Introduction
Homelessness is associated with a wide range of social and health problems and brings especially high costs to society: the vast majority of homeless people are unemployed, have very low incomes (Fischer et al., Reference Fischer, Shinn, Shrout and Tsemberis2008; Roy et al., Reference Roy, Crocker, Nicholls, Latimer and Ayllon2014), and have a high level of psychiatric hospital use, including numerous contacts with justice and criminal services (Hirschtritt and Binder, Reference Hirschtritt and Binder2017).
The current care of these homeless patients has been based, at best and after years of support, on providing accommodations subject to the initiation of treatment and psychiatric follow-up, also known as the Treatment First model. In 2008, a literature review (Kyle and Dunn, Reference Kyle and Dunn2007) suggested that when housing eligibility is not dependent on the patient's treatment compliance, this may ultimately encourage people to engage freely in comprehensive medical and social care. Thereafter, a growing number of studies confirmed the effectiveness of this approach, known as the Housing First (HF) programme, for treating homeless people with mental health problems. The HF model was developed in the USA to address homelessness among people with mental health issues and concurrent substance abuse (Tsemberis and Eisenberg, Reference Tsemberis and Eisenberg2000; Tsemberis et al., Reference Tsemberis, Gulcur and Nakae2004). The originality of this approach is that it reverses the traditional Treatment First model; HF entails: (a) prioritising permanent housing for homeless people with mental disorders, even if they use and abuse alcohol or substances; and (b) delivering recovery-oriented services promoting consumer choice via a support team (Tsemberis et al., Reference Tsemberis, Gulcur and Nakae2004). The HF intervention leads to a wide range of intangible benefits after 1–2 years, namely, a majority of HF users remain in the same dwelling, re-establish family ties, and exhibit a decreased use of hospital services (Stefancic and Tsemberis, Reference Stefancic and Tsemberis2007; Stergiopoulos et al., Reference Stergiopoulos, Hwang, Gozdzik, Nisenbaum, Latimer, Rabouin, Adair, Bourque, Connelly, Frankish, Katz, Mason, Misir, O'Brien, Sareen, Schutz, Singer, Streiner, Vasiliadis and Goering2015; Aubry et al., Reference Aubry, Goering, Veldhuizen, Adair, Bourque, Distasio, Latimer, Stergiopoulos, Somers, Streiner and Tsemberis2016; Baxter et al., Reference Baxter, Tweed, Katikireddi and Thomson2019; Tinland et al., Reference Tinland, Loubiere, Boucekine, Boyer, Fond, Girard and Auquier2020). However, the role of the HF model for people who use alcohol and substances is still unclear (Kertesz et al., Reference Kertesz, Crouch, Milby, Cusimano and Schumacher2009; Tsai et al., Reference Tsai, Mares and Rosenheck2010; Padgett et al., Reference Padgett, Stanhope, Henwood and Stefancic2011; Kirst et al., Reference Kirst, Zerger, Misir, Hwang and Stergiopoulos2015; Cherner et al., Reference Cherner, Aubry, Sylvestre, Boyd and Pettey2017), and there remains a lack of consensus about its benefits over a longer period of time in terms of recovery.
Recovery is commonly recognised as a multidimensional concept (Zimmerman et al., Reference Zimmerman, McGlinchey, Posternak, Friedman, Attiullah and Boerescu2006; Cuijpers, Reference Cuijpers2020; Fava and Guidi, Reference Fava and Guidi2020). Going beyond the one-dimensional concept of recovery in its clinical aspect, in which intervention effectiveness is mostly defined by reductions in symptom severity with secondary measures, including hospitalisation outcomes and medication use (Turton et al., Reference Turton, Wright, White and Killaspy2010), a broader definition of recovery encompasses a focus on well-being, which is more in line with patients' perspectives on recovery. Mental health literature emphasises that recovery processes involve continuous cross-dimensional interactions between clinical recovery, personal recovery (i.e. taking control of one's life through individual responsibility, autonomy, empowerment, overcoming stigma and having supportive relationships), functional recovery (i.e. meaningful participation in society) or social recovery (i.e. restoring one's sense of purpose and meaning). There is evidence indicating that the conceptual distinction between clinical recovery and other dimensions is predominant (Bellack, Reference Bellack2005; Jose et al., Reference Jose, Ramachandra, Lalitha, Gandhi, Desai and Nagarajaiah2015; Soundy et al., Reference Soundy, Stubbs, Roskell, Williams, Fox and Vancampfort2015; van Weeghel et al., Reference van Weeghel, van Zelst, Boertien and Hasson-Ohayon2019). We hypothesised that this intervention, with greater community-based support (teams and housing), may promote both clinical recovery and recovery in a broader sense, which we define as the recovery process, but which includes all the concepts described above (Davidson et al., Reference Davidson, Tondora, O'Connell, Kirk, Rockholz and Evans2007; Stotland et al., Reference Stotland, Mattson and Bergeson2008; Noiseux et al., Reference Noiseux, Tribble St-Cyr, Corin, St-Hilaire, Morissette, Leclerc, Fleury, Vigneault and Gagnier2010; Weijers et al., Reference Weijers, Rasing, Creemers, Vermulst, Schellekens and Westerhof2021).
