Introduction
Granular myringitis, which is also referred to as chronic myringitis, myringitis granulosa, granulomatous myringitis, granulation myringitis and granular external otitis,Reference Devaraja1 is an acute or chronic condition. It is characterised by de-epithelialisation of the tympanic membrane with or without granulation tissue on the outer surface of the tympanic membrane without middle-ear disease. This condition is sometimes confused with otitis externa, chronic suppurative otitis media or a dermatological condition. Most patients with granular myringitis seek medical care with complaints of having itchy ears, aural fullness, otorrhoea or otalgia; however, some patients may be asymptomatic.Reference Levi, Ames, Gitman, Morlet and O'Reilly2 If this condition is not properly treated, it can lead to fibrosis in the external ear, and inflammatory infiltration of the deep canal can lead to ear canal stenosis.Reference Bansal3
Wolf et al. (2006) classified granular myringitis into four grades based on the extent of disease, as follows.Reference Wolf, Primov-Fever, Barshack, Polack-Charcon and Kronenberg4 Grade I: focal de-epithelialisation of the tympanic membrane with the lesion usually covered by a yellowish dry crust. A shallow well-demarcated ulcerative lesion, with or without shallow granulation tissue, is exposed upon peeling back the crust (Figure 1). Grade II: focal, raised, polypoid formation; purulent discharge may be minimal and cover only part of the tympanic membrane (Figure 2). Grade III: diffuse polypoid formation over the entire tympanic membrane. Grade IV: the same as grade III with polypoid formation involving the external auditory canal.
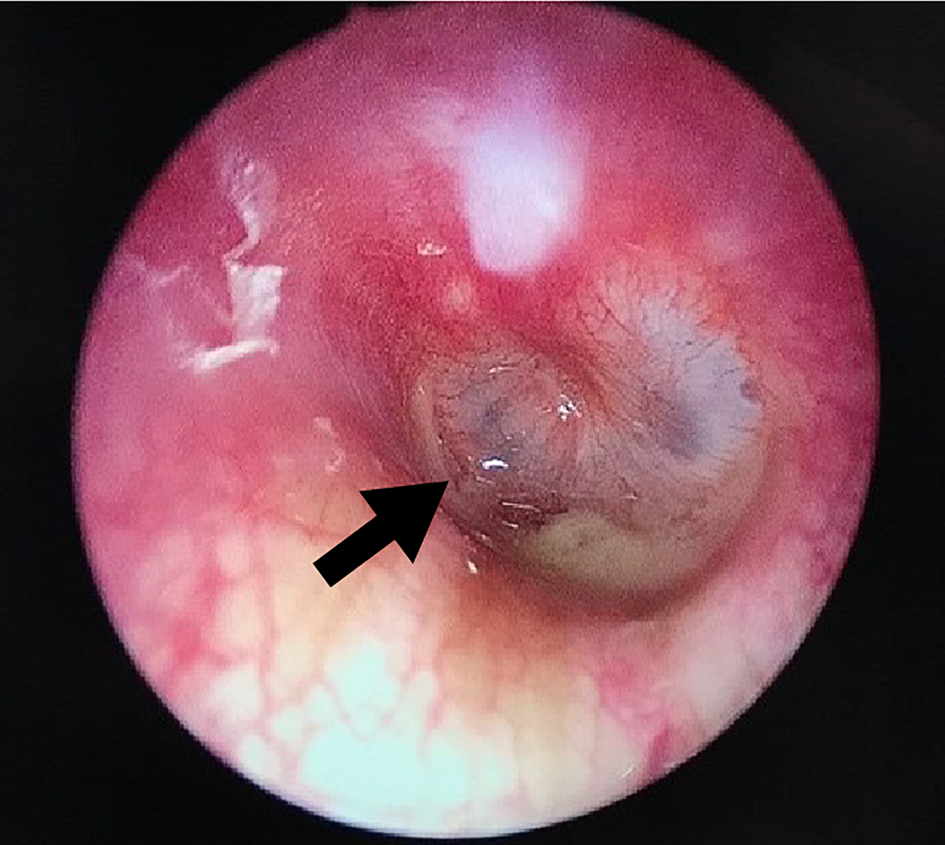
Fig. 1. Endoscopic image showing focal de-epithelialisation (black arrow) of the tympanic membrane.
