Introduction
Sir William Osler stated ‘the best teaching is that taught by the patient himself’ (Osler Reference Osler1905). Despite many developments in medical education, direct patient contact remains at the heart of clinical education (Spencer Reference Spencer2004). Patient attitudes towards medical students are generally positive, but may be conflicted in certain specialties and lines of questioning, particularly those of an intimate physical and psychological nature (Mol et al. Reference Mol, Peelen and Kuyvenhoven2011). The psychiatric history is by its very nature intimate, and even trainee doctors avoid difficult questions in clinical practice (Read and Fraser Reference Read and Fraser1998). Although much has been written about medical students’ attitudes towards patients with mental illness, less is known of the reverse (Aggarwal et al. Reference Aggarwal, Guanci, Caracci and Concepcion2013).
The benefits to students of encounters with patients are obvious, but the benefits to patients are not so clear (Spencer et al. Reference Spencer, Blackmore, Heard, Mccrorie, Mchaffie, Scherpbier, Gupta, Singh and Southgate2000). Research in clinical settings shows patients generally have a positive attitude towards medical students (Choudhury et al. Reference Choudhury, Moosa, Cushing and Bestwick2006, Sayed-Hassan et al. Reference Sayed-Hassan, Bashour and Koudsi2012, Mol et al. Reference Mol, Peelen and Kuyvenhoven2011, Passaperuma et al. Reference Passaperuma, Higgins, Power and Taylor2008, Townsend et al. Reference Townsend, Marks, Mauger and Miller2003, Thomas Reference Thomas1999). However, this does not translate to all specialities or settings (Mol et al. Reference Mol, Peelen and Kuyvenhoven2011, Haffling and Håkansson Reference Haffling and Håkansson2008). One study showed that up to 40% of patients felt uncomfortable discussing family problems, anxiety or sexual problems with medical students present (Wright Reference Wright1974). These issues appear to be more pronounced in some geographic regions, possibly in part due to cultural differences (Aljoudi et al. Reference Aljoudi, Alsolami, Farahat, Alsaywid and Abuznadah2016, Marwan et al. Reference Marwan, Al-Saddique, Hassan, Karim and Al-Saleh2012a, Temesgen Reference Temesgen2013, Iqbal et al. Reference Iqbal, Bukhamsin, Alghareeb, Almarri, Aldajani and Busaleh2020).
There has been recent increased focus on the patient as consumer, reinforcing the right to decline medical student involvement (Barr et al. Reference Barr, Ogden and Rooney2010). Issues around consent and confidentiality along with issues such as time expenditure and reinforcement of feelings of ill-health have been reported as being the main drawbacks to medical student involvement (Eagles Reference Eagles2011). Some conflicting studies found that the presence of medical students increases patient satisfaction with their care (Cooke et al. Reference Cooke, Galasko, Ramrakha, Richards, Rose and Watkins1996). Patients can benefit from medical student involvement, for reasons including altruism, contribution to medical science, extra clinical time, company, well-being and increasing their own knowledge about their condition (Sayed-Hassan et al. Reference Sayed-Hassan, Bashour and Koudsi2012).
A recent systematic review of psychiatric patients’ attitudes towards medical students found eight studies to date, including 1088 patients from five different countries (Dearman et al. Reference Dearman, Joiner, Gordon and Vince2018). Study methodology included quantitative, qualitative and mixed-methods studies (Dogra et al. Reference Dogra, Anderson, Edwards and Cavendish2008, Tunde-Ayinmode et al. Reference Tunde-Ayinmode, Rajagopalan and Little2002, Black and Church Reference Black and Church1998, Lynoe et al. Reference Lynoe, Sandlund, Westberg and Duchek1998, Santulli, Reference Santulli1993a, Oster et al. Reference Oster, Backstrom, Lantz and Ramklint2015, Doshi et al. Reference Doshi, Acharya and Wall2006, Gundel and Wefelmaier Reference Gundel and Wefelmaier1998). Most patients with mental illness have a positive experience when interacting with medical students. Patients with mental illness appear to largely benefit from student contact, reporting a subjective experience of improved care. About 20% of patients were uncomfortable with medical student interaction (Dearman et al. Reference Dearman, Joiner, Gordon and Vince2018). Studies varied in size and quality as assessed by the authors. One study employed a group interview teaching format which is not widely used in the UK or Ireland (Santulli, Reference Santulli1993b). Another study had medical student effectiveness as a primary outcome rather than patient satisfaction (Black and Church Reference Black and Church1998). Most included studies were small, with the exception of the Swedish study by Oster et al. who recruited 655 adult patients in a cross-sectional, mixed-methods survey (Oster et al. Reference Oster, Backstrom, Lantz and Ramklint2015). They noted that those with previous exposure to medical students were most positive towards medical students, and female patients were noted to be less comfortable with male students and younger students. The importance of consent, and adequate information about the purpose of the presence of a medical student was identified in a qualitative analysis.
