Introduction
Major depressive disorder (MDD) is one of the most common psychiatric disorders, with the World Health Organisation reporting that over 300 million people globally live with MDD, making this illness the leading cause of disability worldwide [1]. This manifests in enormous burdens on society, both in its direct effects on quality of life and productivity, as well as in its effects on healthcare services and various facets of the economy. Given its prevalence and impact, there has been much focus on improving treatment outcomes for MDD, culminating in a wide variety of well-established treatment guidelines that span primarily pharmacological and psychological interventions [Reference Gabriel, de Melo, Fraguas, Leite-Santos and Ribeiro2, Reference Gautam, Jain, Gautam, Vahia and Grover3]. Despite this, existing MDD care is suboptimal, which is no surprise given the complex pathogenesis, diagnostic heterogeneity, and high comorbidity associated with MDD [Reference Blazer, Kessler, McGonagle and Swartz4-Reference Menard, Hodes and Russo6]. Given these issues, it is no surprise that there is increasing focus on strategies to improve the management and care of MDD [Reference Almeida, Zizzi, Cattaneo, Comandini, Di Dato and Lubrano7-Reference Unutzer and Park9].
Our previous investigation of existing inefficiencies across the MDD care pathway revealed substantial treatment gaps in Europe and identified several recommendations to enhance MDD management [Reference Strawbridge, McCrone, Ulrichsen, Zahn, Eberhard and Wasserman10]. In summary, it was evident from this care pathway analysis that a large proportion of people who meet the criteria for MDD across Europe are not recognised by healthcare providers, are not accessing recommended first-line treatments, are not adequately followed up after initiating treatment, and are not able to access specialist or secondary care. There are many factors that perpetuate the prevalence of these treatment gaps, from patient-centric psychosocial circumstances to broader inefficiencies in implementation of government policy [Reference Hidaka11-Reference Wainberg, Scorza, Shultz, Helpman, Mootz and Johnson13]. Using a modified-Delphi method (a systematic and iterative approach to reaching consensus views among experts when experimental methodology is not suitable), several recommendations were generated, pertaining to improving diagnosis, optimising provision of treatment, and prioritising continuity of care. However, even if some of the recommendations could be successfully implemented, it is difficult to predict with accuracy how the MDD care landscape will change in the near future.
This uncertainty has become exacerbated with the emergence of the COVID-19 pandemic since the completion of our initial care pathway analysis. COVID-19 has exerted major impacts across systems globally, affecting overall healthcare utilisation and disease care as tremendous resources were re-allocated to COVID-19 management [Reference Kendzerska, Zhu, Gershon, Edwards, Peixoto and Robillard14, Reference Moynihan, Sanders, Michaleff, Scott, Clark and To15]. The pandemic thus has clearly affected mental healthcare, though the extent and nature of these impacts are not immediately obvious, given care pathways in mental health are especially complex and multifaceted [Reference Weaver, Coffey and Hewitt16, Reference Wiktorowicz, Di Pierdomenico, Buckley, Lurie and Czukar17]. It is clear that the COVID-19 pandemic has worsened existing health inequalities and increased the rates of several neuropsychiatric conditions [Reference Mishra, Seyedzenouzi, Almohtadi, Chowdhury, Khashkhusha and Axiaq18, Reference Xiong, Lipsitz, Nasri, Lui, Gill and Phan19]. However, it has simultaneously been suggested that the pandemic offers society an opportunity to re-design the fragmented care systems in place, shifting it towards a more patient-centric system with more inbuilt resilience [Reference Lal, Erondu, Heymann, Gitahi and Yates20, Reference Nimako and Kruk21].
This study is part of a larger European Brain Council value of treatment study, which aims to improve service provision for several neuropsychiatric conditions (including MDD) across Europe. Given the extensive influence of COVID-19, the recommendations stemming from this overarching study would hold suboptimal value without an understanding of how the pandemic has affected existing MDD care pathways. Therefore, in this scoping review, we aim to evaluate the effects of COVID-19 on pre-specified treatment gaps in MDD (detailed in our previous work) and to identify any strategies implemented to mitigate pandemic-related disruptions to MDD care.
Methods
This scoping review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) statement, which was developed to standardise the heterogenous methodology amongst existing scoping reviews [Reference Tricco, Lillie, Zarin, O’Brien, Colquhoun and Levac22]. This statement comprises a 22-item checklist developed by a panel of experts adhering to the Enhancing the QUAlity and Transparency Of health Research (EQUATOR) Network recommendations. A protocol for this scoping review was written prior to the searches being undertaken and published in MedRxiv following the searches [Reference Sually, Wong, Hidalgo-Mazzei, Quoidbach, Simon and Boyer23].
Search strategy
An electronic search of the PubMed and PsycINFO (via OVID) databases was conducted on 28 January 2022, for publications after 1 January 2020, a cut-off corresponding to the arrival of COVID-19 in Europe. Search strings relevant to MDD and COVID-19 were interrogated within all fields in PubMed, including record titles and abstracts, using the following search strategy: ((COVID-19 or COVID 2019 or severe acute respiratory syndrome coronavirus 2 or 2019 nCoV or SARS-COV2 or 2019nCoV or novel coronavirus) and (major depression or major depressive disorder or major depressive episode or MDD or MDE)). The search strategy was adapted for PsycINFO accordingly. The reference lists of articles yielded in the electronic search were also hand-searched to identify additional articles that possibly fit eligibility criteria.
Screening and eligibility criteria
Each study identified during database searching was imported into EndNote reference manager software for (automated and then manual) duplicate removal. W.L.E.W. and D.S. then examined titles and abstracts of the remaining publications against eligibility criteria. Following this initial screening, W.L.E.W. and D.S. evaluated the full texts of remaining articles for inclusion in this scoping review, with any doubts resolved upon discussion with all authors. Eligibility criteria were developed in consensus meetings between all authors, with a focus on broad criteria that would capture the maximum number of pertinent articles; original articles were included in this scoping review when they met the following criteria:
-
1. The relevant data were collected during the COVID-19 pandemic, pre-specified to include all studies after January 2020, to circumvent the varying timelines between countries.