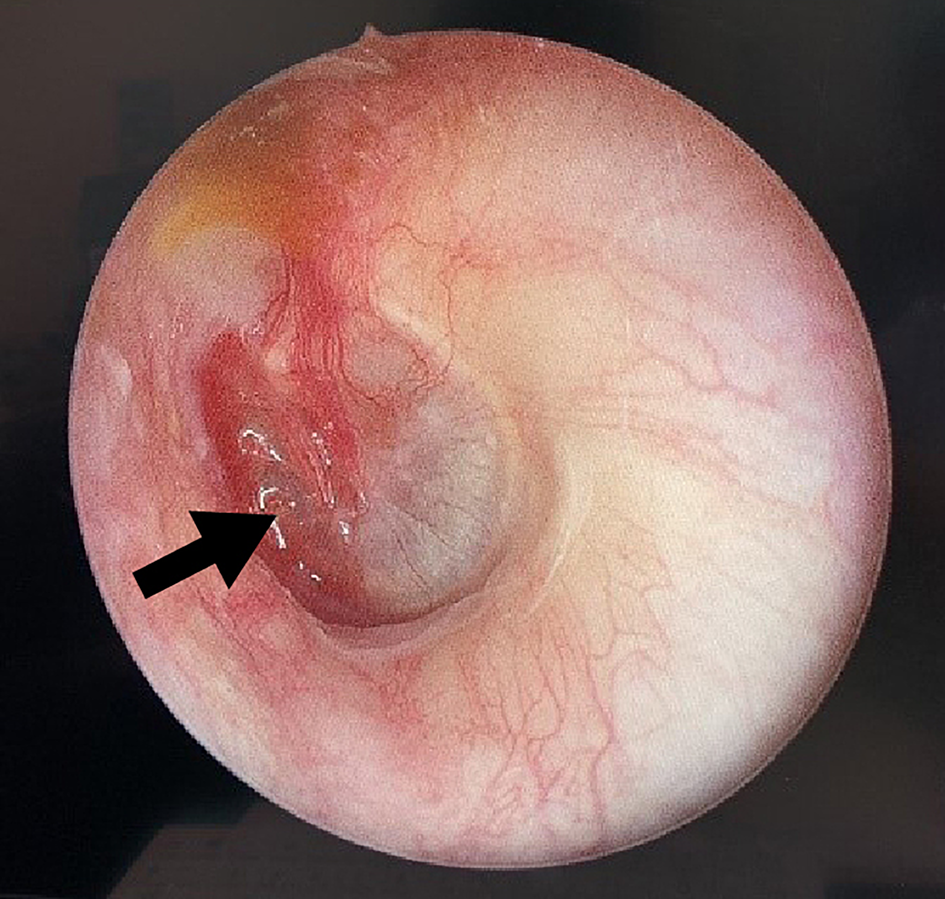
Fig. 2. Endoscopic image showing granulation tissue (black arrow) on the tympanic membrane.
The exact aetiologies and pathophysiology of granular myringitis are poorly understood; however, trauma to the tympanic membrane surface because of repeated ear cleaning or previous surgery appear to be likely aetiologies of granular myringitis.Reference Devaraja1 Other studies suggest that infection processes from bacteria, fungus or a virus instigate the development of granular myringitis. Pseudomonas aeruginosa and Staphylococcus aureus are commonly found from discharge cultures in granular myringitis patients.Reference Devaraja1 Other causes that have been reported include swimming, high-ambient temperature, poor hygiene, local irritants and foreign bodies, as well as skin conditions, such as psoriasis and eczema.Reference Bansal3
There is still no conclusively established treatment guideline for granular myringitis. Current treatment regimens include topical antibiotics, steroid ear drops, diluted vinegar solution, diluted hydrogen peroxide, 5-fluorouracil, Castellani solution, chemical cauterisation and curettage of the granulation.Reference Devaraja1,Reference Chung, Lee and Kim5 The popular topical ear drops used in our institution are topical antibiotics with or without steroids. However, with these formulations, fungal accumulation in the ear canal might sometimes occur.