A French randomised controlled trial, Un Chez Soi d'Abord, sought to evaluate the HF programme's effectiveness compared to the Treatment-As-Usual (TAU) approach over 2 years. The French HF programme is similar to those conducted in the USA or Canada, although the target population has a high level of need that is defined, among other conditions, by the presence of severe mental illness. The multidisciplinary support teams therefore followed an assertive community treatment (ACT) model that offers more intense support than case management (Lehman et al., Reference Lehman, Dixon, Hoch, Deforge, Kernan and Frank1999; Vanderlip et al., Reference Vanderlip, Williams, Fiedorowicz and Katon2014). At the 2-year follow-up, no differences were found between the two approaches in terms of personal recovery, as evaluated using the Recovery Assessment Scale (RAS) (Girard et al., Reference Girard, Tinland, Bonin, Olive, Poule, Lancon, Apostolidis, Rowe, Greacen and Simeoni2017), whereas the clinical results were encouraging and similar to the North American outcomes, with a significant decline in symptoms and hospital length of stay (Stergiopoulos et al., Reference Stergiopoulos, Hwang, Gozdzik, Nisenbaum, Latimer, Rabouin, Adair, Bourque, Connelly, Frankish, Katz, Mason, Misir, O'Brien, Sareen, Schutz, Singer, Streiner, Vasiliadis and Goering2015; Tinland et al., Reference Tinland, Loubiere, Boucekine, Boyer, Fond, Girard and Auquier2020). Following these primary findings, the HF model was included in French planning law at the end of 2017, and the French government has made substantial investments to implement HF throughout the country. Such a programmatic public strategy requires ongoing evaluation to inform decision-makers whether short-term effects are sustained beyond the 2-year period. This is particularly important, as the Chez Soi d'Abord population is suffering from schizophrenia and bipolar disorder. In such populations, the recovery process takes a long time, usually 2–5 years (Robinson et al., Reference Robinson, Woerner, McMeniman, Mendelowitz and Bilder2004; Haro et al., Reference Haro, Altamura, Corral, Elkis, Evans, Malla, Krebs, Zink, Bernasconi, Lalonde and Nordstroem2015). It is therefore essential to document the effects of HF, and particularly recovery outcomes, beyond 24 months to provide guidance to stakeholders (both professionals and decision-makers) regarding the improvement of the HF programme. To our knowledge, no randomised controlled studies have yet assessed the effects of HF on recovery outcomes based on 4-year follow-up data in patients with severe mental illness (Van Eck et al., Reference Van Eck, Burger, Vellinga, Schirmbeck and de Haan2018). The current study fills this gap by determining the effects of HF v. TAU on recovery outcomes, clinical and recovery processes, housing stability, hospital service use, quality of life (QoL) and addiction problems based on 4 years of data from the Un Chez Soi d'Abord trial. We posited that while clinical recovery can be achieved quickly in the context of HF programme, other dimensions of recovery deserve to be assessed over longer periods (Aubry et al., Reference Aubry, Goering, Veldhuizen, Adair, Bourque, Distasio, Latimer, Stergiopoulos, Somers, Streiner and Tsemberis2016; Van Eck et al., Reference Van Eck, Burger, Vellinga, Schirmbeck and de Haan2018).