-
2. The study was conducted in Europe. We defined Europe broadly as including all EU and EEA countries as well as those falling inside (not including contiguous transcontinental nations) the most commonly used boundaries [24]. The full list of countries comprises the following nations: Austria, Belgium, Bulgaria, Croatia, Republic of Cyprus, Czechia, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Poland, Portugal, Romania, Slovakia, Slovenia, Spain, Sweden, Iceland, Liechtenstein, Norway, Switzerland, United Kingdom, Ukraine, Belarus, Serbia (including Kosovo), Bosnia and Herzegovina, Moldova, Albania, North Macedonia, Montenegro, Andorra, San Marino, and Vatican City.
-
3. The study adopted either an interventional or observational design or was a relevant systematic review (with or without a meta-analysis). Non-systematic reviews, editorial or opinion articles, case reports, case series, and preclinical studies were excluded.
-
4. The study examined people with a diagnosis of MDD (full or sub-sample), established according to internationally recognised diagnostic criteria (e.g., ICD-10, DSM-5), which may have been recorded by a healthcare professional and/or rated using a structured or semi-structured diagnostic interview. This diagnosis had to be made at baseline or during the study assessment period.
-
5. The study examined working-age adults, as opposed to specific populations of young people (defined as under 18) or older people (defined loosely as aged over 65). This criterion was set due to variations in services for the young and elderly.
-
6. The study reported data pertaining to one or more of our pre-specified outcomes (relating to care pathways and continuity of care, as well as strategies for maintaining or improving care for people with MDD during COVID-19). These outcomes are detailed further in the below section entitled “Relevant outcomes”.
No language restrictions were implemented during the searching and screening process, provided that the team were able to identify a native speaker of that language able and willing to translate the text. As this is a scoping review, the studies that passed eligibility criteria were not formally assessed for methodological quality.
Relevant outcomes
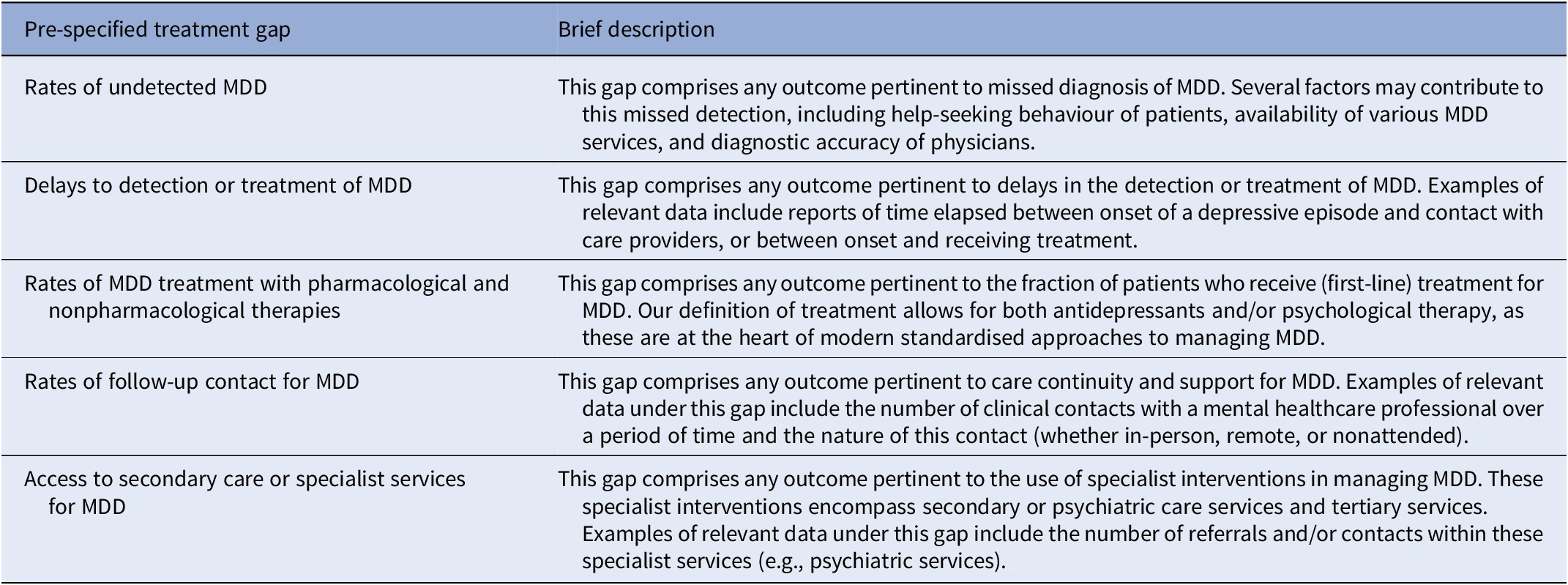
The outcome measures relevant to this scoping review relate broadly to several prespecified treatment gaps, and to mitigation strategies for disruption to MDD care. The prespecified treatment gaps align with our previous European Brain Council Value of Treatment in MDD care pathways analysis [Reference Strawbridge, McCrone, Ulrichsen, Zahn, Eberhard and Wasserman10], which evaluated treatment gaps prior to COVID-19. These treatment gap outcomes are described in more detail in Table 1. Mitigation strategies were relevant outcomes when trialled or implemented in any healthcare service setting to maintain or improve MDD care pathways disrupted during the pandemic. It was anticipated that these strategies would be primarily digital in nature, reflecting a shift in mental healthcare that was introduced even before the pandemic. Digital interventions broadly included any electronic methods that enabled service users with MDD to remain engaged with healthcare providers along care pathways, even without in-person interactions.
Table 1. Description of treatment gap outcomes that are pertinent to this scoping review
Data extraction and data synthesis
Data from included studies were extracted into a pre-designed Excel form. Data extracted included bibliographic information (such as authorship details and publication date), study characteristics (such as study design, location, and objectives), and summarised outcome data. The extracted data were summarised using tables and a narrative synthesis was constructed to analyse observed patterns and themes across the studies.