Altogether, these findings suggest positive attitudes towards medical students in patients attending psychiatric services, but the evidence base is limited. We wished to validate the findings of the largest and highest quality study to date by Oster et al. by replicating and elaborating on their study in a different country. Our main hypothesis was that patients attending psychiatric services would have overall positive attitudes towards medical students. Other hypotheses were that female patients would be less comfortable with younger, male medical students and that previous involvement with medical students will lead to more positive attitudes towards students (Mol et al. Reference Mol, Peelen and Kuyvenhoven2011, Oster et al. Reference Oster, Backstrom, Lantz and Ramklint2015). Arising from the Oster et al. study, we also wanted to quantify data on patients’ experience of the consent procedure. It is generally accepted that informed consent is required for participation of patients in medical education (Howe and Anderson Reference Howe and Anderson2003). However, one study of 582 patients across various specialties found that 41% of patients reported that this aspect had been neglected at some stage (Lynoe et al. Reference Lynoe, Sandlund, Westberg and Duchek1998).
Methods
Study design
This was a mixed-methods cross-sectional questionnaire survey of adult psychiatric patients attending services across two catchment areas (Kilkenny and Waterford) in the South-East of Ireland. The questionnaire was derived with authors’ permission from one used in a previous similar study (Oster et al. Reference Oster, Backstrom, Lantz and Ramklint2015). That questionnaire was in turn derived from an earlier Canadian study in a non-psychiatric population (Passaperuma et al. Reference Passaperuma, Higgins, Power and Taylor2008). The use of a tool that had already been used in two studies would facilitate comparison between studies. One of the authors (EHK) translated the questionnaire from Swedish to English.
The questionnaire consisted of six questions about comfort with medical student involvement, including questions regarding student age, gender and level of involvement. There were three questions about attitudes towards medical students and two questions regarding experiences of student involvement (see Appendix 1). We added two questions to the original questionnaire specifically around patients’ perception of consent as this was identified as a significant issue in the qualitative analysis by Oster al. (Reference Oster, Backstrom, Lantz and Ramklint2015). Statements were answered on a five-point Likert scale, with ‘1’ representing complete disagreement, ‘3’ partial agreement and ‘5’ complete agreement. There were also two open-ended questions regarding how to improve student involvement in psychiatric care and any other comments. Patient demographic data (gender, age, geographic location, inpatient vs. outpatient and number of interactions with medical students) were collected. The study was piloted on ten patients with no concerns identified.
Convenience sampling was employed by distributing surveys in clinics and wards. Information on the study was provided with the questionnaires, which were filled in anonymously. It was made clear that participation or non-participation would not affect patient care. No inducements were offered. Patients were asked to only complete survey once. Completion of the survey was considered consent to participate. The local research ethics committee granted ethics approval. Surveys were distributed in the first six months of 2018.
Participants
Inclusion criteria were as follows: age over 18, with capacity to consent and who were at the time attending psychiatric services in the region. We aimed to recruit 373 patients. This sample size was based on a 95% confidence interval and a 5% margin of error. This was based on an estimated population size of 10,000 people over the age of 18 attending psychiatric services in the region (HSE 2018, O’Shea and Kennelly Reference O’shea and Kennelly2008).
