To the Editor—The subtropical city of Hong Kong has responded to the threat of coronavirus disease 2019 (COVID-19) with a local elimination strategy, Reference Wong, Kwok and Chan1 focusing on preventing virus introductions with border controls and timely application of public health and social measures to control community outbreaks if and when they occur. Reference Cheng, Wong and Chen2,Reference Cheng, Siu and Wong3 As part of the public health response, all confirmed or suspected cases of COVID-19 are isolated in designated public hospitals with isolation beds set up for this purpose. Following the 2003 SARS experience, Reference Seto, Tsang and Yung4,Reference Lee and Ong5 1,400 isolation beds were already available at the start of the pandemic for Hong Kong’s population of 7.5 million. More beds have been added throughout the pandemic, and at present >3,000 isolation beds are available. If COVID-19 cases are identified in patients in nondesignated hospitals, including private hospitals, the standing policy is for those patients to be transferred to the designated hospitals immediately. In addition, the Department of Health routinely traces close contacts of confirmed cases and quarantines them as one of the measures to control transmission in the community. To mitigate the risks posed by COVID-19, 3 private hospitals with nearly 700 beds have developed a 2-stage admission strategy resulting in zero hospital-acquired COVID-19 cases.
Stage 1 of the strategy focuses on screening incoming patients. All patients coming to the hospital are first screened by the appropriate clinical and epidemiological criteria: fever, travel history, occupation, contact with case, or cluster exposure (FTOCC). Any patient meeting 1 or more FTOCC criteria are isolated. All patients who are negative for FTOCC on admission are tested using nucleic acid amplification testing (NAAT). Patients who are FTOCC or NAAT positive are reported to HKDH and are transferred by assigned ambulances to the HKDH isolation facilities. The goal in stage 1 is to not admit even a single COVID-19 case.
Stage 2 of the strategy is to mitigate risks within the hospital. All patients for whom infection is suspected are admitted and isolated in single rooms until all such suspicions are shown to be groundless. This procedure includes patients with symptoms of chest infection, those whose FTOCC status is uncertain, and those for whom admission is needed before the completion of stage 1 procedures. A key reason for this stage 2 strategy is the quarantine requirement: for any positive case of COVID-19 admitted inadvertently, all close contacts will be quarantined. The goal of stage 2 is to avoid such quarantine for any patient or hospital staff during the pandemic. Aggressive contact tracing of any COVID-19 patient admitted or any staff member that is infected from the community is performed in these hospitals as required by the Department of Health.
The numbers of patients seen in the emergency room as day cases and finally admitted as patients are shown in Table 1. All 3 hospitals have been in active service throughout the COVID-19 pandemic. Many SARS-CoV-2 tests have been conducted in stage 1 by the 3 hospitals. As of July 2021, 77 cases of COVID-19 had been successfully transferred to the designated isolation hospitals. In the stage 2 procedures, 1,961 patients had been isolated in single rooms (Table 1). Only 1 patient was subsequently found to be positive for SARS-CoV-2 in hospital A, but no persons were quarantined because adequate infection control measures had been adopted.
Table 1. COVID-19 Infections in 3 Private Hospitals With Data Related to Stage 1 and 2 Procedures and Community Infections of Staff
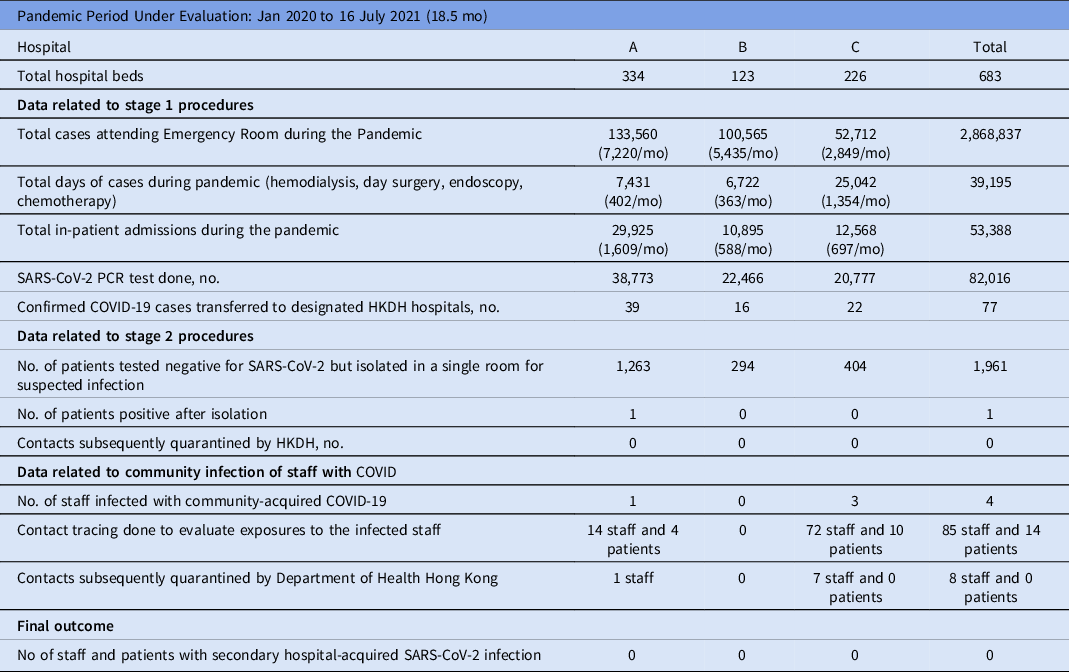
Note. PCR, polymerase chain reaction assay; HKDH, Hong Kong Department of Health.
Table 1 also shows the number of community-acquired SARS-COV-2 infections among hospital staff, which led to substantial contact tracing efforts. Only 2 were clinical staff with patient contact, but appropriate infection control practices were in place and no quarantine of any patient was deemed necessary. In total, 8 staff were quarantined due to exposures to their colleagues, but no secondary infection resulted from these community-acquired infections.
In summary, the measures implemented in these 3 hospitals successfully prevented SARS-CoV-2 transmission. Despite 77 confirmed COVID-19 cases being treated in these hospitals, and only 1 admitted patient under isolation was found to be already infected. In addition, despite very low COVID-19 prevalence in the community, 4 community-acquired infections occurred among staff, but they were all aggressively managed by contact tracing and quarantine as required by the Department of Health, resulting in no secondary cases in these hospitals. This strategy was only possible because the Department of Health required that all confirmed COVID-19 cases be admitted to designated hospitals. The 3 hospitals are still required to ensure that the proper infection control practices are in place for all patient care procedures. Notably, with this strategy, a high number of diagnostic tests are required and sufficient single rooms must be allocated for stage 2. Nevertheless, achieving the result of zero secondary hospital-acquired cases in 3 active acute-care hospitals is a worthwhile accomplishment. This strategy deserves consideration, perhaps with added adaptations in different locations.
Acknowledgments
The authors would like to thank the Hospital Administration of Hong Kong Adventist Hospital and Gleneagles Hospital Hong Kong for their assistance throughout all aspects of the study.
Financial support
No financial support was provided relevant to this article.
Conflict of interest
B.J.C. is a consultant for AstraZeneca, GSK, Moderna, Pfizer, Roche and Sanofi Pasteur. The other authors report no other potential conflicts of interest.