Results
Search and study selection
The electronic search of PubMed yielded 1084 records, while the search of PsycINFO via OVID yielded 660 records. An additional 12 studies were identified via hand searching of relevant reference lists. Following automated and manual duplicate removal, 1636 articles remained. Title and abstract screening of these articles removed 1470 articles, leaving 166 records for full-text screening. After evaluation of full texts, a further 155 articles were excluded, leaving 11 articles included in this scoping review. A flowchart of this search and screening process is presented in Figure 1.
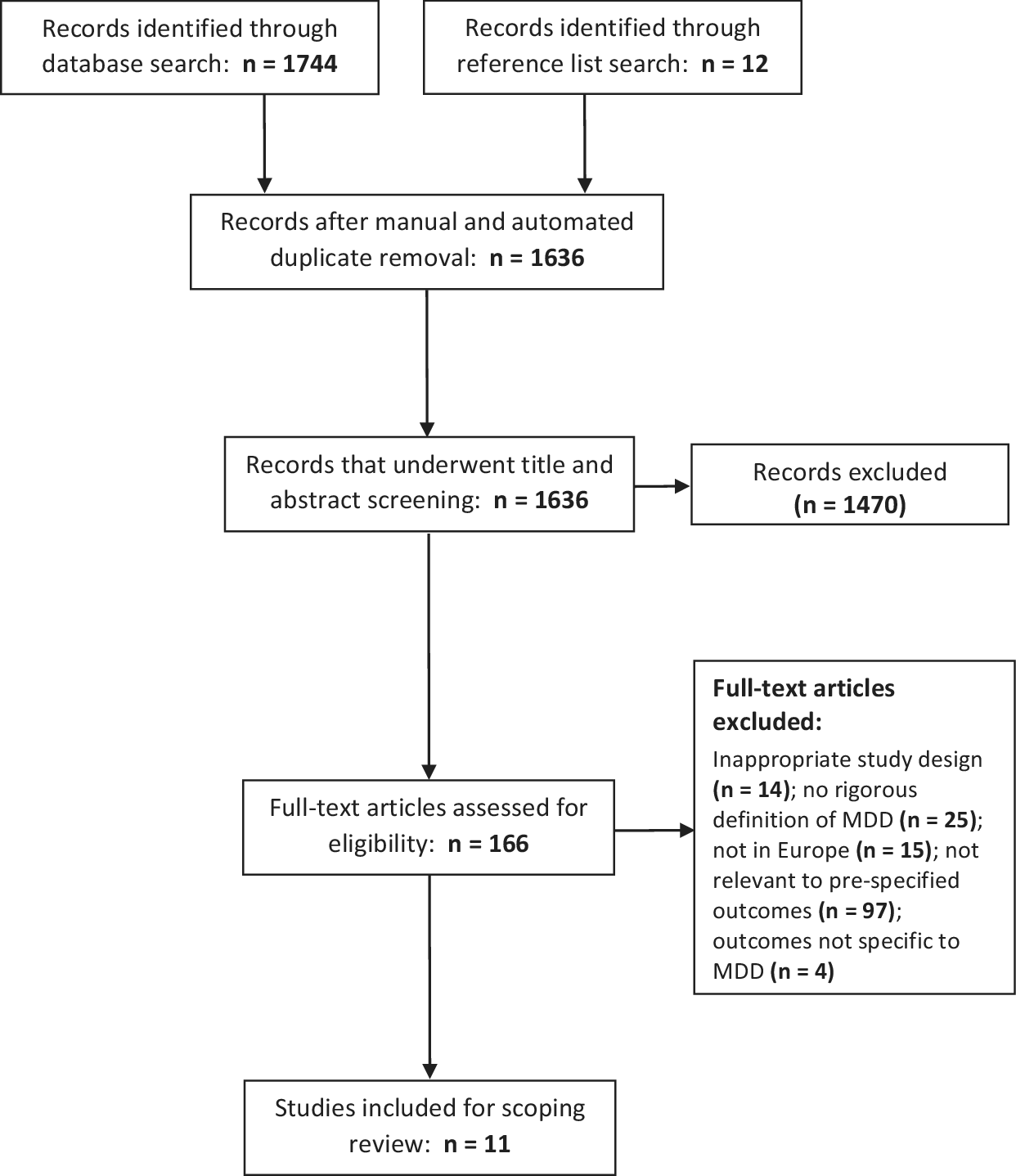
Figure 1. PRISMA flow diagram for included studies.
Summary of eligible studies
Eleven articles were identified after eligibility screening spanned seven countries across Northern, Western, and Southern Europe: Italy, United Kingdom, Germany, Spain, Denmark, France and the Netherlands. Nine of these studies were conducted in the period between March 2020 to May 2020, which corresponds to the introduction of nationwide restrictive measures (in many cases a lockdown) between March 9 and March 23 across the countries studied in this scoping review. Among the remaining two studies, one intersected with another period of lockdown in Italy [Reference Parolin, Benzi, Fanti, Milesi, Cipresso and Ascolto25], and the other immediately followed the loosening of restrictions in Denmark [Reference Kolbaek, Jefsen, Speed and Ostergaard26]. The timelines and pertinent restrictive measures for each study are summarised in Figure 2.