Methods
Trial design
Un Chez Soi d'Abord is a randomised controlled trial involving homeless adults with severe mental illness from four French cities: Paris, Marseille, Toulouse and Lille. The participants were randomised 1:1 to the HF TAU groups, stratified by site. Details of the RCT protocol have been previously described (Tinland et al., Reference Tinland, Fortanier, Girard, Laval, Videau, Rhenter, Greacen, Falissard, Apostolidis, Lancon, Boyer and Auquier2013). The relevant institutional review boards approved the trial. The inclusion period was from August 2011 to April 2014. The initial follow-up period was 2 years. Subsequently, we decided to continue the follow-up for an additional 2 years (for a total of 4 years). The participants were asked to sign a consent form for this extension, and were kept in the same randomisation group for analysis. During the 4-year follow-up, there was no possibility to move from one group to the other: for participants initially in the control group, access to housing could only be achieved through the regular offer; the ACT teams maintained an almost identical follow-up for the people in the HF programme and if HF participants wished to stop the team's support or if they moved into regular housing, they were kept in the HF group (intention-to-treat analysis).
Participants
The participants were recruited from homeless shelters, mobile outreach teams, community mental health teams, hospitals and prisons. At each site, trained research assistants and a psychiatrist checked the eligibility criteria within 24 h of referral, explained the procedures to all enrolled participants, and obtained informed consent. Eligible study patients were over 18 years old, absolutely homeless (no fixed place to stay for at least the previous 7 nights, with little likelihood of finding a place in the upcoming month) or precariously housed (housed in a night shelter or homeless hostel as a primary residence AND with history of two or more episodes of being absolutely homeless in the past year OR one episode of being homeless for at least 4 weeks in the past year), and covered by French state health insurance. Patients were required to have a ‘high level of needs’, defined as schizophrenia (SCZ) or bipolar disorder (BD) diagnosed according to the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV-TR; APA, 2000) moderate-to-severe disability according the Multnomah Community Ability Scale (score ⩽62; range 17–85) (Barker et al., Reference Barker, Barron, McFarland and Bigelow1994), and at least one of the following criteria: (i) ⩾2 hospitalisations for mental illness over the past 5 years; (ii) comorbid alcohol or substance use disorder; and (iii) arrested or incarcerated within the previous 2 years. The exclusion criteria were the inability to provide informed consent, having dependent children or pregnancy.
Interventions
The French HF model offers independent housing with initial housing subsidies and ACT provided by a mobile support team. Access to housing started using the rental intermediation system (IML), which allows access to the private housing market for social landlords and their subtenants, provides a guarantee of rent and the repair of potential damages, and improves the security of (sub)tenants, but also limits direct leases between tenants and landlords. Under sufficient resource conditions, the HF participant becomes a master tenant without any changes in the flat or in the amount of rent. In parallel to independent housing, individualised support with a multidisciplinary team, in which the client can set their own goals at their own pace, is offered and lasts for as long as the client considers it useful.
In the TAU group, people's housing situations vary. They may live on the streets, in squats/slums, or stay with friends or family, and have access to usual care; that is, pre-existing programmes and services for the homeless, including but not limited to outreach teams and day-care facilities. Homeless people may also have access to the following types of accommodations: (i) ‘emergency’ shelters, with each place renegotiated each evening; (ii) transitional shelters in which people also have access to care and integration services (the maximal duration of stay is 6 months); (iii) specific accommodations that address the unique needs of homeless people such as women's shelters, residential and medical accommodations with longer lengths of stay; and (iv) independent housing, which is also accessible (cf., an ‘enforceable’ right to housing has been in place since 2007) through a rather similar IML instrument.
Measures
The outcomes were assessed every 6 months ± 30 days between baseline and 24 months (M0 to M24), and then every 12 months ± 60 days (M36 and M48) (see eTable 1 in the online Supplementary material for a reliability description of each measure).
We broadly defined personal recovery, as opposed to clinical recovery based on symptom remission and functional improvement, as rehabilitation and growth after illness and assessed using the RAS (Corrigan et al., Reference Corrigan, Salzer, Ralph, Sangster and Keck2004; Girard et al., Reference Girard, Tinland, Mohamed, Boyer and Auquier2015). The RAS consists of five domains: personal confidence and hope, willingness to ask for help, goal and success orientation, reliance on others, and no domination by symptoms. The participants responded using a five-point Likert scale (ranging from 1 ‘low’ to 5 ‘high’). We computed an index for each dimension and a total index by adding up the responses, with a higher index indicating better recovery (range: 0–100).