Data analysis
Quantitative analysis was carried out using SPSS 22 (IBM Corporation, NY) and GraphPad Prism 6 (GraphPad Software, CA). Demographic descriptors are presented as means with standard deviation (SD) or number per group (% of group) where appropriate. Differences on Likert scale scores between subgroups (gender: male/female; past experience of medical students: yes/no; clinical setting: inpatient/outpatient; geographical location: Kilkenny/Waterford) and age were analysed using ordinal logistic regression. Predictor variables were tested to ensure there was no significant multicollinearity using variance inflation factor. As the assumption of proportional odds underpinning the ordinal logistic regression model was violated using all five score responses from the Likert scale, the scale was simplified into a three score response for the purposes of ordinal logistic regression. Scores 1 and 2 representing strong disagreement with a statement and scores 4 and 5 representing strong agreement with a statement were respectively combined. The ‘partial agreement’ score was left unchanged. Following these modifications, the assumption of proportional odds was not violated based on tests of parallel lines.
Qualitative data on the two open-ended questions were explored using thematic analysis. OpenCode 4.03 was utilised to facilitate systematic analysis of the data to saturation using iterative coding (ICT Services and System Development and Department of Epidemiology and Global Health, 2015)
Results
Respondents
A total of 340 patients completed the survey within the study timeframe, giving a 5.3% margin of error. Not all respondents answered all questions, including demographic information. We do not know how many patients were invited to participate, nor how many surveys were distributed. The mean age of responders was 44.8 (16.3). 171 (52.8%, n = 324) were female, and 255 (75.2%, n = 339) were seen in an outpatient setting. The majority, 256 (75.7%, n = 338) had encountered medical students in the past. Summaries of demographic details were similar across the two main catchment areas apart from age. Patients in the Waterford catchment area were significantly older (mean age 47.9 vs 39.0, p < 0.05). Full demographic details are listed in Table 1.
Table 1. Demographic data
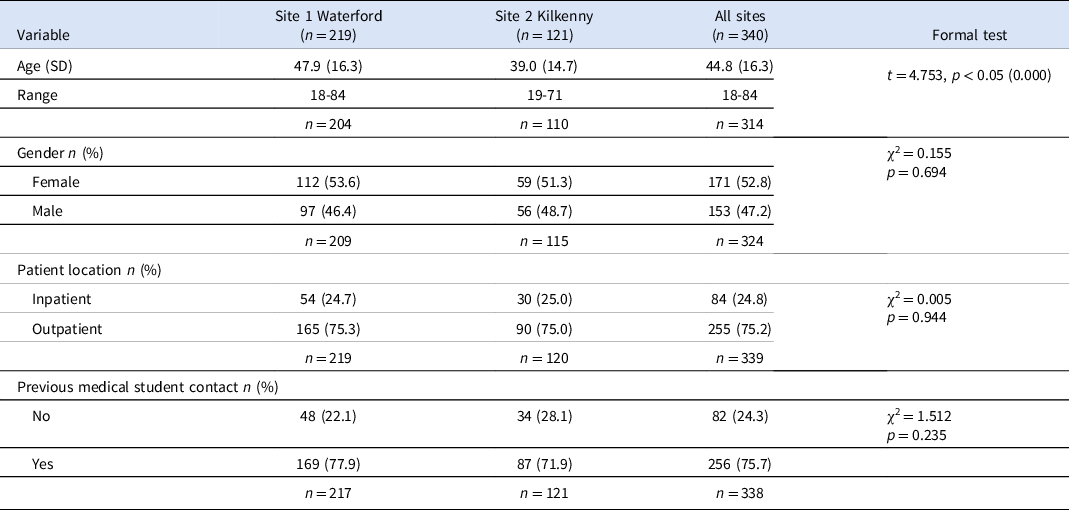
n, number of respondents; SD, standard deviation; t, Student’s t-test; p, p-value; χ2, chi-squared test.
In terms of missing data, this varied from as low as 0.3% (n = 1) for inpatient/outpatient location up to 7.6% (n = 26) for age. For the qualitative analysis, 128 (38%) patients answered the open-ended questions. 75.7% (n = 256) of the respondents had met a medical student in a clinical context. Fig. 1 shows mean Likert scale scores with 95% CI for the twelve questions included in the survey.