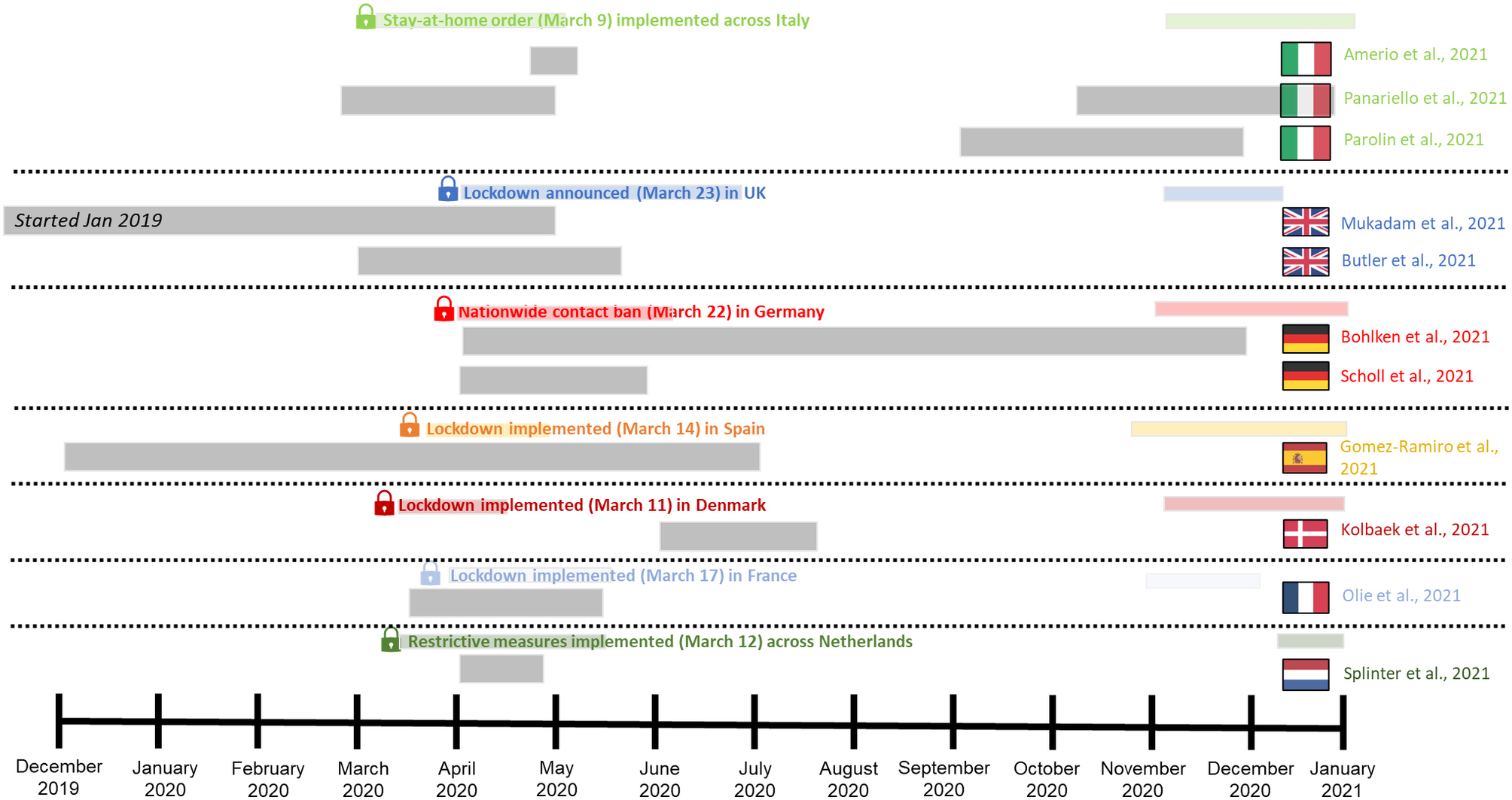
Figure 2. Graphic highlighting the timeline of studies eligible for this scoping review and associated restrictive measures by country. Coloured shading represents lockdown period, grey shading represents study period.
Impact of COVID-19 on treatment gaps in MDD care
Our scoping review search identified nine studies relevant to the aforementioned treatment gaps in MDD care (and two additional studies that were relevant to mitigation strategies), six of which investigated access to care. These studies are summarised in Table 2. Across these articles, there was a general tendency for a decrease in access to care during the COVID-19 pandemic: several studies reported changes in the number of clinical interactions relevant to MDD care, including number of psychiatric presentations to acute mental health assessment centres in London [Reference Mukadam, Sommerlad, Wright, Smith, Szczap and Solomou27], number of admissions to emergency psychiatric care in Barcelona [Reference Gomez-Ramiro, Fico, Anmella, Vazquez, Sague-Vilavella and Hidalgo-Mazzei28], number of hospitalisations to a psychiatric ward in Bologna [Reference Panariello, Longobardi, Cellini, De Ronchi and Atti29], and number of referrals to inpatient and liaison psychiatry services in London [Reference Butler, Delvi, Mujic, Broad, Pauli and Pollak30]. There was consistency in the findings, with number of clinical interactions being reduced in all instances, to varying degrees. Olié and Dubois [Reference Olié, Dubois, Benramdane, Guillaume and Courtet31] further reported that 53.3% of participants with lifetime MDD did not have access to psychiatric care during the pandemic-mediated lockdown period in France. A study of general practitioner records in Germany reported that frequency of depressive disorder diagnoses was down by 11% in the second quarter of 2020, when the first lockdown was implemented, relative to the same period from 2017 to 2019, again indicative of the reduced access to care following the COVID-19 pandemic [Reference Bohlken, Kostev, Riedel-Heller, Hoffmann and Michalowsky32]. A cross-sectional survey study further found that people with depression were more likely to avoid primary care during the pandemic [Reference Splinter, Velek, Ikram, Kieboom, Peeters and Bindels33].