Bacteria grows best in a pH 6.5–7.5 environment,Reference Jung, Cho, Yoo, Lim and Chae6 and 1 per cent acetic acid can produce a pH 2.5 acidic environment.Reference Agrawal, Sarda, Shrotriya, Bachhav, Puri and Nataraj7 Therefore, 1 per cent diluted vinegar would be beneficial in granular myringitis treatment.
Many studies have reported the benefit of diluted vinegar solution as a treatment for granular myringitis. Jung et al. conducted a case-control study in 2002 that included 30 granular myringitis patients.Reference Jung, Cho, Yoo, Lim and Chae6 That study reported that 80 per cent of patients (12 of 15 patients) who were treated with diluted vinegar had more chance of recovery and resolution of symptoms within 1 week without recurrence after follow-up for 6 months compared with the ofloxacin ear drop group.
van der MeerReference van der Meer8 studied granular myringitis in 2010 and found that 4 per cent acetic acid solution could treat granular myringitis, but its effectiveness was inferior to both 4 per cent hydrogen peroxide and Quadriderm® solution.
Vinegar is an inexpensive organic product that is widely available worldwide. It is derived from sugar and starch fermentation that initially produces ethanol but subsequently produces acetic acid.Reference Budak, Aykin, Seydim, Greene and Guzel-Seydim9 In addition to its use as a food, vinegar is also used for medical purposes. It has antimicrobial properties to destroy both bacteria and fungus, such as P aeruginosa,Reference Budak, Aykin, Seydim, Greene and Guzel-Seydim9 S aureus, klebsiella, acinetobacter, Escherichia coli, Methicillin-resistant S aureus, Proteus mirabilis, Candida albicans, Aspergillus niger and Aspergillus fumigatus.Reference Agrawal, Sarda, Shrotriya, Bachhav, Puri and Nataraj7 The mechanisms of the antimicrobial properties of vinegar include inhibition of the growth of bacteria and fungus by creating an acidic environment, reduction of bacterial protease activity and promotion of wound healing.Reference Agrawal, Sarda, Shrotriya, Bachhav, Puri and Nataraj7
Although many therapies for the treatment of granular myringitis have been evaluated and compared, our review of the literature showed no published direct comparison between 1 per cent diluted vinegar and 1 per cent chloramphenicol ear drops using a randomised controlled study design.
Accordingly, the aim of this study was to compare the outcome of granular myringitis treatment between 1 per cent diluted vinegar and 1 per cent chloramphenicol ear drops and to assess the side effects of 1 per cent diluted vinegar.
Materials and methods
Study design
After obtaining approval from the Siriraj Hospital institutional review board (certificate of approval number: SI346/2018), we started this randomised controlled trial study. The authors included patients diagnosed with and treated for granular myringitis during the 13 June 2018 to 31 December 2019 study period. Written informed consent was obtained from all study participants.
Study population
Twenty-four patients with granular myringitis were enrolled in this study. The inclusion criteria were: (1) being 18 years of age or older, and (2) being diagnosed with granular myringitis grade I or II by an otologist within 90 days of symptom onset. The exclusion criteria were: (1) tympanic membrane perforation greater than 3 mm, (2) allergy to chloramphenicol or acetic acid, (3) prior ear operation within 90 days, and (4) concomitant middle-ear disease.