Fig. 1 Patients’ comfort levels and attitudes regarding medical students. Figure shows the unadjusted mean (95% CI) response by patients in the entire cohort to a series of statements regarding medical students. The statements were answered on a five-point Likert scale, with ‘1’ representing complete disagreement, ‘3’ partial agreement and ‘5’ complete agreement.
Comfort levels towards medical student participation
Patients had positive attitudes towards student participation, but preferred passive participation. 73.3% (n = 249) agreed that they were comfortable with students present. This fell to 60.3% (n = 205) when the student asked questions with another doctor present and fell further to 41.8% (n = 142) when the student asked questions independently.
Regarding comfort levels based on gender of the medical student, there were no major differences. 72.6% (n = 246) agreed that they were comfortable with the presence of a male medical student, which increased slightly to 77.6% (n = 263) if the student was female. 65% (n = 221) agreed that they were comfortable if the medical student appeared very young. Mean scores for the group are listed in the second column in Table 2.
Table 2. Ordinal regression analysis of patients’ comfort levels with medical students
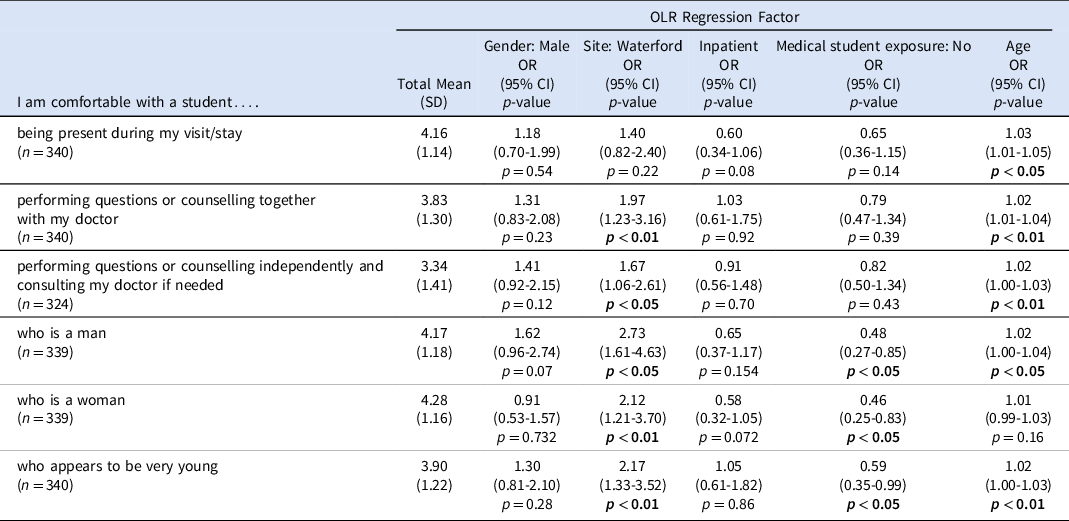
OLR: Ordinal Linear Regression; OR: Odds Ratio.
Ordinal logistic regression was used to analyse any differences in reported comfort levels based on patient gender, study site, inpatient vs outpatient location, previous contact with medical students and age in the model. In terms of comfort levels, the analysis showed no effect of patient gender or whether they were an inpatient or outpatient. Older patients, and those from the Waterford study site, reported higher comfort levels with medical students in general. Patients who had previous exposure to medical students also indicated higher comfort levels on some medical student factors, such as comfort levels on meeting a medical student of either gender or who appeared young, see Table 2 for details.
General attitudes towards medical student participation
83.8% (n = 284) of patients agreed that it is important that medical students meet patients. 64.1% (n = 168) agreed that they would choose to attend a teaching hospital over a non-teaching hospital. 47.2% (n = 158) agreed that the presence of medical students improved the quality of care provided to them. A further 37.9% (n = 127) partially agreed with this statement. The mean scores for the group are listed in the second column in Table 3. In the ordinal regression model, there was no impact of patient gender, study site or whether they were an inpatient or outpatient. Older patients were more likely to agree that the presence of medical students would improve the quality of care provided to them. Patients who had previously met medical students were more likely to agree that it is important for medical students to meet patients during their education, see Table 3 for details.
