Crossref Citations
This article has been cited by the following publications. This list is generated based on data provided by
Crossref.
Manero, Albert
Smith, Peter
Koontz, Amanda
Dombrowski, Matt
Sparkman, John
Courbin, Dominique
and
Chi, Albert
2020.
Leveraging 3D Printing Capacity in Times of Crisis: Recommendations for COVID-19 Distributed Manufacturing for Medical Equipment Rapid Response.
International Journal of Environmental Research and Public Health,
Vol. 17,
Issue. 13,
p.
4634.
Chen, Quan -wen
and
Gong, Ping
2021.
e-Learning, e-Education, and Online Training.
Vol. 389,
Issue. ,
p.
381.
Sang, Yajie
and
Lv, Haibin
2021.
Interactive Innovation Research on Film Animation Based on Maya-Unity Animation Simulation of Visual Sensor.
Journal of Sensors,
Vol. 2021,
Issue. ,
p.
1.
Li, Guangsong
and
Arif, Muhammad
2022.
Virtual Garment Piece Design and Stitching Algorithm Based on Virtual Simulation Technology.
Security and Communication Networks,
Vol. 2022,
Issue. ,
p.
1.
Gaballa, Aya
Cavalcante, Reidner Santos
Lamounier, Edgard
Soares, Alcimar
and
Cabibihan, John-John
2022.
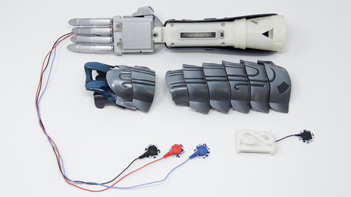
Extended Reality “X-Reality” for Prosthesis Training of Upper-Limb Amputees: A Review on Current and Future Clinical Potential.
IEEE Transactions on Neural Systems and Rehabilitation Engineering,
Vol. 30,
Issue. ,
p.
1652.
Li, Na
2023.
Proceedings of the 2nd International Conference on Cognitive Based Information Processing and Applications (CIPA 2022).
Vol. 156,
Issue. ,
p.
341.
Thomas, K.T.
Jacob, Lija
and
Shukla, Samiksha
2023.
The Role of AI, IoT and Blockchain in Mitigating the Impact of COVID-19.
p.
26.
Li, Wei
Shi, Ping
Li, Sujiao
and
Yu, Hongliu
2024.
Current status and clinical perspectives of extended reality for myoelectric prostheses: review.
Frontiers in Bioengineering and Biotechnology,
Vol. 11,
Issue. ,
McLinden, Shea
Smith, Peter
Dombrowski, Matt
MacDonald, Calvin
Lynn, Devon
Tran, Katherine
Robinson, Kelsey
Courbin, Dominique
Sparkman, John
and
Manero, Albert
2024.
Utilizing Electromyographic Video Games Controllers to Improve Outcomes for Prosthesis Users.
Applied Psychophysiology and Biofeedback,
Vol. 49,
Issue. 1,
p.
63.