No CrossRef data available.
Article contents
Expression of Acute Phase Protein, Glial Fibrillary Acidic Protein, Epithelial Cadherin, and S100 Protein in Brain Tissues from Natural Cases of Ovine Encephalitic Listeriosis
Published online by Cambridge University Press: 24 May 2021
Abstract
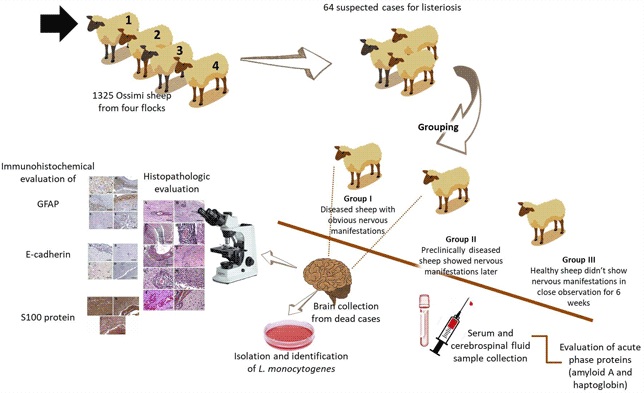
Listeriosis is a disease that is induced by infection with the Gram-positive bacterium Listeria monocytogenes. Much is still unknown about the pathogenesis of encephalitic listeriosis. We aimed to identify the contribution of glial fibrillary acidic protein (GFAP), epithelial cadherin (E-cadherin), S100, and acute-phase proteins (APPs) in pathogenesis, clinical and preclinical diagnosis of natural cases of encephalitic listeriosis. Of 1,325 Ossimi sheep, 64 were suspected of having listeriosis from 2018 to 2020. Prospective cohort evaluation of clinical and postmortem findings was performed, in addition to bacterial isolation, the measurement of APPs in serum and cerebrospinal fluid (CSF), and the histopathological and immunohistochemical evaluation of GFAP, S100, and E-cadherin. Infected sheep showed nervous symptoms ranging from neck stretching to complete paralysis. APPs were significantly increased in the CSF of both clinically and preclinically diseased animals; however, serum APPs were only significantly increased in clinically diseased animals. Histopathological evaluation revealed microabscesses, meningoencephalitis, and perivascular cuffing of the brainstem of infected sheep. Immunohistochemical investigations revealed strong expression of GFAP and S100 in necrotic areas and negative expression of E-cadherin. The measurement of CSF APPs could be useful in the preclinical diagnosis of sheep listeriosis. GFAP and S100 proteins could be involved in the pathogenesis of listeriosis; however, E-cadherin does not appear to be involved.
- Type
- Biological Applications
- Information
- Copyright
- Copyright © The Author(s), 2021. Published by Cambridge University Press on behalf of the Microscopy Society of America