Table 2: Summary of identified studies that investigate how the COVID-19 pandemic affected pre-specified treatment gaps in MDD care
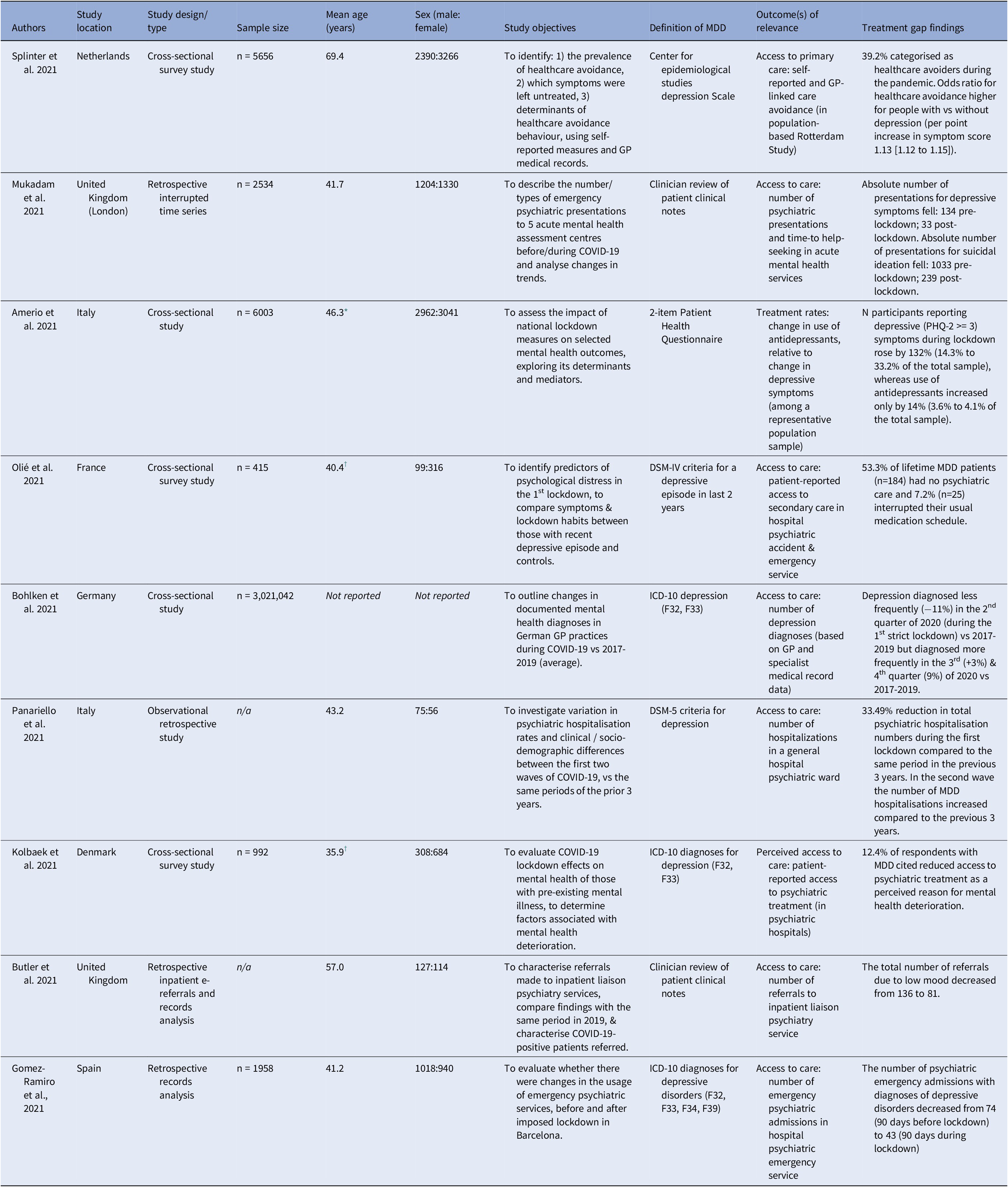
* Only information about the number of people in three age range categories (18-34, 35-54, and 55-74) were provided. Therefore, mean age was estimated using the the mid-point of each age range category.
† Only minimum, maximum, and median age, as well as sample size, were provided. Therefore, mean age was estimated using these parameters.
In addition, one study explored patients’ perception on the effects of changing access to care: Kolbaek and Jefsen [Reference Kolbaek, Jefsen, Speed and Ostergaard26] reported that 12.4% of respondents with MDD in a Danish population cited reduced access to psychiatric treatment as a perceived reason for their mental health deterioration. The final identified study explored rates of treatment as an outcome, reporting that the use of antidepressants increased by 14% following the pandemic-induced lockdown, while the number of participants reporting depressive symptoms increased far more dramatically, by 132% [Reference Amerio, Lugo, Stival, Fanucchi, Gorini and Pacifici34]. No studies explored delays to the detection or treatment of depression, and there were no reports on the rates of follow-up contacts.
Mitigation strategies for COVID-19 disruptions to MDD care
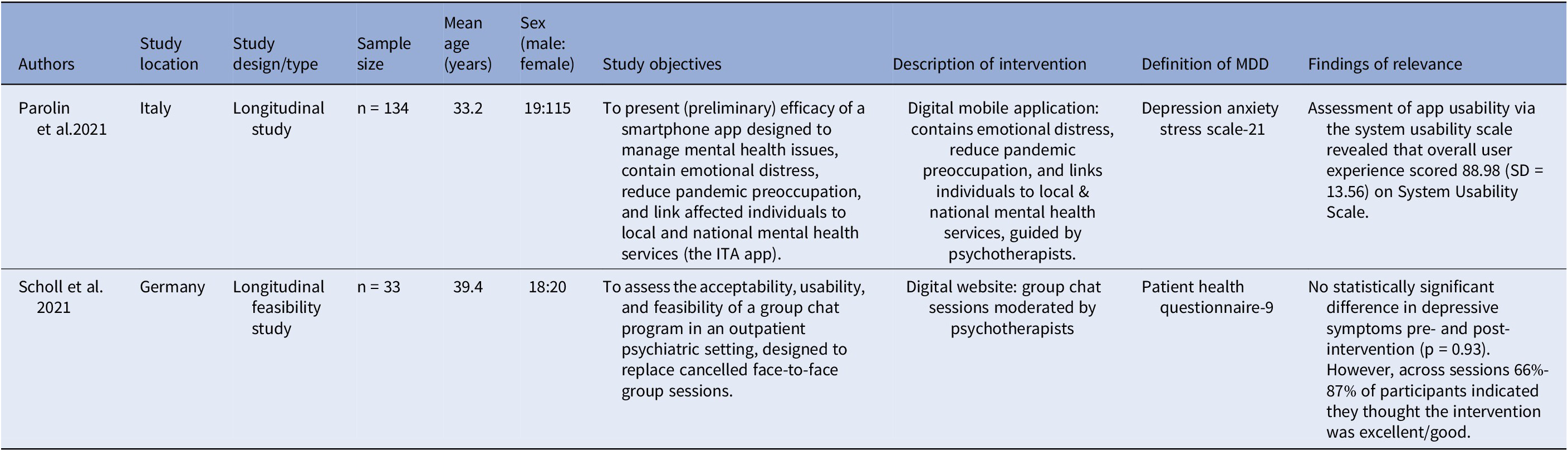
Two included studies, summarised in Table 3, explored strategies implemented to mitigate COVID-19-related disruptions to MDD care. Both were longitudinal studies investigating digital interventions. Parolin et al. [Reference Parolin, Benzi, Fanti, Milesi, Cipresso and Ascolto25] aimed to explore the efficacy of a new smartphone app in Italy (“Italia Ti Ascolto”), which was introduced to manage several pandemic-related disruptions to mental health care, by offering several services including emotional distress management and linkage with mental health services. Overall user experience scored 88.98 (SD = 13.56) on the System Usability Scale [Reference Brooke35], a usability scale ranging from 0 to 100, indicating a strong willingness among service users to shift towards digital interventions. However, there was no investigation of how the application affected care or psychopathological outcomes. Scholl et al. [Reference Scholl, Kohls, Gorges, Steinbrecher, Baldofski and Moessner36] investigated the feasibility of shifting service users from face-to-face group therapy to an online therapist-guided group chat programme in Germany. They found that there were no statistically significant differences in reported symptoms following the intervention, yet between 66 and 87% of participants in online group chats reported that they felt the intervention was good or excellent, suggesting some acceptability of this novel digital intervention following COVID-19. Several other digitally-enabled approaches to mental health management were identified during the initial search; for example, one report evaluated the utility of an application centred around mindfulness and psychotherapeutic support [Reference Bauerle, Jahre, Teufel, Jansen, Musche and Schweda37], while another reviewed mental health apps focused on evidence-based treatment in Australia [Reference Marshall, Dunstan and Bartik38]. These articles, however, did not meet our specific eligibility criteria pertinent to care pathways in Europe.