Table 3. Ordinal regression analysis of patients’ attitudes towards medical students
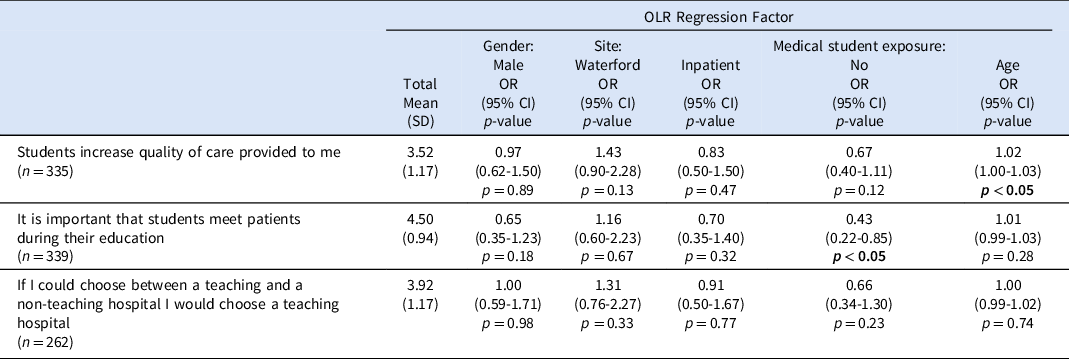
OLR: Ordinal Linear Regression; OR: Odds Ratio.
Experience of consent and meeting medical students
A total of 256 patients had met medical students previously. 68.5% (n = 180) reported they agreed that they had enjoyed their experiences of meeting medical students. A further 24.7% (n = 65) partially agreed. 63.7% (n = 163) agreed that they had been asked for their consent prior to meeting the medical student. 21.9% (n = 56) indicated they partially agreed with this. 39.3% (n = 100) agreed that they were given sufficient information about the medical student prior to meeting them. 37.8% (n = 96) partially agreed. 14.2% (n = 36) indicated they strongly disagreed with this statement. In the ordinal regression model, there was no effect of patient gender or whether they were an inpatient or outpatient. Older patients were more likely to report that they had enjoyed their experiences of meeting student during their care. Regarding consent, the only significant finding was patients in the Waterford study site being more likely to report that they were given sufficient information about the student before meeting them (Table 4).
Table 4. Ordinal regression analysis of patients’ experience of meeting medical students
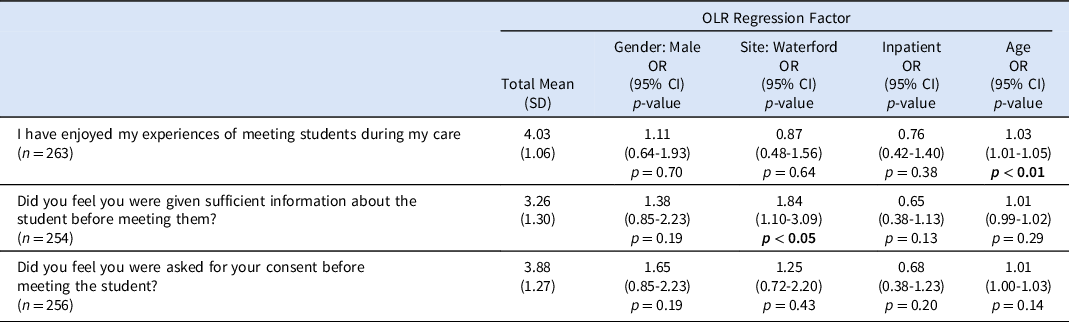
OLR: Ordinal Linear Regression; OR: Odds Ratio.
Qualitative analysis
Data from responses to open-ended questions were analysed together using qualitative content analysis, aided by coding software. Three main themes were identified: information about involvement, conditions during involvement and impact of involvement.
