Impact statement
Life for children and adolescents in South Asia can be challenging, with many reported risks to mental health. For example, various physical (natural disasters and forced displacement), social (crime and neglect), contextual (gender disparity and child labour) and environmental (substance exposure, poor access to services) factors can compromise the well-being of young people. There is also a lack of available services to support children in the face of adversity. Our scoping review intends to improve this situation by investigating what is currently being done to help children and young people in South Asia live well. We provide an overview of mental health risk factors, and focus on community-based intervention as a means of reaching those who are geographically or financially distanced from formal services. We present stories of success, and implications for future work, with task-shifting and stigma reduction methods identified as particularly valuable. These findings provide important information not only for those attempting to boost youth mental health in South Asia, but also for other low-resource settings. Here, approaches that mobilise the local population to address poor mental health and use available resources well can be most effective. We also present information on factors that dictate the feasibility and acceptability of interventions amongst South Asian communities. Our recommendations for practice provide specific detail on how interventions can achieve the greatest likelihood of success, including the use of targeted specialist intervention and comprehensive supervision from professionals. Our recommendations for research cover the increasing development of research capacity in rural locations, the use of strength-based approaches in reducing stigma and additional factors to enhance the feasibility of task-shifting. Collectively, these insights can be applied at the global level, to enhance both research and intervention focusing on the mental health of children and young people.
Introduction
The need to promote youth mental health in South Asian countries is significant and pressing. Globally, there is a lack of sufficient care to meet the mental health needs of children and adolescents (Kieling et al., Reference Kieling, Baker-Henningham, Belfer, Conti, Ertem, Omigbodun, Rohde, Srinath, Ulkuer and Rahman2011), a disparity which is particularly distinct in many of the low- and middle-income countries (LAMICs) in South Asia. Although in some South Asian regions a distinction is drawn between psychiatric disorders (e.g., schizophrenia), externalising disorders (e.g., attention-deficit hyperactivity disorder), internalising disorders (e.g., depression) and neurodevelopmental disorders (e.g., autism), in other locations, all conditions are bracketed under the umbrella term of ‘mental disorders’. The rate of general mental disorders among South Asian children and adolescents ranges from 1.81 to 23.3% (Hossain et al., Reference Hossain, Purohit, Sultana, Ma, McKyer and Ahmed2020). Little research has addressed the prevalence of specific disorders amongst young South Asians; however, one study indicates between 3.9 and 25.4% of adolescents experience suicidal ideation (Aggarwal and Berk, Reference Aggarwal and Berk2015). Autism spectrum disorders (ASDs) affect up to 1 in 93 children (1.1%) across Bangladesh, India and Sri Lanka (Hossain et al., Reference Hossain, Purohit, Sultana, Ma, McKyer and Ahmed2020). The prevalence of ASD amongst children and adolescents in Pakistan, Nepal and Afghanistan is unknown. Substantial variations in prevalence figures indicate that further work is necessary to establish precise estimates for specific disorders and populations.
Whilst mental health infrastructure in these regions is generally lacking (Hanlon et al., Reference Hanlon, Luitel, Kathree, Murhar, Shrivasta, Medhin, Ssebunnya, Fekadu, Shidhaye, Petersen, Jordans, Kigozi, Thornicroft, Patel, Tomlinson, Lund, Breuer, De Silva and Prince2014; Angdembe et al., Reference Angdembe, Kohrt, Jordans, Rimal and Luitel2017), services for young people are particularly underdeveloped. In Bangladesh, Sri Lanka, Nepal and Pakistan, there are no child-specific mental health policies (WHO, 2018; Hossain et al., Reference Hossain, Rahman, Trisha, Tasnim, Nuzhath, Hasan, Clark, Das, Lisako, Mckyer, Ahmed and Ma2021). Additionally, very few psychiatrists offer specialised treatment for children or adolescents in India, Bangladesh, Pakistan, Nepal or Afghanistan (Agarwal, Reference Agarwal2021; Hamdani et al., Reference Hamdani, Huma and Tamizuddin-Nizami2021; Skuse, Reference Skuse2021; Singh et al., Reference Singh, Gupta, Singh, Basnet and Arafat2022; Wang et al., Reference Wang, Feldman, Chkonia, Pinchuk, Panteleeva and Skokauskas2022). Indeed, many countries in South Asia follow the ‘medical model’ of mental health; support is predominantly provided by hospital-based psychiatrists, with very few outpatient or community-based facilities, particularly in Nepal, Pakistan, Afghanistan and Bangladesh. However, these services are more widely available in Sri Lanka and India. Relatedly, with the increasing trend of immigration, relatively poorer South Asian regions suffer from ‘brain drain’, where skilled professionals often migrate to more developed nations (Mullan, Reference Mullan2005), resulting in a lack of psychiatrists, clinical psychologists and social workers (Thara and Padmavati, Reference Thara and Padmavati2013). This phenomenon also leads to a gap in supervising and supporting early career researchers who often need guidance to develop their skills (Sharma and Razzaque, Reference Sharma and Razzaque2017). The lack of mental health specialists for supervision has been identified as a key concern towards capacity building (Eaton et al., Reference Eaton, McCay, Semrau, Chatterjee, Baingana, Araya, Ntulo, Thornicroft and Saxena2011).
Targeting the well-being of young people in South Asia is pertinent, because such a strategy offers benefit beyond childhood and adolescence. A substantial proportion of mental health disorders originates in early life (Kim-Cohen et al., Reference Kim-Cohen, Caspi, Moffitt, Harrington, Milne and Poulton2003; Kessler et al., Reference Kessler, Angermeyer, Anthony, Graaf, Demyttenaere, Gasquet, Girolamo, Gluzman, Gureje, Haro, Kawakami, Karam, Levinson, Mora, Browne, Posada-Villa, Stein, Tsang, Aguilar-Gaxiola, Alonso, Lee, Heeringa, Pennell, Berglund, Gruber, Petukhova, Chatterji and Üstün2007), and interventions to reverse or prevent the effects of cognitive, social and economic deficits reap stronger benefits when delivered to the young (Institute of Medicine and National Research Council, 2000). As such, methods that support the development of lifelong psychosocial resources are a cost-effective route to service provision. Moreover, youth mental health is particularly important in low-resource South Asian regions, because proactively fostering the collective well-being of deprived societies helps to avoid the entrenchment of development problems, and augments global prosperity (Kieling et al., Reference Kieling, Baker-Henningham, Belfer, Conti, Ertem, Omigbodun, Rohde, Srinath, Ulkuer and Rahman2011).
