Introduction
Balloon catheter dilatation treatments have resulted in successful outcomes in various specialties and have been used in many regions of the human body. Balloons were first introduced into otorhinolaryngology in 2005 for use in treating the sinus ostia, with encouraging patient outcomes.Reference Poe and Hanna 1
Eustachian tube dysfunction has been referred to as a ‘black box’ because of the poor knowledge of its pathophysiology.Reference Schroder, Lehmann, Ebmeyer, Upile and Sudhoff 2 Understandably, the mechanisms that underlie the efficacy of eustachian tube balloon dilatation have yet to be determined. Possible hypotheses previously proposed by McCoul and Anand include: submucosal microhaemorrhages, resulting in fibrosis that expands the cross-sectional diameter as the tissues heal; fibrocartilaginous cartilage of the eustachian tube retaining a ‘memory’ of dilatation more than hyaline cartilage would; improvement of epithelial ventilation through a transient reduction in mucosal oedema, permitting the recovery of mucociliary flow; and the initiation of a local signalling pathway within the mucosa that modulates the function of cartilage and muscle.Reference McCoul and Anand 3
Despite an increasing number of technological advances, access to the eustachian tube remains challenging. Furthermore, a number of key anatomical structures lie close to the eustachian tube, which, if damaged, could result in serious morbidity or mortality. Several senior otologists have warned against surgical procedures on the eustachian tube because of a lack of high-level evidence of efficacyReference Bluestone 4 and previously reported mortality from procedures in the eustachian tube region.Reference Poe 5
Balloon dilatation of the eustachian tube can be performed via two approaches: transnasally, which is the more common and well known; or transtympanically, which has limited and conflicting evidence to support its use to date.
Various authors have asserted that the cartilaginous portion of the eustachian tube is the most likely site of pathology in eustachian tube dysfunction,Reference Adil and Poe 6 , Reference Miller and Elhassan 7 and this has certainly correlated with histopathological analysis of the region.Reference Kivekas, Chao, Faquin, Hollowell, Silvola and Rasooly 8 Limiting dilatation techniques to the cartilaginous portion has the added safety advantage of an increased distance buffer from the carotid artery. However, a competing school of thought is that both the cartilaginous and bony portions should be targeted in balloon dilatation of the eustachian tube.Reference Ockermann, Reineke, Upile, Ebmeyer and Sudhoff 9 The bony portion was certainly the primary target of historical surgical approaches,Reference House, Glasscock and Miles 10 which were later abandoned given the morbidity associated with the approach.
Increasing the minimum cross-sectional area should be the main objective in eustachian tube dilatation, as it is with almost all other clinical applications of balloon dilatation catheters. A group of researchers from Pittsburgh used three-dimensional computer-aided reconstructions of histological slides to accurately measure the eustachian tube dimensions.Reference Miura, Sando, Balaban, Takasaki and Haginomori 11 , Reference Sudo, Sando, Ikui and Suzuki 12 The minimum area was consistently found in the lateral aspect of the cartilaginous portion of the eustachian tube, within 5 mm of the junctional portion, with great variation found amongst the 16 specimens. The results of the studies have been combined and are graphically represented in Figure 1. Given these data, it is likely that reaching the narrowest point of the eustachian tube may not be possible transnasally using current equipment and techniques.
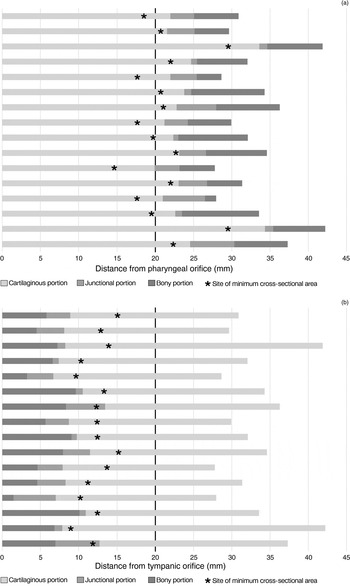
FIG. 1 Graphical representation of adult temporal bone data from the Pittsburgh research group papers, combined.Reference Miura, Sando, Balaban, Takasaki and Haginomori 11 , Reference Sudo, Sando, Ikui and Suzuki 12 Data represented are plotted in terms of: (a) distance from pharyngeal orifice, indicative of a transnasal approach for eustachian tube balloon dilatation; and (b) distance from tympanic orifice, indicative of a transtympanic approach for eustachian tube balloon dilatation.
The two most commonly used catheters in eustachian tube balloon dilatation in previous studies vary in length from 16–24 mm, with the most commonly used length being 20 mm.Reference Randrup and Ovesen 13 It is evident from Figure 1a that a 20 mm balloon catheter inserted transnasally would not reach the position of the minimum cross-sectional area in 50 per cent of the specimens examined. Even a 24 mm catheter would not have reached the minimum cross-sectional area in 13 per cent of specimens, and this is rarely used. Failure to incorporate the minimum cross-sectional area may be one reason for the failure rate of the transnasal approach.
The only ways to overcome this limitation of the transnasal approach are to employ longer balloons or to insert the balloons more laterally. Given the variable anatomy demonstrated in Figure 1, this would be unsafe because of the potential for damage to critical structures.