Information about involvement
One of the primary aspects of this theme was patients’ need for advance knowledge of the proposed interaction with the student before presenting. ‘Would prefer to be informed before I go in for appointment that student is present rather than finding out when I arrive in for appointment’.
Pressure of student presence was identified as an issue for information giving and confidentiality. ‘Before sensitive questions ask the student to leave then check with the patient if they feel comfortable with them during questioning’. Patients also identified the need for consent to be obtained without the student present. ‘Being asked without the student present’.
Patients wanted more detailed information about the student’s level of training and previous experience. ‘I would feel more comfortable if they were further on in their training and are more experienced’. Student identity was seen as relevant, to ensure no previous personal relationship. ‘I wouldn’t mind the student as long as I didn’t know them’.
Conditions during involvement
Level of student engagement during the consultation was the most common condition identified by patients during the consultation. ‘Ask questions to make atmosphere comfortable’. Many patients felt that more student interaction would help them feel at ease; however, this was not universal. Patients also identified traits that they would value in a student’s demeanour, using terms such as ‘friendly and compassionate’ or ‘professional’.
Another area highlighted under this theme was communication skills. ‘If they introduce themselves properly and shake my hand’. Student supervision during interactions also emerged as a significant concern for patients, with many expressing the preference to have a trained clinician present throughout. ’Senior doctor/clinician present at all times’.
Impact of involvement
Impact of student presence was expressed positively and negatively, with confidentiality issues, patient acknowledgement of training needs, indirect and direct patient benefits amongst the sub-themes.
Feelings about impact of student involvement on confidentiality tended to be negative, with patients stressing the discomfort that arose from perceived impact of student presence. ‘I understand students need to learn the ropes but I feel uncomfortable even talking to a doctor’.
Respondents recognised the impact of their own involvement on the educational experience as well as acknowledging training needs. ‘I think it’s brilliant to give the student more insight’. Patients also identified positive impacts, with students seen as providing fresh perspective and enthusiasm. ‘I like that students are open-minded and can bring new ideas to the table’. One patient felt that on occasion students had outperformed their clinician regarding comfort levels and engagement. ‘I have been less comfortable with the qualified doctor as I felt no eye contact and human engagement compared to the students’.
Student involvement in patient interactions and care was seen by patients to hold direct benefits, such as additional time. ‘When I was an inpatient, the student had the time to come and talk to me, and that really helped’. Indirectly, patients benefited from observing educational encounters between clinician and student. ‘It’s interesting to hear doctors teaching students for my own information’.
Discussion
This study examined attitudes to medical student involvement of Irish psychiatric patients. Most respondents claimed to be comfortable with students. Older patients reported generally higher comfort levels, and in specific situations, such as different genders or ages of students, as well as higher levels of student participation and autonomy. Higher comfort levels were also seen in patients with previous experience of students. Older patients were most likely to agree that students enhanced the quality of care provided to them and to express enjoyment in meeting students. Patients with previous experience of student involvement were more likely to express agreement that their participation was valuable to the students’ education. The highest agreement scores were in response to the statement ‘It is important that students meet patients during their education’. Patients were least likely to agree that they had been given sufficient information about the student before meeting them, with only 39.3% (n = 100) in agreement. Most patients (63.7%, n = 163) felt they had been asked for consent before meeting the student. In free-text responses, patients stressed the importance of advance knowledge of student involvement, the impact of the student’s presence on the consent process and the patients’ perception of confidentiality.
The only significant demographic difference between the two cohorts of patients involved in this study was age, with patients at the Waterford site being significantly older. Given the significant effect of age in our data, this may explain the differences between geographic locations regarding expressed comfort levels; however, we attempted to correct for this using ordinal regression. These results reinforce the findings of earlier studies which have demonstrated greater acceptance of medical student involvement by older patients (Choudhury et al. Reference Choudhury, Moosa, Cushing and Bestwick2006, Oster et al. Reference Oster, Backstrom, Lantz and Ramklint2015). It is possible that older patients may have experienced more cumulative time within healthcare settings due to failing health and therefore are more likely to have previously encountered a student. This may contribute to the effect of age on our data, as it has been demonstrated both within the results of this study and in previous studies that previous exposure to medical students can positively affect patient perceptions (Lynoe et al. Reference Lynoe, Sandlund, Westberg and Duchek1998, Mol et al. Reference Mol, Peelen and Kuyvenhoven2011, Oster et al. Reference Oster, Backstrom, Lantz and Ramklint2015, Hartz and Beal Reference Hartz and Beal2000). Another possible reason for the disparity in patient attitudes between sites is the established university presence at the Waterford site, which may result in different patient expectations, independent of age.