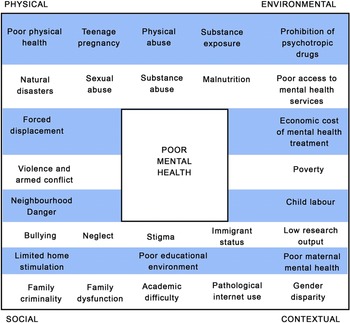
There is a growing evidence base regarding the epidemiology of mental health disorder in children and adolescents across South Asia. Established risk factors for the development of emotional, intellectual and behavioural disorders in LAMIC South Asian settings include low educational stimulation (Arun and Chavan, Reference Arun and Chavan2009), gender disparity (Rudatsikira et al., Reference Rudatsikira, Muula, Siziya and Twa-Twa2007), being orphaned or raised in an institution (Ruiz-Casares et al., Reference Ruiz-Casares, Thombs and Rousseau2009; Erol et al., Reference Erol, Simsek and Münir2010), abuse or neglect (Benjet, Reference Benjet2010) and exposure to trauma including harmful substances (Roy et al., Reference Roy, Bellinger, Hu, Schwartz, Ettinger, Wright, Bouchard, Palaniappan and Balakrishnan2009), violence (Panter-Brick et al., Reference Panter-Brick, Eggerman, Gonzalez and Safdar2009), armed conflict and war (Qouta et al., Reference Qouta, Punamäki, Miller and El-Sarraj2008; Harel-Fisch et al., Reference Harel-Fisch, Radwan, Walsh, Laufer, Amitai, Fogel-Grinvald and Abdeen2010; Layne et al., Reference Layne, Olsen, Baker, Legerski, Isakson, Pašalić, Duraković-Belko, Dapo, Ćampara, Arslanagić, Saltzman and Pynoos2010; Oldham-Cooper et al., Reference Oldham-Cooper, Hardman, Nicoll, Rogers and Brunstrom2011), forced displacement (Mels et al., Reference Mels, Derluyn, Broekaert and Rosseel2010), immigrant status (Wong et al., Reference Wong, Homma, Johnson and Saewyc2010) and natural disasters (Jia et al., Reference Jia, Tian, He, Liu, Jin and Ding2010; Li et al., Reference Li, Huang, Tan, Liu, Zhou and Yang2010). The most pertinent risk factors during infancy and early childhood are limited care and home stimulation (Grantham-McGregor et al., Reference Grantham-McGregor, Cheung, Cueto, Glewwe, Richter and Strupp2007), exposure to violence (Walker et al., Reference Walker, Wachs, Meeks Gardner, Lozoff, Wasserman, Pollitt and Carter2007) and poor maternal mental health (Anselmi et al., Reference Anselmi, Piccinini, Barros and Lopes2004). During the school-age period (from ages 5 to 18 years), factors of low physical health (Lo et al., Reference Lo, Ho, Mak, Wong, Lai and Lam2009), academic difficulties (Arun and Chavan, Reference Arun and Chavan2009), bullying (Chaux et al., Reference Chaux, Molano and Podlesky2009), family dysfunction (Lee et al., Reference Lee, Guo, Tsang, He, Huang, Zhang, Liu, Shen and Kessler2011), child labour (Ibrahim et al., Reference Ibrahim, Abdalla, Jafer, Abdelgadir and De Vries2019), physical, sexual and substance abuse (Benjet, Reference Benjet2010; Curto et al., Reference Curto, Paula, Do Nascimento, Murray and Bordin2011; Miller et al., Reference Miller, Borges, Orozco, Mukamal, Rimm, Benjet and Medina-Mora2011), pathological use of the Internet (Lam and Peng, Reference Lam and Peng2010) and teenage pregnancy (Miller et al., Reference Miller, Borges, Orozco, Mukamal, Rimm, Benjet and Medina-Mora2011) can also give rise to problematic mental health. These factors and their relationships to mental health risk are observed in numerous settings across the globe, and the aforementioned articles evidence their specific relevance to the development of mental health conditions in South Asia. An overview of the range of contributory factors is conceptualised in Figure 1.
Figure 1. Contributory factors in the development of mental health problems amongst children and adolescents in South Asia.
Whilst many mental health risks are highly prevalent in South Asia, particular psychosocial and environmental conditions can mitigate against the development-related disorders. Evidence suggests that in LAMIC South Asian settings, factors that contribute to this kind of resilience are effective behavioural and emotional self-regulation (Goldstein and Brooks, Reference Goldstein and Brooks2013), emotionally responsive and competent parenting, educational resources, strong carer attachment and a comprehensive peer network (Wyman et al., Reference Wyman, Cowen, Work, Hoyt-Meyers, Magnus and Fagen1999; Kieling et al., Reference Kieling, Baker-Henningham, Belfer, Conti, Ertem, Omigbodun, Rohde, Srinath, Ulkuer and Rahman2011).
The development of mental health services to address and prevent identified mental health disorders in South Asia aligns with the global health agenda (Department of Health and Social Care, 2019). However, the progress of this goal is complicated by a number of cultural and contextual factors. For example, a comparatively low research output in South Asian countries hinders the development of policy and practice (Tomlinson et al., Reference Tomlinson, Bornstein, Marlow and Swartz2014), which in turn complicates the identification of effective resource deployment. Despite a predominantly rural population, the majority of mental health services are located in large cities, which exacerbates issues related to a general lack of specialist personnel and facilities (Palit and Bandyopadhyay, Reference Palit and Bandyopadhyay2016). This is particularly pertinent given specific observations that diagnostic and therapeutic services in primary care are lacking in India and Pakistan (Agarwal, Reference Agarwal2021; Hamdani et al., Reference Hamdani, Huma and Tamizuddin-Nizami2021), and that in Nepal, primary care practitioners are prohibited from legally diagnosing mental health conditions (Angdembe et al., Reference Angdembe, Kohrt, Jordans, Rimal and Luitel2017). Collectively, this means individuals are unable to obtain appropriate treatment from more localised forms of healthcare.
Further complication arises from the use of healthcare systems predominantly based on out-of-pocket payments in Bangladesh, India and Nepal, which exclude a majority of residents from obtaining formal treatment (Maselko et al., Reference Maselko, Sikander, Bangash, Bhalotra, Franz, Ganga, Rajan, O’Donnell and Rahman2016; Angdembe et al., Reference Angdembe, Kohrt, Jordans, Rimal and Luitel2017). Rates of urban poverty and unemployment are significant and increasing across LAMIC South Asian countries, therefore not only giving rise to mental health problems, but also restricting the capacity of those affected to receive treatment (Patel et al., Reference Patel, Flisher, Nikapota and Malhotra2008). In Pakistan, some support is offered by specialist taxes known as ‘zakat’, which is used to provide national social assistance to those living in poverty. However, the collection and distribution of zakat is disorganised, rendering it inaccessible to most of the population (Karim et al., Reference Karim, Saeed, Rana, Mubbashar and Jenkins2004), and residents are expected to pay at least 20% towards the cost of expensive services and medicine. Rates of mental health disorder tend to be the highest in the most deprived groups, as a result of food scarcity leading to malnutrition, and co-existing factors of family dysfunction and violence, criminality and neighbourhood danger (Patel et al., Reference Patel, Flisher, Nikapota and Malhotra2008). As such, those who are most in need of mental health treatment are also those least able to access it.
Lastly, the tendency to stigmatise and discriminate against people with mental illnesses is widespread across Asia (Zhang et al., Reference Zhang, Sun, Jatchavala, Koh, Chia, Bose, Li, Tan, Wang, Chu, Wang, Tran and Ho2019). There is little awareness and education on the complexities of mental health problems, which are known moderators of stigma (Corrigan et al., Reference Corrigan, Druss and Perlick2014). People with mental health problems are often perceived as dangerous or violent, and some evidence suggests that even the attitudes of professionals working to improve mental health are discriminatory (Lauber and Rössler, Reference Lauber and Rössler2007). Stigma can also present a barrier to the scaling-up of successful mental health services (Angdembe et al., Reference Angdembe, Kohrt, Jordans, Rimal and Luitel2017), and directly affects not only people living with mental illnesses, but also their wider support system and willingness to seek treatment (Corrigan et al., Reference Corrigan, Druss and Perlick2014). Collectively, these factors impede the delivery of care, which is already complicated by issues of limited resource, low accessibility and economic cost. Relatedly, Roberts et al. (Reference Roberts, Shrivastava, Koschorke, Patel, Shidhaye and Rathod2020) report that in rural areas of India, there is low perceived need for treatment and low awareness regarding psychological disorders. For example, depressive symptoms were described as ‘tension’, which are a natural response to living in poverty, or having a physical illness, and distinct from mental illness. This leads to the belief that such will only be alleviated if a person’s socioeconomic situation improves or symptoms of their physical illness are treated. As a result, there was a low take-up for treatment of depressive symptomatology, even when services were expanded.
