higher one which is a significant (P < 0.01) difference between the study groups. In this study, majority of the respondent belongs to less than 300 US$. Participants who had family monthly income (US$) (301 to 500) [AOR (95% CI) = 2.761 (1.536–4.960), P < 0.01] were less likely to be anemic as compared to those with a monthly family income (US$) (100–300). A study in Pakistan showed that patients with a monthly family income less than Rs 5000 had a hemoglobin value of 1 g/dl lower than those with monthly income of greater than Rs 5000 (Rukhsana et al., Reference Rukhsana, Nabia, Malik, Mobeen, Tara and Shan2009). Another study in Bangladesh reported that the prevalence of anemia was the highest among the low-income group and with the increase of income the prevalence decreased to 20% (Rahman et al., Reference Rahman, Nessa, Yesmin, Rahman and Rahman2018). Generally, the low monthly income disturbs the household food purchasing capacity while affecting the food security to high risk of nutritional deficiencies (Ahmed et al., Reference Ahmed, Mamun, Mahmud, Farzana, Sathi, Biswas, Datta and Ahmad2019). Previous studies have shown an association of anemia with low education status (Balarajan et al., Reference Balarajan, Ramakrishnan, Ozaltin, Shankar and Subramanian2011; Jufar and Zewde, Reference Jufar and Zewde2014; Chowdhury et al., Reference Chowdhury, Ahmed, Jebunessa, Akter, Hossain and Shahjahan2015; Obai et al., Reference Obai, Odongo and Wanyama2016). Although education levels were significantly (P < 0.01) different between the study groups but we did no found association with anemia. Several studies have been found that age was significantly associated with anemia during pregnancy (Milman et al., Reference Milman, Bergholt, Byg, Erikson and Gradual1999; Cusick et al., Reference Cusick, Mei, Freedman, Looker, Ogden, Gunter and Cogswell2008) This current study has observed that only age group (20–25) years (AOR = 1.94, 95% CI: 1.052–3.596) and (26–30) years (AOR = 2.37, 95% CI: 1.18–4.74) were significantly (P < 0.05) associated with anemia. Similar results found that a study conducted in Pakistan and reported that young women between (20–30) years were anemic during pregnancy (Khaskheli et al., Reference Khaskheli, Baloch, Sheeba, Baloch and Khaskheli2016).
Obstetric and maternal characteristics are known important determinants of anemia (Jufar and Zewde, Reference Jufar and Zewde2014). The obstetric variables were different levels of significance (P < 0.001 and P < 0.01) between the study groups. Anemia was 1.92 times more prevalent in multipara (AOR = 1.92, 95% CI: 1.108–3.342, P < 0.05) and 1.63 times in multigravid (AOR = 1.63, 95% CI: 1.05–2.54, P < 0.05), respectively. Although a study conducted in Addis Ababa Ethiopia reported that increased presence of anemia with a short birth interval (Jufar and Zewde, Reference Jufar and Zewde2014), but our study found no association between birth interval and anemia which is in agreement with other studies (Obai et al., Reference Obai, Odongo and Wanyama2016). Our study showed that the prevalence of anemia was highest (68.30%) during the third trimester as compared with the second (27.20%) and first trimester (4.50%). This might be due to hemodilution and also indicate poor prenatal care and nutrition. These findings agree with that of Turkey (Karaoglu et al., Reference Karaoglu, Pehlivan, Egri, Deprem, Gunes, Genc and Temel2010), but are different from those from Porto Novo, Cape Verde, and Abeokuta, Nigeria (Idowu et al., Reference Idowu, Mafiana and Sotiloye2005; Okeke, Reference Okeke2011). The anemia risk increases with the age of a pregnancy (trimester), due to iron demand reaches 6.6 mg/day in the third trimester (Khaskheli et al., Reference Khaskheli, Baloch, Sheeba, Baloch and Khaskheli2016). Our study shows a significant association between anemia and contraception (no contraception (AOR = 2.5, 95% CI: 1.59–3.91, P < 0.001), which is consistent with the study in Addis Ababa Ethiopia (Jufar and Zewde, Reference Jufar and Zewde2014). Another study suggests that anemic subjects must use an effective contraception method and should not conceive for at least 2 years giving time for iron stores to recover (Sharma and Shankar, Reference Sharma and Shankar2010). This study showed that the physical factors of the participants were different levels of significance (P < 0.001 and P < 0.01) between the study