Previous research has demonstrated a general trend of preference for female students, or gender-concordant student-patient pairings (Passaperuma et al. Reference Passaperuma, Higgins, Power and Taylor2008, Oster et al. Reference Oster, Backstrom, Lantz and Ramklint2015, Marwan et al. Reference Marwan, Al-Saddique, Hassan, Karim and Al-Saleh2012b, Mol et al. Reference Mol, Peelen and Kuyvenhoven2011). In this study, patients did not express any significant preference towards a student of a particular gender. This is encouraging and may be useful from an educator perspective when considering the optimal patient-student pairings for patient comfort. However, older patients and patients with previous exposure to medical students were significantly more likely to agree that they were comfortable with students of either gender. Given the high percentage of patients in this cohort who had previously interacted with students (75.7%) and the findings of previous investigators regarding a gender difference, it may be important to investigate the effect of gender with a wider sample of patients from regional or rural teaching areas, which have less student involvement.
Comfort levels decreased as student involvement and autonomy increased, with lowest comfort expressed in a situation where the student could question or counsel independently without supervision. Qualitative data supported this, with patients expressing a strong preference for some form of student supervision, or a more passive role for the student. Passaperuma et al. (Reference Passaperuma, Higgins, Power and Taylor2008) demonstrated that patients were comfortable with students observing questioning, but less likely to be comfortable with questioning from a student than with the student performing a non-invasive examination (Passaperuma et al. Reference Passaperuma, Higgins, Power and Taylor2008). These findings are supported by our results and have significant implications for medical education in a psychiatric context, given the emphasis on dialogue, trust and rapport in the psychiatric interview. The effect of student participation on patient comfort levels can be managed by continued supervision throughout the interaction, but this may represent an added burden to supervisors.
Patients agreed strongly with the importance of their involvement for the overall learning experience for students, which augments similar previous findings (Haffling and Håkansson Reference Haffling and Håkansson2008, Doshi et al. Reference Doshi, Acharya and Wall2006). However, the more equivocal attitude of patients as to the extent and nature of that interaction poses a difficult dilemma for educational supervisors, which must be examined when designing clinically based educational experiences. Student attitudes and levels of professionalism may play a role in mitigating patient reservations about student participation, and the impact of student demeanour on patient perception has been previously demonstrated (Manninen et al. Reference Manninen, Henriksson, Scheja and Silén2014). The level of information given ahead of interaction with a student has also been shown to impact likelihood to feel comfortable during an encounter with a medical student (Oster et al. Reference Oster, Backstrom, Lantz and Ramklint2015, Hartz and Beal Reference Hartz and Beal2000). Patients in this study were least likely to agree that they had sufficient information about a student prior to encountering them. This suggests that, if given more information about a student prior to engaging with them, patients may be more accepting of deeper student involvement. Patients also emphasised direct and indirect benefits of student involvement in their care, for example increased time and attention, and education about their condition. Patients recognise the contribution that students can make to their care and perceive that students can improve their involvement in decision-making and their knowledge about their conditions (Marwan et al. Reference Marwan, Al-Saddique, Hassan, Karim and Al-Saleh2012b, Mol et al. Reference Mol, Peelen and Kuyvenhoven2011, Dearman et al. Reference Dearman, Joiner, Gordon and Vince2018). The role of the supervisor is vital to educate and encourage patients regarding student participation (Marwan et al. Reference Marwan, Al-Saddique, Hassan, Karim and Al-Saleh2012b, Hartz and Beal Reference Hartz and Beal2000, Tang and Skye Reference Tang and Skye2009). It may be interesting to investigate the effect of supervisor ability to communicate expected extent of interaction and possible benefits of patient engagement with the student.