In answer to the difficulties of facilitating effective mental health treatment in South Asia, the World Health Organization (WHO) has endorsed the value of community-based programmes (WHO, 2011). Such programmes include all those that take place locally, for example, in schools, primary care and community centres. Some community-based programmes may also help facilitate nonspecialist personnel to deliver mental health provision in their own environment, by offering training, supervision and support. This provides an immediate solution to the lack of available mental health specialists, and can drastically promote the availability of essential treatment to distanced, impoverished and marginalised populations (Angdembe et al., Reference Angdembe, Kohrt, Jordans, Rimal and Luitel2017). This practice is one example of ‘task-shifting’, and can increase the reach of programmes to a broad range of locations, whilst also making mental health support more financially accessible for both individuals and whole societies (WHO, 2007). The local nature of community-based programmes, as well as harnessing of pre-existing resources, can help target individuals before they begin to exhibit stark mental disorders, which require more extensive and expensive treatment to reduce the overall cost of delivering mental health services (Zraly et al., Reference Zraly, Rubin-Smith and Betancourt2011). This style of care can thus precede the necessitation of psychotropic drugs, which bypasses the complication of specialist diagnosis and prescription (Angdembe et al., Reference Angdembe, Kohrt, Jordans, Rimal and Luitel2017).
Community-based services have been shown to reduce the impact of stigma. For example, work in Korea has demonstrated the role of community-based services in promoting mental health literacy amongst a broader proportion of the population, and in turn increasing the degree of respect devoted towards people with mental illnesses (Zhang et al., Reference Zhang, Sun, Jatchavala, Koh, Chia, Bose, Li, Tan, Wang, Chu, Wang, Tran and Ho2019). Additionally, community-based services use medical diagnostic terms to a lesser extent than formal healthcare services, meaning they are less likely to evoke prejudiced perceptions of service users (Corrigan et al., Reference Corrigan, Druss and Perlick2014). Community-based services are more easily accessible, meaning those with mental health problems may be able to receive treatment at an earlier stage when their difficulties are less pronounced (Lauber and Rössler, Reference Lauber and Rössler2007).
Whilst community-based interventions present a practical and effective strategy to deliver evidence-based mental health treatment in low resource settings, little is known about their nature and implementation across South Asia for children and adolescents. Developing further knowledge on this topic can enable collaboration and integration by health professionals and policy makers to prioritise relevant research activities and services for LAMIC regions provide information on the fidelity and effectiveness of care in community-based settings and enable the potential scale-up of successful programmes.
Given the current lack of empirical evidence on the provision of community-based mental health programmes for young people in South Asian countries, and the complexity of this topic, we have chosen to present a scoping review with clear implications for research and practice, according to Daudt et al. (Reference Daudt, Van Mossel and Scott2013). This will provide a foundational summary of existing research, with a view to catalysing further investigation that considers more intricate themes across and within geographical and cultural contexts. As such, our primary objective was to identify the extent and type of evidence regarding mental health programmes for children and adolescents in South Asia, as well as identify gaps in knowledge. Secondary aims were to acknowledge examples of successful programmes with potential for delivery at scale, recognise principles to incorporate amongst new models of treatment and develop recommendations for integration across community-based South Asian healthcare.
Method
Positionality statement
Although this review is based in South Asia, it was conducted solely in the United Kingdom. Therefore, it would be pertinent to understand our personal and professional positionalities which have shaped this review. The first, second and last authors of this scoping review are White British academics from the United Kingdom. The third author is an ethnic South Asian academic from Southeast Asia with lived experiences in Southeast Asia and strong ties to South Asia.
All authors were a part of the Mental Health Initiative for South Asia (MhiSA), a 3-year project formed in 2018 with the objective of promoting science and research partnerships between the countries of South Asia and the United Kingdom. Throughout 3 years, MhiSA received funding from the British Council and support from other institutions such as the Ferdowsi University of Mashhad to conduct workshops and events that brought delegates from South Asia and the United Kingdom together and provided a platform to enable discussions and facilitate collaborations. One such workshop was the ‘United Kingdom–South Asia collaboration on Mental Health Workshop’ held in Nepal in April 2018. This workshop brought together policy makers, researchers and clinicians in the South Asia region and researchers in the United Kingdom to develop an agenda and strategy for mental health research and practice. Throughout activities and discussions during the events, one key theme that was identified was the need for more research in child mental health. We recognize that the aim of this project is to improve understanding of community-based mental health treatment in South Asia, and we have ensured that the study is unbiased, sensitive and appropriate to the South Asian context.
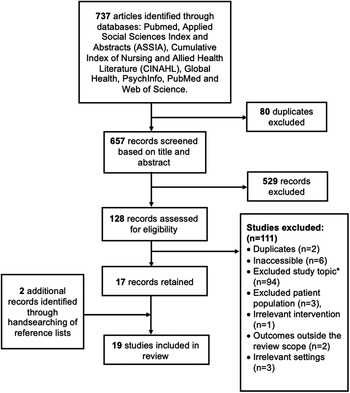
Data selection
Between August 2019 and March 2020, the following databases were used to conduct an electronic search of relevant articles: Applied Social Sciences Index and Abstracts, Cumulative Index of Nursing and Allied Health Literature, Global Health, PsychInfo, PubMed and Web of Science. Articles were returned if they contained appropriate descriptors of mental health (e.g., ‘depress*’ and ‘resilien$’), treatment (e.g., ‘interven$’ and ‘therap$’), setting (e.g., ‘community?base*’ and ‘non?government& organi?ation’), population (e.g., ‘adolescen$’ and ‘school?age’) and location (e.g., ‘Pakistan$’ and ‘Sri Lanka*’). An example of the search strategy applied to the databases is provided in the supplementary materials. Hand searching of reference lists pertaining to included articles was also conducted. Given the funding source, we addressed research specifically conducted in Bangladesh, India, Afghanistan, Pakistan, Iran, Sri Lanka and Nepal, according to the British Council’s definition of South Asia. Articles were restricted to those published between 1 January 2000 and the date of search.
Inclusion and exclusion criteria
The title and abstract of each article were used to determine initial relevance. Of interest were articles which could inform future research on community-based psychosocial treatment of child and adolescent mental health problems across South Asia. Accordingly, all research designs were retained. However, research related to diagnostic protocol or prevalence estimates, and research regarding purely pharmacological interventions, were excluded. Studies conducted in non-community-based settings were also excluded, as were articles which only addressed adults over the age of 18 and those which concerned any population residing outside of South Asia, as defined in this review. If the study regarded a mixed-age sample, inclusion for review necessitated a sample mean age within 0 to <18 years. All studies were required to include mental health as a primary consideration. Articles describing treatments which were only indirectly related to mental health (e.g., substance abuse) were excluded. However, no limitations were placed on dose, duration or mode of delivery of mental health treatment. Book chapters and editorial articles were also excluded.
Data analysis
Data for each included article were extracted using an adapted version of the template for intervention description and replication (TIDieR) checklist (Hoffman et al., Reference Hoffman, Glasziou, Boutron, Milne, Perera, Moher, Altman, Barbour, Macdonald, Johnston, Lamb, Dixon-Woods, McCulloch, Wyatt, Chan and Michie2014), leading to the identification of the following: number and age of participants, location of research, aim, type, duration and setting of intervention, sampling strategy, study design, comparators, outcome measurement, data analysis, results, conclusions, implications and economic considerations. Where possible, articles were coded for risk of bias according to the Cochrane Risk of Bias Tool for randomized controlled trials (RCTs) and non-RCTs, and any additional limitations of each study were identified. Moreover, factors that supported or inhibited the success of intervention design, delivery and implementation were noted.