Study protocol
Diagnosis of granular myringitis was based on clinical examination using microscopic or endoscopic examination. Diagnosis was jointly confirmed by an otologist, and patients who met the criteria were recruited into the study.
Thirty bottles of medication, 15 bottles of 1 per cent diluted vinegar (1 cc of acetic acid combined with 99 cc of sterile water) and 15 bottles of 1 per cent chloramphenicol ear drops, were prepared and randomly numbered 1–30 using the block randomisation technique by the pharmacists who prepared them. Except for the number randomly assigned to each bottle, all other characteristics were exactly the same (Figure 3). The researchers were blinded to the study drug assignment for each patient, and this information was only known to the pharmacists.

Fig. 3. Randomly numbered bottles of 1 per cent chloramphenicol ear drops and 1 per cent diluted vinegar drops that were used in this study.
Patients 1–30 received ear drop medication bottles 1–30, respectively. Local management that was required on a case-by-case basis, such as ear toilet, cauterisation with 85 per cent trichloroacetic acid or application of 2 per cent merbromin solution, was applied as needed at each visit as a standard procedure for local wound care management.
Patients were advised to use their assigned topical ear drops by using four to six drops kept in the ear for five minutes, three times a day. Each patient had a follow-up appointment every 7–14 days for a total of 56 days or until the patient recovered.
Data collection process
Patient data were recorded in a case record form, and patient data confidentiality was maintained. A code was used to identify each patient, but no other forms of identification (e.g., name and hospital number) were used. Recorded information included: (1) demographic data, such as gender, age, underlying disease, history of ear surgery, drug allergy and current medication; (2) clinical presentation, including duration of onset, presenting symptoms, perforation size, grading of myringitis and size of lesion; and (3) follow-up data, including clinical, individual treatment and side effects of treatment.
Outcome measurement
Outcome of treatment was categorised as either ‘recovered’ or ‘not recovered’. Recovered would be documented when physical examination by an otologist showed a completely epithelialised tympanic membrane, without otorrhoea, moistness or subjective complaints. Not recovered would be documented when the tympanic membrane showed de-epithelialisation or granulation tissue. All patients were asked to report any side effects of the use of their assigned study drug.
Sample size calculation
The sample size for this study was calculated using reference data from the study by Jung et al.Reference Jung, Cho, Yoo, Lim and Chae6 That study found that 2 out of 15 patients treated with antibiotic ear drops recovered within 1 week and that 12 out of 15 patients treated with diluted vinegar recovered after 1 week of treatment. The level of significance was set at 0.01 with 80 per cent power of the test. The number of patients per group was 12 patients. The authors increased the size of the sample by 20 per cent (to 15 patients per group) to compensate for withdrawal from the study for any reason.
Statistical analysis
Demographic data and baseline characteristics were summarised using descriptive analysis. The results were reported as frequency and percentage, mean ± standard deviation, or median and interquartile range. Comparison of categorical data, including gender, history of ear surgery, tympanic membrane perforation, grading, size of disease and side effects of treatment, was performed using the chi-square test. The independent t-test was used to compare continuous data (age). The Mann–Whitney U test was used to compare disease duration between groups. Time to recovery was estimated by Kaplan–Meier analysis, and those results were compared between groups using the log-rank test. All statistical tests were considered statistically significant at a p-value of less than 0.05. All data analyses were performed using SPSS® (version 18) statistical software.