Strengths of this study are the relatively large sample size and relatively diverse cohort of patients sampling different geographical areas, different acuities of care and with a broad range of patient ages (18-84). Efforts were made to include patients from tertiary and regional centres to ensure as broad as possible a range of patient experiences and previous exposures to medical students.
In this study, the questionnaire was adapted with only minimal changes from one used in a previous Swedish study (Oster et al. Reference Oster, Backstrom, Lantz and Ramklint2015). Whilst absolute numbers of participants differed, patient cohorts were otherwise broadly comparable demographically, with similar ratios in both cohorts regarding gender, age and inpatients to outpatients. Cultural context of both studies is similar, sited in affluent Northern European countries with public/private healthcare systems. The Swedish cohort had a slightly higher percentage of participants who had never encountered a medical student (32%) compared to our cohort (24.3%).
Patients in both studies reported high levels of general comfort with the presence of students, and mean score values were highest in both studies for the statement ‘It is important that students meet patients during their education’. Mean scores for all question items regarding comfort and attitudes towards students in the Irish cohort were comparable or higher than the corresponding Swedish scores. This difference may reflect the higher percentage of patients in the Swedish cohort who had never previously encountered a medical student. Overall, the results of this study were broadly comparable with the Swedish paper, validating previous findings and suggesting that within similar cultural contexts, our results may be generalisable. Results may also be applicable to similar clinical contexts and could be considered in other educational settings where students will encounter patients, such as clinical skills teaching in a university setting.
Mixed-methods methodology was adopted, including free-text open-ended questions to ensure patients had the change to expand on answers and provide unique insights into the experience of psychiatric patients have when involved in teaching and learning of medical students.
The study has limitations to acknowledge. Whilst the questionnaire was used previously and allowed for some comparison of results, it is not a validated instrument and therefore any findings must be interpreted with additional caution. The recruitment rate was slightly suboptimal, which may reflect the additional workload imposed on an already overburdened clinical and administrative team. There is a possibility of response bias as no data were captured on non-participants as a result of anonymous questionnaires. Questionnaires were distributed directly before or after the appointment, in the hope of accurate responses and maximising recruitment rates. However, this may have produced a possible implicit pressure for patients to answer positively. There may also have been a bias towards overly positive responses due to social desirability bias. These issues could have been mitigated somewhat by mailing questionnaires to patients and asking them to complete in their own environment; however, it is likely that this would have impacted negatively on both accuracy and recruitment rates.
Conclusions
Psychiatric patients are aware of the importance of clinical interactions and practical learning for medical students but are ambivalent about more extensive or unsupervised student engagement. Patients require information in advance when considering involvement with a medical student and do not wish to be asked for consent in the presence of the student. The benefits to patients of engaging with students are recognised and may represent a possible mechanism which educators can reinforce and encourage patients to interact more meaningfully with students. Medical educators in clinical teaching settings should be aware of the differences in patient perception of students which may result from younger patient age, lack of previous involvement with students or perceived lack of information about the students and the proposed encounter.
Acknowledgements
This paper is dedicated to the memory of the late Seamus MacSuibhne.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Authors’ contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by SA, EHK, DS and EMK. First and subsequent drafts of the manuscript were written by EMK. SA, DS and EHK commented on draft versions and read and approved the final manuscript.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committee on human experimentation with the Helsinki Declaration of 1975, as revised in 2008. The authors assert that ethical approval for publication of this research has been provided by their local Ethics Committee.
Ethics approval
All study procedures were approved by the HSE South-Eastern Area Research Ethics Committee.
Consent to publish
The authors affirm that participants provided informed consent regarding publication of their data.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Availability of data and material
Access to raw data analysed in this manuscript is available from the corresponding author upon reasonable request.
Code availability
OpenCode 4.03 available from https://www.umu.se/en/department-of-epidemiology-and-global-health/research/open-code2/
Conflict of interest
The authors declare that they have no conflicts of interest.