Intercoder agreement
A second coder screened randomly selected articles (n = 295; 40%) to provide coder agreement data on inclusion and exclusion for review. Agreement was calculated by dividing the number of agreements (i.e., both coders elected to include or both elected to exclude the same article) by the total number of articles reviewed by both researchers (n = 295). Coders agreed upon 97% of articles, and for those upon which researchers did not agree, a discussion and mutual decision on inclusion took place. One coder then extracted data on all 26 variables the 19 articles, and one further coder conducted data extraction on all 26 variables for 10 of the 19 articles (53%). In this instance, agreement was defined as the extraction of exactly the same information from an article, and calculated via dividing the total number of agreements across variables and articles by the total number of variables (n = 260; 26 variables for each of the 10 articles). Agreement for these data was 96% (range 88–100% across variables).
Results
The final literature search resulted in 19 studies which were included (Figure 2). An overview of the 19 studies with respect to their design, location, setting, aims and intervention is provided in Table 1.
Figure 2. Flowchart depicting the selection of studies to be included in the review. *‘Topic’ refers to research related purely to diagnostic protocol or prevalence estimates rather than treatment.
Table 1. Overview of design, participants, setting, aims and intervention data across all identified studies (n = 19)
Abbreviations: ASD: autism spectrum disorder; CBA: Controlled before-and-after
Delivery methods and personnel
Twelve articles involved mental health professionals, eight recruited parents or teachers and eight included community volunteers. Three studies reported on the production of workbook materials, one recorded the use of training via video conferencing and four interventions involved game-related components.
Aims
The most commonly occurring intervention aims were to treat PTSD (n = 6) and autism (n = 5). Additional studies attempted to address behavioural problems (n = 3), anxiety (n = 3), cognitive development (n = 2) and general emotional problems (n = 2). Other articles concentrated on stress (n = 2), depression (n = 2), ADHD (n = 1) and suicide prevention (n = 1). Other research adopted a strengths-building approach, focusing on the promotion of general well-being (n = 2), resilience (n = 1) and self-esteem (n = 1). Five articles employed an educational approach as a means of improving mental health awareness. Equally, 12 articles used educational methods to train a broad range of skills relevant for the management of mental health conditions that across articles, from self-regulation to communication, and was directed at both those at-risk or experiencing a mental health problem, as well as parents, caregivers and healthcare professionals responsible for providing support. Task-shifting methods were also employed in 16 articles, involving the training of teachers, parents, volunteers, lay health workers and counsellors, local specialists, parents and care-givers and children themselves. Three of these articles employed task-shifting via the specific adoption of a train-the-trainer approach. Finally, eight articles considered the development of context specific resources, including technologies, workbooks and games suitable for specific cultural and demographic requirements.
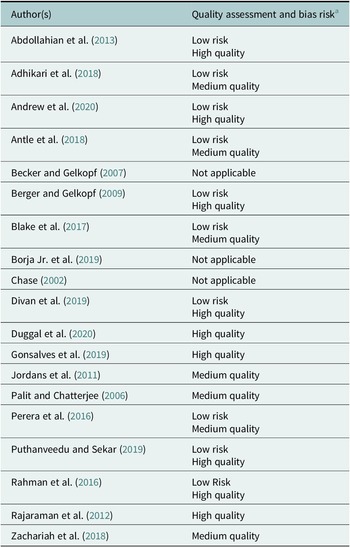
Risk of bias and critical appraisal of sources of evidence
Of the studies able to be assessed using the Cochrane Risk of Bias Tool for RCTs and non-RCTs (n = 6), bias for sampling randomisation, allocation concealment, participant and outcome blinding and data completeness and reporting was generally low (see Table 2). In one study (Antle et al., Reference Antle, Chesick, Sridharan and Cramer2018), a lack of allocation concealment and blinding of participants presented a high risk of bias, and four of the six studies lacked sufficient information to identify risk of bias on one or more of the assessment domains. The most frequent limitations of quality were a small or poorly representative sample size, lack of suitable comparators, low use of pre-validated questionnaires and little assessment of longitudinal outcomes. Additionally, most intervention programmes were designed and evaluated by the same researchers, with little use of empirical frameworks to increase the validity of findings. Alternatively, several studies presented robustly designed and well-validated research (Berger and Gelkopf, Reference Berger and Gelkopf2009; Rahman et al., Reference Rahman, Divan, Hamdani, Vajaratkar, Taylor, Leadbitter, Aldred, Minhas, Cardozo, Emsley, Patel and Green2016; Divan et al., Reference Divan, Vajaratkar, Cardozo, Huzurbazar, Verma, Howarth, Emsley, Taylor, Patel and Green2019; Andrew et al., Reference Andrew, Attanasio, Augsburg, Day, Grantham-McGregor, Meghir, Mehrin, Pahwa and Rubio-Codina2020), including one qualitative analysis which used multiple perspectives to substantiate information and triangulation (Zachariah et al., Reference Zachariah, de Wit, Bahirat, Bunders-Aelen and Regeer2018). As such, the results of some studies, particularly those which involved superficial outcome assessments or poorly generalisable samples (Chase, Reference Chase and Bush2002; Jordans et al., Reference Jordans, Komproe, Tol, Susanty, Vallipuram, Ntamatumba, Lasuba and De Jong2011; Adhikari et al., Reference Adhikari, Upadhaya, Satinsky, Burkey, Kohrt and Jordans2018; Antle et al., Reference Antle, Chesick, Sridharan and Cramer2018), should be interpreted with caution.
Table 2. Overview of bias risk using the Cochrane Risk of Bias Tool where applicable
a For all applicable studies, a critical appraisal based on study strengths and limitations is given using the Cochrane Risk of Bias for RCTs and non-RCTs is also used.
Availability
The number of interventions conducted in different geographical regions assimilates the patterning of prevalence data, with most research activity in India, and substantially less work conducted in Afghanistan, Iran and Pakistan. Whilst access to formal mental health support is most limited in rural areas (Palit and Bandyopadhyay, Reference Palit and Bandyopadhyay2016), the majority of studies in the current review were located in urban districts, indicating current community-based provision does not wholly address the lack of formal mental health infrastructure. Consequently, broad policy approaches may consider how pre-existing programmes can be applied across rural locations in South Asia.
Most studies were delivered in schools, with outpatient clinics, home-based programmes and community centres utilised to a lesser extent. School settings were noted as valuable for accessing large numbers of children at regular intervals to both test and implement intervention programmes (Berger and Gelkopf, Reference Berger and Gelkopf2009). However, it is also necessary to acknowledge that some children in LAMIC South Asian settings are unable to attend school, often for reasons which also increase their mental health risk, such as poverty or an unstable home environment (Jordans et al., Reference Jordans, Komproe, Tol, Susanty, Vallipuram, Ntamatumba, Lasuba and De Jong2011). As such, it is important to consider the most appropriate avenues to address the needs of hard-to-reach groups.
A home-based programme for autism demonstrated equivalent efficacy to that conducted in specialist therapeutic settings, suggesting that the lack of formal care centres in rural settings can at least be partially addressed by upskilling local workers to deliver support (Perera et al., Reference Perera, Jeewandara, Seneviratne and Guruge2016). Using community centres was also noted to catalyse cohesion by bringing together different religious and subcultural factions (Chase, Reference Chase and Bush2002). Grassroots community projects also hold particular value, because they are more sustainable, responsive and organic than top-down interventions which have a less flexible structure, and do not necessarily respond to the specific needs of the populations they are designed to support (Chase, Reference Chase and Bush2002). This suggests that community-based interventions may be more effective in responding to situational factors (such as increasing access to mental healthcare whilst reducing stigma) than larger-scale programmes.