Table 3: Summary of identified studies that investigated mitigation strategies for managing COVID-19-related disruptions to MDD care
Discussion
Summary of results
The studies identified in this scoping review highlighted that the COVID-19 pandemic appeared to exacerbate some of our pre-specified treatment gaps, particularly during the first wave of COVID-19 across the Spring to Summer of 2020. Across the seven countries yielded in our search, restriction measures were enforced around approximately the same time, initially across March, then again across November to December in response to the second COVID-19 wave. All identified studies were conducted within a similar timeframe and either followed or intersected with the introduction of the initial restriction measures; however, the full nature of these restrictions did vary between countries. For instance, the United Kingdom and Italy differed in severity of at-home isolation orders, while the timing of lockdown policies between the United Kingdom and Germany differed [Reference Meintrup, Nowak-Machen and Borgmann39]. There was nevertheless a common “lockdown” period of restricted contact shared across all countries in this review. Organisation of care, too, varied between countries, with the European Psychiatric Association reporting a significant difference in mental health service delivery between countries during the first wave [Reference Rojnic Kuzman, Vahip, Fiorillo, Beezhold and Skugarevsky40]. These differences pertained to variations in hospital-based care for mental health, to the creation of specialist units, and to the guidelines introduced by professional associations; all these factors are likely to affect (to some degree) our findings, though a full exploration of these disparities is beyond the scope. As this scoping review did not focus on capturing the full background context of government measures and care structures in each region, the trends we discuss below must therefore be interpreted with some degree of caution.
Investigations from the United Kingdom, Denmark, Spain, Italy, and France reported a reduction in access or perceived access to secondary or inpatient care, reflected in either reduced clinical contact or patient-reported decreases in clinical access [Reference Kolbaek, Jefsen, Speed and Ostergaard26-Reference Olié, Dubois, Benramdane, Guillaume and Courtet31]. Studies of primary care services also indicated a reduction in general practitioner visits for depression in the Netherlands and Germany during the pandemic, compared to pre-pandemic rates [Reference Bohlken, Kostev, Riedel-Heller, Hoffmann and Michalowsky32, Reference Splinter, Velek, Ikram, Kieboom, Peeters and Bindels33]. A single study assessing rates of self-reported pharmacological treatment for MDD [Reference Amerio, Lugo, Stival, Fanucchi, Gorini and Pacifici34], found a substantial increase in reported depressive symptoms that was not commensurate with a more modest increase in antidepressant usage. This discrepancy could imply a reduction in the proportion of patients receiving antidepressants during the pandemic. Although this evidence is patient-reported and indirect, it is supported by a study in the United Kingdom, which highlighted that rates of increasing antidepressant prescriptions in 2020 were not significantly different from pre-pandemic trends [Reference Rabeea, Merchant, Khan, Kow and Hasan41]. These results are consistent with other reports that underscore how COVID-19 has decreased overall healthcare utilisation, a phenomenon that can be explained by the restrictions imposed by pandemic-induced lockdowns, fear of exposure to the virus, and inadequate availability of healthcare resources, amongst others [Reference Moynihan, Sanders, Michaleff, Scott, Clark and To15, Reference Nunez, Sreeganga and Ramaprasad42].
We were cognisant to enforce relatively loose inclusion criteria for the definition of MDD in this review, given the limited available data addressing our treatment gaps. Despite this, only nine pertinent studies were identified, and only a few of the pre-specified treatment gaps were addressed across these reports. While some trends were evident in this scoping review, these cannot be interpreted with certainty, as there is heterogeneity among the outcomes evaluated across studies. Several of the studies employed patient-reported data to draw conclusions about the effect of the pandemic, but this only acts as a proxy for actual changes in relevant outcomes, with the accuracy of self-reported data varying heavily [Reference Hafferty, Campbell, Navrady, Adams, MacIntyre and Lawrie43, Reference Short, Goetzel, Pei, Tabrizi, Ozminkowski and Gibson44]. Moreover, several investigations were conducted at a very small number of clinical sites, such that the absolute numbers assessed were often very small; it is thus difficult to aver the generalisability of these conclusions. Rates of undetected MDD could only be crudely assessed by evaluating the number of positive diagnoses during the pandemic, while no identified articles explored follow-up contacts for MDD and delays to the detection of MDD as outcomes.