One possible solution is to consider a transtympanic approach for eustachian tube balloon dilatation. This approach could reliably incorporate the minimum cross-sectional area into the dilated region, and the critical structures are directly visualised and could be avoided. Figure 1b shows the same data represented from the tympanic orifice of the eustachian tube. Although a balloon catheter of 20 mm length would be sufficient for this purpose, a longer balloon could be used to ensure the entire cartilaginous portion is incorporated. Presumably this would not compromise safety, as if the balloon were too long, it would exit the pharyngeal orifice. Furthermore, transtympanic dilatation may be performed concurrently during surgery for chronic ear problems, often carried out because of sequelae of longstanding eustachian tube dysfunction.
Given the potential benefits of the transtympanic approach, this study aimed to systematically review the evidence currently available for transtympanic balloon dilatation of the eustachian tube.
Materials and methods
The databases included in the search, conducted in October 2015, were the Cochrane Library, Medline, PreMedline and Embase. The keyword search terms used were ‘dilation’ or ‘dilatation’, and ‘balloon’ and ‘eustachian tube’. All databases were searched using the full historical range. The study design was required to be original research. The population targeted were either human subjects or cadavers. The intervention was balloon dilatation of the eustachian tube via a transtympanic approach. Studies which solely used the transnasal approach were excluded. There were no exclusions based on comparators or outcome measures. The process of article identification and assessment for eligibility followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (‘PRISMA’) guidelinesReference Moher, Liberati, Tetzlaff and Altman 14 and is described in Figure 2. The risk of bias was assessed with the Cochrane Collaboration's tool for assessing risk of bias.Reference Higgins, Altman, Gøtzsche, Jüni, Moher and Oxman 15
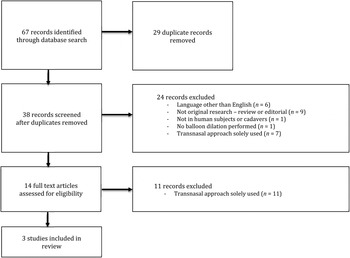
FIG. 2 Results of literature search presented as a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (‘PRISMA’) flow chart.
One investigator completed the screening of the records; however, both investigators reviewed all full text articles independently and discussed any discrepancies until consensus was reached.
Results
There were three studies eligible for inclusion. Each of the studies had a low number of subjects and they were quite disparate in their methods.
The first study investigated balloon dilatation via the transtympanic approach in six human cadavers and reported serious safety concerns.Reference Kepchar, Acevedo, Schroeder and Littlefield 16 Endoscopic visualisation was not employed, necessitating removal of posterior external canal bone until a more favourable angle of view was obtained with the microscope. Four of the six cadavers in this study had sustained head trauma resulting in skull base fractures. In these fractured cadavers, two were unable to have catheters inserted on one side, despite good visualisation of the eustachian tube lumen. The remaining two had catheters inserted into the carotid canal unilaterally and the Vidian canal bilaterally.
The second study investigated transtympanic balloon dilatation of the eustachian tube in human subjects in a limited case series of eight patients.Reference Tarabichi and Najmi 17 All were undergoing simultaneous surgery for either closure of a perforation or removal of cholesteatoma. In all patients, the procedure was safely performed with no intra- or post-operative complications reported. Seven patients reported no pressure symptoms in their ear on follow up, with six of these having good objective medium-term post-operative results. Five patients felt able to perform a Valsalva manoeuvre where they could not pre-operatively, with three demonstrating evidence of insufflation. One patient was lost to follow up.
The third study was also a limited case series, comprising three patients; all had severe eustachian tube stenosis following nasal surgical procedures.Reference Testa, Tamiso, Paris, Testa, Filho and Penido 18 Transnasal balloon catheter dilatation was performed with transtympanic catheterisation and illumination of the eustachian tube for assistance. Although not solely performed transtympanically, this study was included in the review as it combined both approaches. The authors failed to describe any quantitative results or analysis thereof, and used only broad descriptive terms to report positive outcome data and ease of performing the procedure.
Bias was assessed across the three studies and overall the risk of bias was high. Selection bias was not evaluated as the studies were all case series. Performance bias was high risk in all studies as all researchers were aware of the interventions. Detection bias was low risk in the study by Kepchar et al. as the assessment was blinded.Reference Kepchar, Acevedo, Schroeder and Littlefield 16 The other two studies were high risk as outcome assessment was not blinded.Reference Tarabichi and Najmi 17 , Reference Testa, Tamiso, Paris, Testa, Filho and Penido 18 Attrition bias was low risk in all studies. Reporting bias was low risk in the study by Kepchar et al.,Reference Kepchar, Acevedo, Schroeder and Littlefield 16 but high risk in the other two studies.Reference Tarabichi and Najmi 17 , Reference Testa, Tamiso, Paris, Testa, Filho and Penido 18
Discussion
At present, there is a very narrow evidence base for the transtympanic approach for balloon dilatation of the eustachian tube. All three studies identified in this review had significant limitations. It is promising that balloon dilatation of the eustachian tube has been performed transtympanically in one centre in a clinical setting, with no complications and encouraging results.Reference Tarabichi and Najmi 17 However, serious safety concerns were raised in a cadaveric transtympanic study, and these need to be addressed comprehensively. Much research remains to satisfactorily prove the feasibility, safety and efficacy of the procedure before it can be introduced into standard practice.