Treatment focus
Existing data suggest that the most common mental health disorders in South Asia are depression, stress, PTSD and anxiety (Hossain et al., Reference Hossain, Purohit, Sultana, Ma, McKyer and Ahmed2020). In the present review, there were a high proportion of studies which investigated care for PTSD, an addition to a large body of work on autism. However, much less work attended to the treatment of depressive disorders. Ogbo et al. (Reference Ogbo, Mathsyaraja and Koti2018) argue that the prevalence of depression in South Asia positions its prevention and treatment as a key priority, and as such, a greater degree of depression-related intervention may be a valuable direction for future research. Evidence also indicates that marginalised populations are most likely to present with mental health problems (Hossain et al., Reference Hossain, Purohit, Sultana, Ma, McKyer and Ahmed2020). Five of the 19 reviewed studies concerned populations who typically suffer prejudice, including children of Devadasis and socioeconomically deprived communities. The Devadasi system is a practice followed by a small community in South India, which involves dedicating girls from low social castes to a deity and auctioning their virginity. Devadasi women are prohibited from marrying and their illegitimate children are shunned by society. On one hand, work that addresses the needs of those most likely to experience mental health problems is undoubtedly valuable. However, there are also data to suggest that distinguishing groups who are already stigmatised can exacerbate the effects of prejudice, and further isolate individuals from the rest of society (Puthanveedu and Sekar, Reference Puthanveedu and Sekar2019). Additional work suggests that community-based mental healthcare can have further unintended negative consequences, given by nature it does not involve specialist personnel and therefore must be carefully delivered. For example, in the present review, Berger and Gelkopf (Reference Berger and Gelkopf2009) note that directly addressing trauma in children who had experienced exposure to terror and war resulted in increased sensitisation and the need for specialist attention. Equally, whilst Zachariah et al. (Reference Zachariah, de Wit, Bahirat, Bunders-Aelen and Regeer2018)) found that a suicide-prevention programme delivered by school children to their peers provided benefits for both providers and recipients, they also discovered peer educators could attempt to provide advice too quickly, causing recipients to feel misunderstood, and become withdrawn. Finally, after developing and evaluating a smartphone game to support adolescents at risk of depression in India, Gonsalves et al. (Reference Gonsalves, Hodgson, Kumar, Aurora, Chandak, Sharma, Michelson and Patel2019) noted that whilst the game was well received and effective, it could not completely replace direct counsellor supervision. These findings indicate the value of carefully targeting specific disorders and populations, in order to avoid exacerbating pre-existing problems.
In reducing the risk of negative intervention consequences, it may valuable to further investigate the approaches of strength building and proportionate universalism. In contrast to deficit-driven models, strength-based approaches aim to build resilience by developing human capacities which can protect against adversity (Gable and Haidt, Reference Gable and Haidt2005; Wong, Reference Wong2013). Given that strength-based approaches shift focus away from formal diagnoses or treating disease symptomatology, they are less likely to risk stigmatising individuals who become labelled as ‘ill’. Instead, strength-based approaches concentrate on the promotion of positive functioning across societies and individuals (Ryff and Singer, Reference Ryff and Singer2006). One study explored the use of creative healing, such as art- and drama-based therapy, as an alternative to medicalisation or counselling (Chase, Reference Chase and Bush2002). At present, the evidence base for such work is limited, both in South Asian and Western settings (Baker et al., Reference Baker, Metcalf, Varker and O’Donnell2018). However, given that non-medicalised methods hold potential for promoting well-being without evoking stigma, future research may consider investigating the efficacy of creative healing and other strength-based approaches in South Asia. Indeed, the growing emphasis on preventative healthcare methods in Western settings represents a learning opportunity at the global scale, suggesting South Asian countries may benefit from embedding preventative care at an early stage, as they develop their mental health resources.
The principle of proportionate universalism argues that interventions to reduce inequality are most effective when universally implemented, however with a scale and intensity that is proportionate to the level of disadvantage (Marmot and Bell, Reference Marmot and Bell2012). This model involves delivering projects that offer holistic treatment at scale, with targeted intervention for those in need of more specialised therapy. It increases the accessibility and cost efficiency of mental health support, whilst also acknowledging some groups require more extensive treatment, and has been applied to great effect regarding health inequalities in Western settings (Carey et al., Reference Carey, Crammond and De Leeuw2015). A study conducted in Nepal (Adhikari et al., Reference Adhikari, Upadhaya, Satinsky, Burkey, Kohrt and Jordans2018) noted that a family- and school-based intervention to improve child behaviour problems could lead to successful results by providing children of lower social castes and additional services as a means of subtly addressing ingrained discrimination. Moreover, a study found that a multilayered programme which implemented low-intensity interventions at scale, as well as a triage system for those with more severe needs, efficiently matched the requirements of individual children to different levels of care (Jordans et al., Reference Jordans, Komproe, Tol, Susanty, Vallipuram, Ntamatumba, Lasuba and De Jong2011). This is pertinent given that resources to provide mental health support are particularly limited in South Asian settings, and therefore must be distributed wisely. As such, future research should continue to explore the integration of proportionate universalism amongst developing mental healthcare in South Asia.
Feasibility
Task-shifting
Studies in the present review included a broad range of implementation methods, and the concept of task-shifting has been noted as particularly relevant for LAMIC settings, increasing both the practical and financial accessibility of projects by maximising available human resources. Task-shifting was utilised in 11 of the 19 identified articles, and a number of implications can be inferred across studies. For example, several authors perceived task-shifting as useful, including Rahman et al. (Reference Rahman, Divan, Hamdani, Vajaratkar, Taylor, Leadbitter, Aldred, Minhas, Cardozo, Emsley, Patel and Green2016) and Rajaraman et al. (Reference Rajaraman, Travasso, Chatterjee, Bhat, Andrew, Parab and Patel2012), who noted the value of this approach in scaling-up school health promotion in LAMIC settings. Moreover, Andrew et al. (Reference Andrew, Attanasio, Augsburg, Day, Grantham-McGregor, Meghir, Mehrin, Pahwa and Rubio-Codina2020) specifically described task-shifting as a factor in the success of a home-based intervention for child development in Indian urban slums, whereas Becker (Reference Becker2007) concluded that task-shifting is of distinct value in disaster settings because it allows large numbers of individuals to be trained and mobilised for prompt mental healthcare delivery. Finally, Palit and Chatterjee (Reference Palit and Chatterjee2006) and Zachariah et al. (Reference Zachariah, de Wit, Bahirat, Bunders-Aelen and Regeer2018) also reported the benefits of task-shifting to extend to those who are trained to deliver care by providing a sense of purpose and employment.