Results
Patient characteristics and demographic data
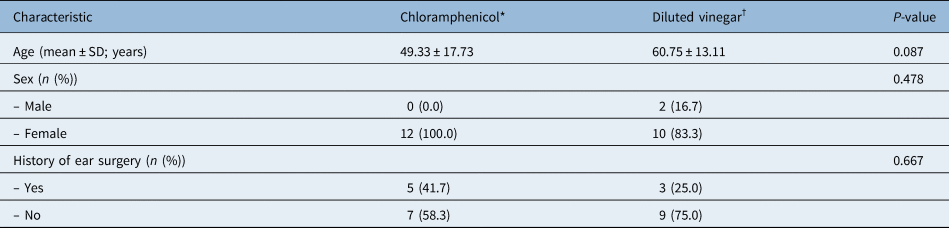
From 13 June 2018 to 31 December 2019, 27 patients were enrolled into this study; however, 3 of those patients were subsequently excluded (1 case was lost to follow-up and 2 cases were found to have middle-ear disease). The remaining 24 patients (22 females and 2 males) completed the study and were included in the final analysis. Twelve female patients were treated with 1 per cent chloramphenicol ear drops, while 2 male and 10 female patients were treated with 1 per cent diluted vinegar solution. The average age of patients was 49.33 ± 17.73 years in the 1 per cent chloramphenicol group, and 60.75 ± 13.11 years in the 1 per cent diluted vinegar group (p = 0.087). Demographic and surgical data of all patients are shown in Table 1. No significant difference between groups was observed for any of the clinical characteristics described in Table 2.
Table 1. Demographic data and surgical history characteristics compared between groups

A p-value <0.05 indicates statistical significance. * n = 12; †n = 12
Table 2. Clinical characteristics compared between groups

A p-value less than 0.05 indicates statistical significance. *n = 12; †n = 12. IQR = interquartile range
Regarding the clinical presentation of granular myringitis, most patients presented with otorrhoea (14 patients, 58.3 per cent), which was characterised as clear discharge, mucoid discharge or mucopurulent discharge. Otalgia was the second most common presentation (11 patients, 45.8 per cent), followed by aural fullness (9 patients, 37.5 per cent) and itching (4 patients, 16.7 per cent). There were 3 patients (12.5 per cent) who were asymptomatic (Table 3).
Table 3. Clinical presentation of myringitis

*n = 24
Therapeutic outcomes
After follow-up for 56 days, complete recovery of granular myringitis was found in 11 patients (91.7 per cent) who were treated with 1 per cent diluted vinegar solution and in 8 patients (66.7 per cent) who were treated with 1 per cent chloramphenicol ear drops (p = 0.156). The average recovery time was 16 days in the 1 per cent diluted vinegar group and 26 days in the 1 per cent chloramphenicol ear drop group. The earliest recovery time was 8 days in the 1 per cent diluted vinegar group (2 of 12 patients) and 15 days in the 1 per cent chloramphenicol group (4 of 12 patients; Figure 4).
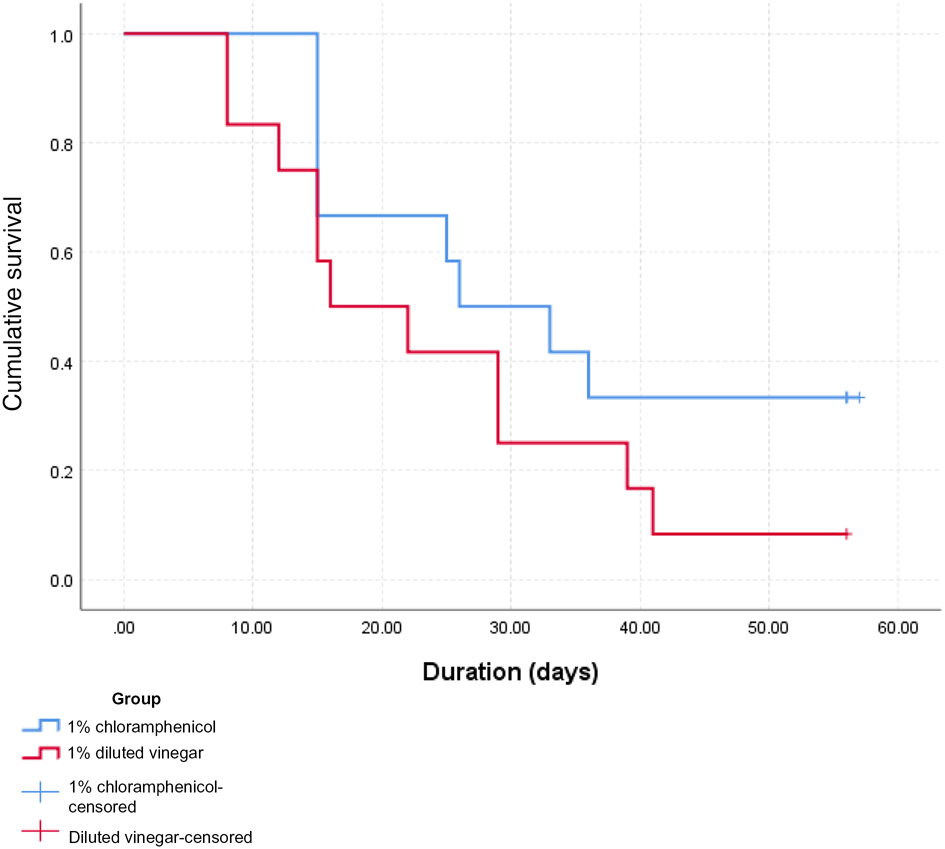
Fig. 4. Kaplan–Meier analysis showing the overall treatment outcome of granular myringitis patients treated with 1 per cent chloramphenicol ear drops (n = 12) or 1 per cent diluted vinegar (n = 12).