Transtympanic approach advantages
Given the potential clinical advantages of the transtympanic approach for balloon dilatation of the eustachian tube, it is worthwhile to consider this technique for future procedures.
Full visualisation of the balloon dilatation catheter can be maintained throughout its insertion into the eustachian tube. Continuous visualisation decreases the risk of kinking, confirms deployment of the balloon and decreases the chances of insertion into a false passage, all of which are more likely with blind insertion, as occurs in the transnasal approach.
The region of minimum cross-sectional area can be ensured and the entire cartilaginous portion of the eustachian tube can be dilated. Despite wide anatomical variation, a balloon with a minimum of 20 mm length inserted transtympanically would encompass the minimum cross-sectional area of the eustachian tube. The use of longer balloons would also be possible without concerns for damage to structures at or beyond the distal end.
There is the potential for dual endoscopic visualisation; a transnasal endoscope can also be used to add an increased level of safety to the procedure. This increases certainty that a false passage has not been created and that the balloon is in the exact desired position prior to inflation.
Finally, there is potential for simultaneous surgery to manage chronic ear problems and dilatation of the eustachian tube during the one procedure.
Transtympanic approach disadvantages
There are also a number of disadvantages of the transtympanic approach for balloon dilatation of the eustachian tube.
It is necessary to elevate a tympanomeatal flap for access to the protympanum. A transnasal approach can often be performed without the need for adjunct procedures for access, although a limited number of studies report septoplasty and/or turbinoplasty for access.Reference McCoul and Anand 3 Entering the middle ear carries increased risks of perforation and dysgeusia, as well as rarer ones such as sensorineural or conductive hearing loss, disequilibrium, vertigo, tinnitus, and facial nerve injury.
There is a likelihood of general anaesthetic. Some studies have reported the use of local anaesthetic with the transnasal approach,Reference Catalano, Jonnalagadda and Yu 19 while general anaesthetic would likely be required for transtympanic approaches.
Finally and crucially, there is a risk of carotid artery injury. The proximity of the carotid artery in the usual anatomical configuration, and the possibility of injury to the vessel, is of grave concern in the transtympanic approach to the eustachian tube. It is important to pay due diligence to the carotid artery when considering a transtympanic approach by ensuring the following points are respected: (1) ensuring full endoscopic visualisation of the protympanum is consistently maintained; (2) using dual endoscopic visualisation to confirm entry of the balloon catheter tip into the nasopharynx; (3) carefully avoiding entering any bony false passages, through constant visualisation, and avoiding kinking, resistance and abnormal trajectory of insertion; and (4) ensuring the proximal end of the catheter is situated beyond the carotid prominence on inflation, which will enable avoidance of the region where the carotid is situated closest to eustachian tube lumen. If there are any doubts of compromise, the procedure should be aborted without hesitation.
Future directions and recommendations
Further investigation of the transtympanic technique in cadavers is underway to determine if the safety concerns raised by Kepchar et al.Reference Kepchar, Acevedo, Schroeder and Littlefield 16 can be overcome. Two key modifications that will need to be employed are: the use of cadavers that have not sustained any pre-existing trauma; and the use of endoscopic visualisation at all stages of the procedure, including dual endoscopic visualisation transtympanically and transnasally. Results with these modifications are promising with respect to feasibility, safety and efficacy.Reference Jufas, Treble, Newey and Patel 20 This may provide a level of confidence sufficient to progress to clinical trials.
The authors agree with and strongly emphasise the cautionary sentiments previously expressed by senior otologists with respect to this novel technique.Reference Poe 5 Endoscopic surgical skills will need to be perfected before engaging in more complex applications such as balloon dilatation of the eustachian tube.
Transtympanic balloon dilatation of the eustachian tube is a procedure still in its infancy, yet it shows significant theoretical promise. In the future, appropriately selected patients should be recruited into well-designed studies – either randomised, controlled trials or case–control studies. There will need to be narrow indications and broad contraindications used in the selection criteria. Standard subjective and objective reporting outcomes will need to be used to measure efficacy. These might include audiometry, otoscopy, tympanometry, the ability to perform a Valsalva manoeuvre and completion of a eustachian tube dysfunction questionnaire (e.g. ETDQ-7).Reference Randrup and Ovesen 13 These strict criteria should apply to both the transnasal and transtympanic approaches for balloon dilatation of the eustachian tube, to allow comparisons of safety and efficacy between the two techniques.
Conclusion
Sufficient evidence of the safety and efficacy of transtympanic balloon dilatation of the eustachian tube has yet to be established. There have only been three original research studies conducted on this topic and these report conflicting results. While the technique shows promise, safety concerns remain, and these require careful scrutiny. This would be best achieved with further cadaveric research and well-designed clinical studies.