However, certain conditions are also required for task-shifting approaches to work effectively. Primarily, the appropriate supervision of support staff for retaining implementation fidelity and protecting the mental health of delivery staff themselves are required. Jordans et al. (Reference Jordans, Komproe, Tol, Susanty, Vallipuram, Ntamatumba, Lasuba and De Jong2011) reported significant distress among volunteer facilitators who implemented classroom-based interventions for mental well-being compared to counsellors who received extensive training and renumeration for their time. Addressing logistical difficulties and providing mental health support could help to reduce stress across service providers, as well as adapting workloads Jordans et al., Reference Jordans, Komproe, Tol, Susanty, Vallipuram, Ntamatumba, Lasuba and De Jong2011). This finding is complemented by the observations of Andrew et al. (Reference Andrew, Attanasio, Augsburg, Day, Grantham-McGregor, Meghir, Mehrin, Pahwa and Rubio-Codina2020), who recommended physical health workers who are provided additional psychosocial training must be supported so that mental health intervention does not detract from their existing work. Rahman et al. (Reference Rahman, Harrington and Bunn2002) and Rajaraman et al. (Reference Rajaraman, Travasso, Chatterjee, Bhat, Andrew, Parab and Patel2012) concluded that comprehensive professional supervision was essential in training and supporting nonspecialist personnel in delivering mental healthcare, whilst Rajaraman et al. (Reference Rajaraman, Travasso, Chatterjee, Bhat, Andrew, Parab and Patel2012) indicated that implementing clearly defined referral procedures helped lay school counsellors to feel confident in delivering appropriate care, and to signpost serious cases when necessary. The importance of a hands-on yet flexible supervisory approach was also effective in upskilling professionals supporting children with developmental difficulties (Duggal et al., Reference Duggal, Dua, Chokhani and Sengupta2020). One study noted that facilitators on a peer-education programme to reduce suicide should be reminded of the limits of their personal responsibility, and provided opportunities for group debriefing and social bonding in order to prevent burnout (Zachariah et al., Reference Zachariah, de Wit, Bahirat, Bunders-Aelen and Regeer2018). Lastly, in a study evaluating large-scale psychosocial support interventions for Rohingya refugees, the authors stated that projects that involve international experts must strive for stability in management, rather than short-term tenures, which can lead to changes in strategy and difficulty in the implementation of programmes (Borja Jr. et al., Reference Borja, Khondaker, Durant and Ochoa2019). This can subsequently result in unfavourable responses from other sectors, who devalue inconsistent programmes as disorganised.
Training
The importance of providing training for mental health provision in South Asian settings is emphasised to be important for community-based interventions. One study (Antle et al., Reference Antle, Chesick, Sridharan and Cramer2018) suggested that training parents to deliver interventions is unrealistic in some settings, due to deficits in literacy, time and educational background. Alternatively, a home-based early intervention programme for autism conducted in urban Sri Lanka (Perera et al., Reference Perera, Jeewandara, Seneviratne and Guruge2016) found that offering parents’ individual supervision, demonstrating activities and materials, conducting follow-up sessions and providing personalised information strongly contributed to the programme’s success, via increased motivation and capacity of parent interventionists. Becker (Reference Becker2006) noted that the adoption of a train-the-trainer model is valuable in resource poor settings, specifically in the training of large numbers of people. Under this model, initial training is delivered to a small number of individuals who then go on to impact organisations. Given the importance of best understanding how to recruit, train and supervise those who deliver task-shifting approaches (Borja Jr. et al., Reference Borja, Khondaker, Durant and Ochoa2019), future research may consider these factors in more detail, as a means of bridging the treatment gap between need and availability of care LAMICs.
Telepsychiatry
It is also valuable to consider the growing use of technological approaches, particularly given the transformative effect of COVID-19 on telemedicine (Portnoy et al., Reference Portnoy, Waller and Elliott2020). Telepsychiatry is an emerging resource in South Asian settings, particularly in India where the rapidly increasing penetration of mobile devices enables geographically unrestricted intervention. Smartphone games can be useful in promoting engagement, decreasing stigma and addressing some of the challenges of delivering accessible and timely mental health support in under-resourced society. However, Gonsalves et al. (Reference Gonsalves, Hodgson, Kumar, Aurora, Chandak, Sharma, Michelson and Patel2019) concluded that such tools should be extensively tested to ensure efficacy and acceptability, and paired with instructional and relationship support from physical counsellors. Two studies also explored how technology can be used to successfully address difficulties in training for mental healthcare. Antle et al. (Reference Antle, Chesick, Sridharan and Cramer2018) investigated the use of a computer-tablet game to improve self-regulatory skills, and found that participants quickly and successfully learnt how to use the platform, removing the need for parent training on the delivery of mental health support. The efficacy of the game was observed in real-world change, including decreases in hyperactive, aggressive and anxious behaviour, and increases in self-esteem, concentration, self-expression and discipline. Duggal et al. (Reference Duggal, Dua, Chokhani and Sengupta2020) explored the use of technology in training a broad range of child health practitioners to develop autism-specific treatment skills. They found that online supervision enabled continuity and interaction across participants, and facilitated the involvement of multidisciplinary individuals from a number of geographical areas. This is highly significant in LAMIC settings, where professional awareness of autism is low, training opportunities are limited and experts are localised to a few locations. However, it is also important to note that access to technology may still be limited in some areas or populations, and to integrate such contextual information in the design or adaptation of interventions.
Acceptability
Adaptation of materials
One of the most prevalent observations was the importance of adapting intervention materials to specific contextual requirements, which have been highlighted by several authors. There is a lack of pre-validated survey instruments that have been reliably translated for South Asian contexts; many tools contain questions inappropriate for children living in poverty (Antle et al., Reference Antle, Chesick, Sridharan and Cramer2018). Altering designs in smartphones to account for literacy difficulties across youths in India was found to significantly improve literacy, and by designing the game to operate offline allowed youths to engage with the game in regions with limited Internet access (Gonsalves et al., Reference Gonsalves, Hodgson, Kumar, Aurora, Chandak, Sharma, Michelson and Patel2019). Another example is demonstrated by a study conducted in Sri Lanka. As emotions are widely expressed via body processes, and acknowledging one’s strength is public is considered ostentatious, the authors adapted their programme to emphasise somatic experience and encourage children to take pride in their strengths whilst acknowledging weaknesses (Berger and Gelkopf, Reference Berger and Gelkopf2009). The importance of attending to the meaning and relevance of terms across languages to ensure comprehension was also recommended (Borja Jr.. et al., Reference Borja, Khondaker, Durant and Ochoa2019), and to use qualitative methods to understand the context in the development and implemented on materials (Blake et al., Reference Blake, Rubenstein, Tsai, Rahman, Rieth, Ali and Lee2017). This is particularly important during projects that involve the consecutive translation of materials across multiple languages, and in settings where concepts related to mental health are often new and not widely understood. Future research may consider how intervention materials can be best developed to account for cultural factors, as well as the development of questionnaires which are appropriate for research with target populations.
Relationships across stakeholders and researchers
Intervention acceptability was also influenced by the relationship between researchers and stakeholders. In a school-based programme which trained community volunteers as lay counsellors, teachers initially mistakenly referred children to the programme based on disciplinary rather than mental health problems, and complained about a lack of information sharing (Rajaraman et al., Reference Rajaraman, Travasso, Chatterjee, Bhat, Andrew, Parab and Patel2012). These issues were substantially reduced after monthly updates were produced and disseminated amongst the faculty, resulting in a more positive evaluation of the programme across both teachers and students. The reports were also effective in reducing the stigmatising attitude of some teachers, and identifying a specific period to deliver counselling in the school timetable further alleviated tension between counsellors and staff. When delivering mental health training to those already working in the field, Duggal et al. (Reference Duggal, Dua, Chokhani and Sengupta2020) stated that incorporating stakeholder feedback is particularly critical in South Asia, because professionals have often received some basic training, but lack specialised skills, which require deliberate practice and reflection.