During follow-up, 6 of 12 patients (50.0 per cent) in the 1 per cent diluted vinegar group complained of a mild burning sensation and irritation of the external auditory canal, and 8 of 12 patients (66.7 per cent) in the 1 per cent chloramphenicol group had the same complaint. Most patients described this complaint during the early part of the study period, and then the burning and irritation symptoms spontaneously resolved. Only 1 patient (8.3 per cent) treated with 1 per cent diluted vinegar had mild dizziness after using the topical ear drops. No patients in the 1 per cent chloramphenicol group had dizziness. There was no significant difference in the incidence of side effects between groups (p = 0.408 and p = 1.00, respectively). All patients in this study were able to tolerate their assigned treatment protocol. No patients had severe irritation or dizziness. The side effects of treatment are shown in Figure 5.

Fig. 5. A clustered column chart showing the number of patients who had side effects from 1 per cent chloramphenicol and 1 per cent diluted vinegar treatment.
Patients who had tympanic membrane perforation had a longer recovery time than patients who did not have tympanic membrane perforation (39 days vs 15 days; p = 0.017; Figure 6).

Fig. 6. Recovery rate compared between those with and without tympanic membrane perforation.
In this study, duration of onset, history of ear surgery, size of disease and grading of disease were not found to be significantly associated with recovery time (p = 0.520, p = 0.663, p = 0.688 and p = 0.575, respectively).
Discussion
Granular myringitis is diagnosed by presentation of de-epithelialisation of the tympanic membrane or granulation tissue on the tympanic membrane. The aetiology and pathogenesis of this disease is still unclear. One hypothesis is that the rate of desquamation of the tympanic membrane surface exceeds the speed of epithelial cell migration,Reference Levi, Ames, Gitman, Morlet and O'Reilly2,Reference Wolf, Primov-Fever, Barshack, Polack-Charcon and Kronenberg4 and this may cause keratin accumulation with a secondary inflammation reaction.Reference Wolf, Primov-Fever, Barshack and Kronenberg11 Local trauma and infection are also suspected aetiologies. Most clinicians still use antibiotic ear drops as the main treatment to correct granular myringitis.
In this study, we found a far higher prevalence of granular myringitis in women than in men (22 women out of 24 patients, 91.67 per cent). No specific symptom was shown to be a clue for myringitis since most patients (58.3 per cent) in this study presented with otorrhoea, and nearly half of patients had otalgia (45.8 per cent).