It is important to note that there were a number of studies identified in our systematic search that did not meet our inclusion criteria, but that did have relevant insights to support some of the findings. Several articles focused on treatment gaps broadly across psychiatric care rather than specifically for MDD. For instance, Sampson and Wright [Reference Sampson, Wright, Dove and Mukadam45] found a decrease in referrals to psychiatric liaison services across North Central London during the first pandemic wave, while Pignon and Gourevitch [Reference Pignon, Gourevitch, Tebeka, Dubertret and Cardot46] reported reduced emergency psychiatric consultations during the first 4 weeks of lockdown in Paris and its suburbs. A cross-sectional study in Austria further reported a decrease in the percentage of participants that self-reported treatment for broad mental disorders during lockdown [Reference Simon, Helter, White, van der Boor and Laszewska47]. While not specific to MDD, these findings altogether corroborate the notion of reduced access to acute care, secondary care or rates of treatment in MDD management during the pandemic. Rates of broader psychiatric treatment were also peripherally assessed in several articles: in a survey of university students in France, Wathelet and Duhem [Reference Wathelet, Duhem, Vaiva, Baubet, Habran and Veerapa48] reported that 6.8% were seeing a professional for mental health reasons, far less than the 16.1% that were assessed with MDD based on the Beck Depression Inventory. Across three Dutch case-control cohorts, Pan and Kok [Reference Pan, Kok, Eikelenboom, Horsfall, Jorg and Luteijn49] reported that only 55% of participants with a lifetime mental health condition were undergoing treatment during the pandemic. While these investigations for the rate of treatment are further suggestive of impaired healthcare provision for psychiatric conditions and thus MDD, these statistics were not compared to pre-pandemic statistics, such that direct comparison of treatment rates for MDD was not possible.
There were also a large number of articles that did not explore our outcomes of interest but did directly assess changes in MDD prevalence during COVID-19, generally highlighting increased prevalence in depressive disorders following the pandemic [Reference Babicki, Kowalski, Bogudzinska and Mastalerz-Migas50-Reference Winkler, Formanek, Mlada, Kagstrom, Mohrova and Mohr53]. This relationship has been further underscored in several comprehensive systematic reviews, which suggest worsened levels of overall psychological distress during COVID-19 [Reference Xiong, Lipsitz, Nasri, Lui, Gill and Phan19, 54]. This was concomitant with a greater need for therapeutic support and heightened public concern about treatment impairment [Reference Favreau, Hillert, Osen, Gartner, Hunatschek and Riese55]. Given the COVID-19-mediated impairment of MDD care provision identified in this review, this is a particularly serious public health concern. Altogether, this evidence emphasises the need to ameliorate these worsened treatment gaps and make MDD care more resilient to external factors.
To this end, we also attempted to collate evidence of mitigation strategies introduced during the pandemic to improve MDD care. However, given our inclusion criteria, only two studies were included in our synthesis [Reference Parolin, Benzi, Fanti, Milesi, Cipresso and Ascolto25, Reference Scholl, Kohls, Gorges, Steinbrecher, Baldofski and Moessner36]; both these studies trialled digital interventions, one to replace face-to-face group therapy sessions and the other to link service users with mental health services, indicating that participants were receptive to the usage of these tools, though their efficacy in managing MDD is unclear. Once again, our search did identify a number of other studies exploring digital interventions, but that did not strictly assess an outcome of interest or was too broad in nature. For instance, Bauerle and Jahre [Reference Bauerle, Jahre, Teufel, Jansen, Musche and Schweda37] evaluated an e-mental health intervention integrating mindfulness and cognitive behavioural therapy, highlighting some therapeutic efficacy without addressing implications on care provision. Olwill and Mc Nally [Reference Olwill, Mc Nally and Douglas56] surveyed psychiatrists about their experiences with phone consultations, but this was for broader mental health concerns. While these articles did not meet our inclusion criteria, they nonetheless illustrate how the pandemic has expedited a shift into digital or remote solutions for mental health care more generally, a trend likely to continue in the post-pandemic era given the reported efficacy of such solutions even in non-pandemic contexts [Reference Moshe, Terhorst, Philippi, Domhardt, Cuijpers and Cristea57, Reference Torous, Bucci, Bell, Kessing, Faurholt-Jepsen and Whelan58]. Clearly, more work needs to be done to identify how these innovations have affected, and continue to affect, MDD care during COVID-19. Our search strategy failed to identify articles that offered detailed evaluations on how remote care and the use of teleconsultations during COVID-19 affected MDD service provision in particular, though there was evidence for increased telemedicine usage across mental health [Reference Abraham, Jithesh, Doraiswamy, Al-Khawaga, Mamtani and Cheema59, Reference Patel, Irving, Brinn, Broadbent, Shetty and Pritchard60]; to this end, it would be useful to have more detailed evaluations on how the general shift to teleconsultations across healthcare has affected specific MDD care pathways.
In addition to the aforementioned mitigation strategies, it is important to consider the extent to which restructuring of mental health care services addressed COVID-19-mediated gaps in psychiatric care provision. This re-organisation of care arose due to a need to divert people away from acute hospitals (to reduce contact and relieve hospital burden) while maintaining some level of support for individuals suffering from mental health conditions. While our search strategy did not yield MDD-specific reports on this topic, several reports highlight how community mental health services across the world continued to provide broad psychiatric care and support throughout the pandemic, despite the many challenges they faced [Reference Kopelovich, Monroe-DeVita, Buck, Brenner, Moser and Jarskog61-Reference Vigo, Patten, Pajer, Krausz, Taylor and Rush63]. Furthermore, it is clear that these community services adopted digital technologies and telemedicine to ensure care delivery in a safe and optimal manner [Reference Burton, Wall and Perkins64, Reference Sklar, Reeder, Carandang, Ehrhart and Aarons65], with relatively favourable perceptions of this digital shift, which may have long-term implications for the how community mental health resolves to bridge the gaps in MDD, and psychiatric, care provision.