Intervention terminology
Lastly, several authors noted that participants appreciated interventions which did not require medical professionals, or the use of diagnostic terms. In particular, the substitution of the word ‘ASD’ with ‘problem behaviours’ promoted engagement by parents of children with autism by emphasising an outcome parents were most motivated to address, and reduced the fear of possible stigma related to labelling a disability (Blake et al., Reference Blake, Rubenstein, Tsai, Rahman, Rieth, Ali and Lee2017). Likewise, another study investigated a programme to provide cognitive-behavioural play therapy for children with ADHD, and parents welcomed a form of therapy which did not involve referral to a psychologist, psychiatrist or physician for medical treatment (Abdollahian et al., Reference Abdollahian, Mokhber, Balaghi and Moharrari2013). Finally, Puthanveedu and Sekar (Reference Puthanveedu and Sekar2019) reported that children of devadasis are stigmatised to the extent they are isolated to outlying districts where facilities are poorly available. As such, providing community-based mental health provision in these regions helps to avoid the entrenchment of further discrimination, and may support the eventual ‘mainstreaming’ of marginalised populations.
Discussion
The present search revealed only a small number of studies regarding community-based intervention for children and adolescents living in South Asia with most research activity in India. This is unsurprising, given known deficits in research and practice for mental health support amongst this population (Kieling et al., Reference Kieling, Baker-Henningham, Belfer, Conti, Ertem, Omigbodun, Rohde, Srinath, Ulkuer and Rahman2011). However, the results do indicate the emerging existence of community-based youth mental health provision in South Asia, including several studies which are the first of their kind to be undertaken in a LAMIC setting. For example, Rahman et al. (Reference Rahman, Harrington and Bunn2002) presented a novel contextual evaluation of an ASD intervention, and Jordans et al. (Reference Jordans, Komproe, Tol, Susanty, Vallipuram, Ntamatumba, Lasuba and Jong2010) investigated a pioneering multilayered psychosocial healthcare initiative. We found that the majority of the included studies were (1) conducted in India, (2) delivered in school-based and urban settings and (3) focused on the treatment of PTSD or ASD.
The empirical quality of identified studies was variable, with a high prevalence of small and poorly generalisable samples, and low use of adequate comparators or pre-validated assessment materials. These factors likely result from the complexity of conducting research in LAMIC South Asian settings; resources are generally constrained, and the availability of questionnaire materials to assess mental health outcomes which are comprehensible to populations of interest is low. Moreover, there can be logistical and administrative complications regarding the implementation of randomised controlled trials in South Asian settings, as well as the ethical dilemma of withholding treatment to control groups (Becker, Reference Becker2006). Therefore, future research could also address the development of contextually appropriate questionnaires, and enhance pre-existing research by utilising larger and more diverse samples.
It is also important to acknowledge cultural and linguistic factors to support accepted and effective intervention. Whilst Fricchione et al. (Reference Fricchione, Borba, Alem, Shibre, Carney and Henderson2012) call for an increase in research at the local context level to adapt and evaluate interventions to ensure that it is appropriate for the context, it is important to understand the scale of language barriers. South Asia is one of the most diverse regions in the world, and each of the countries in South Asia is rife with cultural and linguistic diversity. India, for example, has 22 major languages (Department of Higher Education, 2021). Interventions and translation of materials must be innovative to cope with the complexities of the diversity of language and culture (Patel and Prince, Reference Patel and Prince2010).
Another issue with linguistic barriers arises from the communication difficulties between Western professionals and health workers, where interpreters may be used. Swartz et al. (Reference Swartz, Kilian, Twesigye, Attah and Chiliza2014) argue that using interpreters to translate across cultures may not be sufficient to bridge this gap due to the vast differences in languages and cultural nuances, and translating instruments into a few local languages are insufficient to meet the diversity and complexity of language. It is also important to recognise the vast differences in urban–rural and socioeconomic settings across the regions, where materials may need to be adapted. Literacy levels within countries also differ considerably adding on to the complexity of translation of intervention materials which needs to be adapted to be suitable to the target users.
There should be ongoing dialogue and discussions between Western professionals/clinicians, researchers and lay workers on the ground who are familiar with the cultural and linguistic context of the families and target users during the adaptation of intervention materials. For example, Blake et al. (Reference Blake, Rubenstein, Tsai, Rahman, Rieth, Ali and Lee2017) report training received by the native clinicians in ASD by Western professionals, and ongoing discussions between investigators from Bangladesh and the United States, and native clinicians in Bangladesh to ensure that the materials used for an ASD intervention were suitable for the cultural, linguistic and socioeconomic context. Language was simplified, and where possible images were used rather than words to accommodate parents with low literacy levels. Images were also appropriate within the specific rural and socioeconomic context. Importantly, there was ongoing dialogue between the native clinician delivering the intervention, study investigators and scientists involved to ensure that the material was culturally, linguistically and contextually appropriate while ensuring that the concepts are not lost in translation. Swartz et al. (Reference Swartz, Kilian, Twesigye, Attah and Chiliza2014) also call for an increase in reports and sharing knowledge by workers who have worked on the ground and developed and delivered mental health programmes, overcoming language barriers.
Common to many LAMIC regions, it is also important to consider the power imbalance between Western professionals and interpreters and lay workers during training, where they may feel compelled to behave in a way that they think is most acceptable to professionals, thus compromising the efficacy of delivery (Swartz et al., Reference Swartz, Kilian, Twesigye, Attah and Chiliza2014). Power imbalances are also observed between professionals or health workers and participants in a study where participants may not fully answer questions due to what they perceived was a lack of education on their side compared to the professional, and therefore needed more probing to provide their perspectives (Roberts et al., Reference Roberts, Shrivastava, Koschorke, Patel, Shidhaye and Rathod2020). It is important to be aware of these cultural differences when communicating and interacting with participants who may feel compelled to behave in a way that they perceive is appropriate to the professional.
In summary, the paucity of resources and trained professionals in South Asian settings leads to a significant gap between mental health treatment and needs. Capacity to address this via professional training is limited, given the resource-constrained context of South Asia, and so utilising methods which are innovative, flexible and make best possible use of existing capacity is critical. Community-based mental health provision appears to provide a potential answer to this need, particularly when task-shifting and stigma reduction methods are implemented. However, there needs to be ongoing support in relation to supervision of staff to maintain effectiveness of intervention in the long term. This support should incorporate training, mentoring and capacity development in order to ensure a more sustainable model for intervention implementation.
The results of this review indicate the availability of mental health support, and can also be used to understand the feasibility, acceptability, impact and quality of existing interventions. Additionally, these findings provide new insight on approaches which are thought valuable for South Asian settings, primarily task-shifting and stigma reduction, with implications for policy, practice and research. This review also provides a number of directions for future research to build upon existing intervention, in order to bolster the mental health and future prosperity of South Asian societies.
Limitations
It is important to note several limitations of the current work. First, we must acknowledge that mental health is a complex concept, requiring interdisciplinary intervention. Our approach is focused upon the infrastructure and enactment of mental health treatment, rather than ‘care’ in its most comprehensive term, and therefore should be viewed as complementary to additional investigations which utilise different disciplinary perspectives, for example, those that consider community-based interventions integrated amongst care programmes.
Additionally, our study is limited only to the articles in the review which was determined by the inclusion and exclusion criteria. For example, we exclusively considered studies where the mean age of samples is between 0 and 18. Studies that may have included slightly older young adults may provide information on interventions that are applicable to those under 18; however, this work was not included in the current review.
The review was also dominated by studies in India, and given the cultural and geographical diversity of South Asia, our findings are limited in their extrapolation to every region considered. However, this is reflective of relatively developed mental health infrastructure and research capacity in India compared to other countries, and therefore provides important detail on the current state of research output in other regions. Relatedly, we sought to obtain insights from grey literature including reports and dissertations that may include important insights on community-based care in this region. Despite contact with local agents, any material proved highly difficult to access, and therefore could not be included in the present review.