At 56 days, complete recovery was found in 11 patients (91.7 per cent) who were treated with 1 per cent diluted vinegar (3 patients recovered at 14 days, another 4 patients recovered at 28 days and another 4 patients recovered at 42 days). Within the same 56-day follow-up period, 8 patients (66.7 per cent) completely recovered in the 1 per cent chloramphenicol group (no one recovered at 14 days, 6 patients recovered at 28 days and another 2 patients recovered at 42 days).
Apart from the number of cured patients, the recovery time in the 1 per cent diluted vinegar group was shorter than that in the 1 per cent chloramphenicol group (8 days vs 15 days, respectively). This showed that the 1 per cent diluted vinegar ear drops seemed to be more effective than the 1 per cent chloramphenicol ear drops for treating granular myringitis, but the difference between groups failed to achieve statistical significance. This insignificant result is probably a result of the small number of participants in each subgroup since the previous positive studyReference Chung, Lee and Kim5 that we used for sample size calculation used a higher concentration of diluted vinegar with the irrigation method.
When we looked at the late recovery group, we observed that patients had tympanic membrane perforation, which suggests that myringitis with tympanic membrane perforation is a severe form of granular myringitis. As such, modification of the granular myringitis grading system should perhaps be considered.
In 2000, El-Seifi and FouadReference El-Seifi and Fouad12 reviewed 94 cases of granular myringitis. They reported that granular myringitis patients treated with antibiotic plus steroid drops followed by 1.5 per cent acetic acid 3 times daily had 100 per cent recurrence. They used a higher concentration of acetic acid than we did in this study, but their treatment results were very disappointing. This might suggest that local wound care, which we provided to every patient at every follow-up visit, is an important component of granular myringitis treatment in addition to topical ear drop treatment.
In 2002, Jung et al.Reference Jung, Cho, Yoo, Lim and Chae6 studied 30 granular myringitis patients in a case-control study, and they reported a marvellous result. Twelve of 15 patients who were treated by irrigation with 40 ml of 1.25 per cent diluted vinegar solution once or twice a day recovered in only 1 week. However, they excluded patients with tympanic membrane perforation, a group of patients who demonstrated poor recovery in our study.
• One per cent diluted vinegar can be used for treating granular myringitis
• One per cent diluted vinegar is not different to 1 per cent chloramphenicol ear drops in granular myringitis treatment
• Side effects of 1 per cent diluted vinegar are few and not different to 1 per cent chloramphenicol ear drops
• One advantage of 1 per cent diluted vinegar is no induction of antimicrobial resistance
A 2010 study from IndiaReference Taneja13 investigated the efficacy of 2 per cent diluted vinegar in both chronic otitis externa and myringitis cases. The result of treatment in the myringitis group was quite good with 81.03 per cent of myringitis patients recovering within two weeks. Side effects of treatment were not mentioned in that study.
Many different vinegar solution formulations are currently prescribed around the world. Higher concentration may increase therapeutic effect, but it may also increase irritation. In the present study, we used a lower concentration of diluted vinegar (1 per cent). It is possible that a higher concentration would have yielded a significant difference in complete cure between groups; however, our 1 per cent concentration caused only mild side effects, and there was no significant difference in side effects between the 2 study groups.
To summarise, to the best of our knowledge, this is the first study to compare the efficacy of granular myringitis treatment between 1 per cent diluted vinegar solution and 1 per cent chloramphenicol ear drops using a randomised controlled study design.
Conclusion
The results of this study showed 1 per cent diluted vinegar to be an interesting option for granular myringitis treatment. Other comparative advantages of 1 per cent diluted vinegar include its low price and no induction of antimicrobial resistance.
Acknowledgements
The authors gratefully acknowledge the patients who generously agreed to participate in this study and Miss Julaporn Pooliam and Dr Saowalak Hunnangkul for assistance with statistical analysis. This study was funded by a grant from the Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, Thailand (grant number: R016131060).
Competing interests
None declared