groups (Table 3). Our study suggested the dietary habits of the study participants who were receiving ANC at government and private hospitals were significantly (P < 0.001) different (Table 3). We found that the subjects who visited government hospital have low BMI and inadequate intake of diets compared to the subjects of private hospital. This result indicates that eating green vegetables, fruits, and animal products helps to reduce the risk of anemia in the pregnancy period. Pregnant women should eat iron-containing food and vitamin-c-rich foods to enhance iron absorption and also mature the folic acid from dihydrofolate to tetrahydrofolate (Woldemariam et al., Reference Woldemariam, Timotiows, Girma and Genebo2002). The nutritional status of iron depends on the ingestion of adequate amounts of iron in the diet or through iron supplementation (Sharma and Shankar, Reference Sharma and Shankar2010). The sanitary effect of iron supplementation on improvement of hemoglobin levels in pregnancy has been documented in various studies (Khambalia et al., Reference Khambalia, O’Connor, Macarthur, Dupuis and Zlotkin2009; Alem et al., Reference Alem, Enawgaw, Gelaw, Kena, Seid and Olkeba2013), which is similar to our study. We also found significant association between iron supplement and anemia [no iron supplement (AOR = 0.64, 95% CI: 0.42–0.99, P < 0.05)]. Thus, this finding indicates that the pregnant women in the study attend ANC late or insufficient in pregnancy, may be a high prevalence of anemia due to iron deficiency. It is recommended to improve the ANCs that have been taken in the government hospital. As pregnancy is a critical stage for a woman, we highly recommended that the people should take extra care apart from the treatment received from the hospital so that they can prevent the life treating risk of anemia. However, this study did not show a significant association between anemia and occupation, mother’s education level, family size, residence, history of blood loss, but previously statistically significant associations were reported in different studies. It was an institutional-based study, which means that the results cannot be extrapolated to the whole population. Further study should be conducted based on a community level to make this finding stronger. We did not consider the other factors such as, malaria, parasitic infection that can lead to anemia. The actual diet of the participants was not investigated. We were therefore not able to determine their contribution to anemia in our study population. Being a cross-sectional study, therefore, we could not identify the cause-and-effect relationship.
Conclusions
The findings in this study demonstrate that the prevalence of anemia in pregnant women attending ANC in governmental hospitals was higher than in private hospitals. In the current study, we found overall high prevalence of anemia and the majority of them were moderate-type anemia (Hb level: 7–9.9 g/dl). The severity of anemia in this study has shown a statistically significant association with occupation, monthly family income, gravity, birth interval, and gestational age. Among pregnancy women, being an early age group woman, low family income group, high parity, and high gravity, attending ANC at governmental hospitals, without contraceptive use, and no iron supplements are independent risk factor for anemia. Therefore, it is recommended to improve the socioeconomic status, diversifying food intake including iron-rich foods and iron supplementation of pregnant women. Greater efforts are required to encourage early antenatal attendance for these at risk pregnant women. Moreover, using family planning methods and to enhance maternal health nutrition education intervention is highly recommended to potentially reduce the prevalence of anemia during pregnancy.
Acknowledgments
We thank all subjects attending antenatal care who voluntarily participated in this study. We are thankful to the management and staff of respective hospitals for allowing us to carry out this research.
Financial support
This study received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None of the authors have competing interests
Authors’ contribution
BSA and MSI designed the study. BSA, MSI, and MRK contributed to data collection and analysis. All the authors contributed to the drafting of manuscript and approved the final version for publication.