Recommendations for practice and research
The present review indicates that community-based mental health provision for children and adolescents in South Asia is meagre, yet emerging. Identified studies suggest that community-based interventions can be effective, acceptable and impactful for young South Asian populations, and may hold particular value in reducing the impact of stigma and its consequences, whilst addressing the paucity of care available outside of urban districts with formal centres of care. The findings presented here suggest that task-shifting approaches should incorporate comprehensive and flexible supervision, clearly defined referral procedures and a consistent managerial team. Results also indicate that community-based programmes may be most effective when complemented with targeted specialist intervention, as recommended in proportionate universalism. Furthermore, the contextual adaptation of intervention materials is critical, and must take into account linguistic, cultural and logistical factors. One approach taken in ‘implementation science’ methodology is to co-design and co-produce interventions with the end user, and this seems particularly appropriate here given the diversity in intervention context (Eccles et al., Reference Eccles, Armstrong, Baker, Cleary, Davies, Davies, Glasziou, Ilott, Kinmonth, Leng, Logan, Marteau, Michie, Rogers, Rycroft-Malone and Sibbald2009).
Priority areas for further investigation are to develop research capacity and practice in rural locations and in countries with a relatively reduced output, as well as to increase the number of studies which investigate the treatment of depressive disorders. Work on the efficacy of community-based intervention in reducing stigma could also be complemented by considering strength-based approaches. Whilst task-shifting methods appear to present strong value for mental health intervention in low resource settings, it is important to acknowledge that ongoing support is critical, and greater knowledge regarding the supervision, training and recruitment of staff across different contexts and populations could further support their implementation. Additionally, consideration should be given to the sustainability of support after initial research projects or external funding has ended. Lastly, technology could be utilised to a greater extent to address the treatment gap between demand and provision of mental health support, and as such further research should build upon the investigations included here.
Open peer review
To view the open peer review materials for this article, please visit https://doi.org/10.1017/gmh.2022.49.
Data availability statement
Data availability is not applicable to this article as no new data were created or analysed in this study.
Acknowledgements
We would like to thank the Mental Health Initiative in South Asia (MhiSA) partners, the facilitators and delegates from the ‘South Asia Collaboration on Mental Health’ event held in Kathmandu, Nepal, on 10–12 April 2018 in which the discussions held during the event led to this scoping review: Dr Fatemeh Ahmadi (British Council, UK), Dr Javad Fadardi (Ferdowsi University of Mashhad, Iran), Dr Rebecca Crane (Bangor University, UK), Dr Farzana Islam (Child Development Centre, Apollo Hospital, Bangladesh), Dr Sanjeev Jain (National Institute of Mental Health and Neurosciences, India), Dr Sumeet Jain (The University of Edinburgh, UK), Mr Suraj Koirala (Transcultural Psychosocial Organization, Nepal), Dr Anand Krishnan (All India Institute of Medical Sciences, India), Mr Nagendra P. Luitel (Transcultural Psychosocial Organization, Nepal), Dr Kedar Marahatta (World Health Organization Country Office, Nepal), Dr Mohammad Nami (Shiraz University of Medical Sciences, Iran), Dr Jacqueline Rodgers (Newcastle University, UK), Dr Rajesh Sagar (All India Institute of Medical Sciences, India), Dr Sayyed Ali Samadi (Ulster University, UK), Dr Aditya Sharma (Newcastle University, UK), Dr Rahul Ramchandra Shidhaye (Public Health Foundation of India), Dr Michaela Swales (Bangor University, UK), Dr Zahra Tabibi (Ferdowsi University of Mashhad, Iran) and Dr Fahmida Tofail (International Centre for Diarrhoeal Disease Research, Bangladesh).
Author contributions
Conceptualisation: R.A.S. and J.A.P.; Writing – original draft: R.A.W.; Writing – review and editing: all authors.
Financial support
This scoping review was supported by the British Council.
Competing interests
The authors declare no competing interests exist.







Comments
Dr Azlina Amir Kassim
Lecturer
School of Human and Behavioural Sciences
Bangor University
July 22, 2022
Professor Gary Belkin (Editor-in-Chief) and
Dr Rahul Shidaye (Associate Editor)
Cambridge Prisms: Global Mental Health
Dear Prof Belkin and Dr Shidaye,
Thank you for the opportunity to submit a revised draft of the manuscript. We thank you and the reviewers for their time and feedback on our manuscript. We have worked hard to address the reviewers’ comments in what we believe is the final version of the paper. We hope the manuscript will now be acceptable for publication in Cambridge Prisms: Global Mental Health. In addition to the revised paper, we also include the graphical abstract, impact statement and social media summary with this submission.
Below, we detail how we have responded to the reviewer’s comments (in bold). All edits in the main manuscript in line with the reviewers’ comments are in red font. We also include the revised sentences and edits in this letter.
• Reviewers comment 1: Page 4: "in India, Bangladesh, Pakistan or Afghanistan (Belfer, 2008), and very few in Nepal (WHO, 2017)." These new precisions are appreciated but one of the citations is 14 years old and the other is 5 years old. Especially for the Belfer citation (the older), one wonders if the information remains accurate?
<b>We have revised the sentence and updated the citations to reflect the more current situation, as below:</b>
Revision (page 3): “In Bangladesh, Sri Lanka, Nepal and Pakistan there are no child-specific mental health policies (WHO, 2017, Hossain et al., 2021). Additionally, very few psychiatrists offering specialised treatment for children or adolescents in India, Bangladesh, Pakistan, Nepal or Afghanistan (Agarwal, 2021; Hamdani, Huma, & Tamizuddin-Nizami, 2021; Singh, Gupta, Singh, Basnet, & Arafat, 2022; Skuse, 2021; Wang et al., 2022).”
• Reviewers comment 2: Page 4: a poor psychosocial environment is listed as a risk factor - it would be good to understand what is meant by this. The list in general has a lot of overlapping concepts.
<b>We agree that the list contains overlapping concepts, and we have replaced the term “poor psychosocial environment” to “low educational stimulation” to be more specific. We believe that this paragraph is clearer now with this addition, and other psychosocial factors more clearly delineated in the subsequent paragraph. Revised text is below:</b>
Revision (page 4): “Established risk factors for the development of emotional, intellectual and behavioural disorders in LAMIC South Asian settings include low educational stimulation (Arun & Chavan, 2009),…….”
• Reviewer comment 3: There remains on pages 4-5 ambiguity about whether the lists of factors contributing to mental health risk or resilience are referring specifically to factors documented in South Asian countries or whether they are factors observed in other settings and hypothesized to be active in South Asia as well.
<b>We have added a sentence on page 5 to specify that these factors are observed across the globe and referred to evidence to their specific relevance in south Asia. The revised sentence is below:</b>
Revision (page 5): “These factors and their relationships to mental health risk are observed in numerous settings across the globe, and the aforementioned articles evidence their specific relevance to the development of mental health conditions in South Asia”
• Page 6: "This is particularly pertinent given specific observations that diagnostic and therapeutic services in primary care are lacking in India and Pakistan (Karim et al., 2004; Khandelwal et al., 2004; Regmi et al., 2004)". Again these citations are 18 years old; it would seem important when making statements about the presence or absence of particular services to have some more recent data or at least an assertion that there is no reason to believe that the situation has changed.
<b>We have updated the statements with recent citations. This updated statement is below:
</b>
Revision (page 6): “This is particularly pertinent given specific observations that diagnostic and therapeutic services in primary care are lacking in India and Pakistan (Agarwal, 2021; Hamdani et al., 2021)…..”
We thank you again for your time and feedback, and for consideration of this revised manuscript for publication. For any further information, please do not hesitate to contact the undersigned author.
Yours sincerely,
Azlina Amir Kassim
a.amirkassim@bangor.ac.uk