Strengths and limitations
There were several strengths to this scoping review. This study is the first to broadly investigate the effects of COVID-19 on pre-existing treatment gaps, and more broadly care provision, specific to MDD in Europe. Moreover, we conducted this review in accordance with rigorous PRISMA-ScR guidelines and adopted a systematic approach to our search and screening methodology, to ensure we properly synthesised evidence on this topic. We further registered a protocol prior to the conduct of this study, adhering to it to achieve objectivity and transparency in our review. Our eligibility criteria were also meticulously developed in several consensus meetings to ensure the review was comprehensive while relevant to MDD care provision, and we permitted studies that were not written in English for better coverage, though this did not facilitate the inclusion of additional studies.
Limitations of this study include the lack of critical appraisal for study quality and the broad nature of the data synthesis, though these limitations are a staple in scoping reviews. The eligibility criteria adopted in this review are concomitant with several other limitations: our MDD criteria were relatively loose to maximise scope, and certain subgroups were not investigated at length (e.g., the older adult population). Despite some methodological leniency, there were only a small number of articles eligible for analysis following our rigorous screening, which limits the interpretation of our findings. There are limitations to the generalisability of our findings across continental Europe, given the small number of countries reported on in this review, primarily concentrated across Northern, Western, and Southern Europe. Certain treatment gaps were left completely unaddressed, meaning we do not have a complete picture of how COVID-19 has affected MDD care provision in Europe. Furthermore, there was much methodological heterogeneity across studies and therefore a lack of standardisation, limiting the types of analysis that could be conducted with the results. We also acknowledge the possibility of missed relevant articles because of delays in indexing and because this is a fast-moving field. A final important limitation of this scoping review is the difficulty in directly comparing the extent of treatment gaps and mitigation strategies during the pre- and peri-pandemic periods. For example, while Butler and Delvi [Reference Butler, Delvi, Mujic, Broad, Pauli and Pollak30] found a 40.4% decrease in number of people accessing secondary care from 2019 to 2020, we cannot estimate comparable rates for the continued or post-pandemic period, rendering it difficult to assess the complete role of COVID-19 in moderating this particular treatment gap.
Future directions
In the peri- and post-pandemic era, it will be important to collate and re-evaluate several of the outcomes from the studies identified in this scoping review. There is a need to analyse longer-term observational data from MDD care services and wider public samples, in order to determine the nature and extent of treatment gaps in MDD care, particularly during the latter stages of and gradual transition from the pandemic. A fully developed understanding of how the pandemic impacted MDD care provision in Europe would enable comparison with the implementation of recommended guidelines, and importantly enable us to capture the effects of both positive (for instance, via the implementation of guideline recommendations) and negative events (like the pandemic) on MDD care.
This scoping review also highlighted several additional studies that could be conducted to help develop a full perspective on the impacts of COVID-19 on MDD care in Europe. There is still much scope to investigate the digital mitigation strategies implemented for management of MDD during the pandemic. The use of digital strategies in MDD has been a topic of interest even prior to the pandemic, with a large variety of tools deployed with mixed efficacy. For instance, evidence for internet-based cognitive behavioural therapy is fairly mature [Reference Karyotaki, Efthimiou, Miguel, Bermpohl, Furukawa and Cuijpers66], though the efficacy of other innovations, such as virtual reality, chatbots, and smartphone applications, has yet to be fully validated [Reference Torous, Bucci, Bell, Kessing, Faurholt-Jepsen and Whelan58] and requires more study. Telepsychiatry too has grown extensively in popularity during the pandemic, though there is still scope for refinement of its implementation [Reference Greenhalgh and Wherton67]. Our search found that many such digital interventions have been trialled and implemented during the pandemic; however, many investigations to date did not meet our inclusion criteria due to a lack of specificity for MDD service provision. This lack of specificity was a common occurrence for articles that did not pass screening for our eligibility criteria; while understandable given the comorbidity of MDD with other mental health disorders, it will be important to conduct additional investigations specific to MDD care, as treatment pathways in this subgroup already contain complexities. During our initial search, there were also several pertinent articles for specific subgroups (such as student populations) that did not meet eligibility criteria – it would thus be useful to conduct a similar review surveying MDD care pathways in these subgroup populations. For example, an investigation into how COVID-19 affected MDD care provision in the elderly population would be interesting, as they were likely impacted in different manners, due to various subgroup-specific factors, including the presence of comorbidities and differing access or skills with digitally enabled solutions that were trialled in the pandemic. Several of our pre-specified treatment gaps – especially delays to MDD detection and rates of follow-up – were not fully addressed by the current literature, further reinforcing that additional retrospective analysis would be useful. While there were longitudinal investigations, none included sufficient follow-up to enable a complete evaluation of COVID-19-related trends.
Despite the uncertainty around many of the conclusions from this scoping review, stemming from a limited amount of available data, treatment gaps for MDD appeared to be exacerbated by COVID-19. It will therefore be important to re-evaluate previous recommendations for MDD care to ensure they are robust in the face of unpredictable events. Treatment gaps in MDD care clearly remain extensive and problematic, so it is more critical than ever to implement standardised solutions throughout the pathway.
Acknowledgements
The authors acknowledge the assistance and support from all members of the European Brain Council Value of Treatment Research Working Groups (particularly the MDD group). We are grateful to Dr. Fabio Panariello, who kindly provided us with additional data that was key in this manuscript. We also acknowledge the contributions of Dr. Mutahira Qureshi, who offered advice and translation support while this research was conducted.
Financial support
This work was supported by the European Brain Council (EBC). This work is also supported by the National Institute for Health Research (NIHR) Maudsley Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London.
Competing interest
R.S. has received honoraria from Janssen. A.H.Y. has been commissioned to provide lectures and advice to all major pharmaceutical companies with drugs used in affective and related disorders; has also undertaken investigator-initiated studies funded by Astra Zeneca, Eli Lilly, Lundbeck, and Wyeth. V.Q. is employed at the European Brain Council (funder) and P.B. undertakes work for the European Brain Council. D.H.M has received CME-related honoraria and served as a consultant for Abbott, Angelini, Ethypharm Digital Therapy, and Janssen-Cilag with no financial or other relationship relevant to the subject of this article. J.S. has received EBC academic expert honoraria with no financial or other relationship relevant to the subject of this article. W.L.E.W and D.S. declare no competing interests.










Comments
No Comments have been published for this article.