We defined housing stability as the number of days in an independent house or flat, and determined it using a residential timeline follow-back calendar. We assessed inpatient days and emergency department visits using a health service questionnaire, and we used a calendar to help the participant recall medical events. We also emphasised the confidentiality of sensitive items. We evaluated subjective QoL using the S-QoL 18 (Boyer et al., Reference Boyer, Simeoni, Loundou, D'Amato, Reine, Lancon and Auquier2010; Girard et al., Reference Girard, Tinland, Mohamed, Boyer and Auquier2015), a validated self-reporting tool for homeless subjects with mental disorders, including eight dimensions, with higher values implying better QoL. We used a generic QoL questionnaire to assess perceived physical and mental QoL using the Medical Outcomes Study 36-item Short Form Health Survey (SF-36) (Leplège et al., Reference Leplège, Mesbah and Marquis1995). Two composite scores were calculated – the physical composite score and the mental composite score (MCS) – with higher values indicating better health status. We evaluated mental health symptoms during the previous month via the Modified Colorado Symptom Index (MCSI) (Conrad et al., Reference Conrad, Yagelka, Matters, Rich, Williams and Buchanan2001), with higher scores indicating more self-symptoms.
We measured alcohol dependence using the specific AUDIT scale (Alcohol Use Disorders Identification Test) (Babor et al., Reference Babor, Dolinsky, Meyer, Hesselbrock, Hofmann and Tennen1992), which ranges from 0 to 38; a score of 12 or more denotes alcohol dependence. We evaluated dependence on psychoactive substances using section K of the Mini International Neuropsychiatric Interview (MINI) (Sheehan et al., Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs, Weiller, Hergueta, Baker and Dunbar1998). We only assessed the last two outcomes every 12 months (at baseline, M12, M24, M36 and M48).
Statistical methods
We performed a descriptive analysis of the study sample. Quantitative variables are expressed as the means and standard deviations; categorical variables are expressed as numbers and proportions. We conducted a comparative analysis of the two groups at inclusion using χ 2 or Fisher's exact tests for categorical variables, and Student's or Wilcoxon tests for quantitative variables, depending on the conditions of application. We carried out analyses adapted to longitudinal data using all available data from M0 to M48. We used linear mixed-effects models and generalised linear mixed-effects models to take into account the variability linked to individuals and the cluster effect. We modelled the within-subject random effects for each participant to adjust standard errors for the non-independence of observations within participants (cluster parameter = ‘site’; n = 4) (McNeish and Stapleton, Reference McNeish and Stapleton2016; Austin and Leckie, Reference Austin and Leckie2018). We based the selection of explanatory variables on the previous results of the Un Chez Soi d'Abord programme, which highlighted potential confounding factors (Tinland et al., Reference Tinland, Loubiere, Boucekine, Boyer, Fond, Girard and Auquier2020). We adjusted all multivariate models for the following variables: group, time, site, gender, SCZ or BP disorder diagnosis, age when first homeless, and the interaction of the group with all these variables (group × time, group × site, group × gender, group × diagnosis and group × age when first homeless). Time was represented by the function ln(t + 1), where t was the time from baseline. We only presented the results of the ‘group × time’ interaction in the form of β coefficients associated with their 95% confidence intervals and the p-value of the interaction. The β coefficient reflects the effect size (i.e. the difference between the slope of the HF group and the TAU group); if statistically significant, the interaction implied that the trajectory of improvement over time was better with HF than with TAU. We carried out a false discovery rate correction of the p-values for the subdimensions of the RAS and S-QoL scales to take into account the increased risk of error linked to the multiplicity of tests carried out (Benjamini and Hochberg, Reference Benjamini and Hochberg1995). We performed descriptive analysis using SPSS 12 for Windows (SPSS Inc., IBM, NY, USA). We implemented imputation models using MICE via chained equations and mitools R packages (RStudio, R version 3.6.0, Inc., Massachusetts, USA). We employed linear mixed-effects models for continuous variables and generalised linear mixed-effects models for substance dependence using R studio (lmer function using broom.mixed, lmerTest and lme4 packages or glmer function with a binomial family).
Results
A total of 703 homeless people agreed to participate and were randomised: 353 were assigned to the HF group and 350 to the TAU group (Fig. 1). The overall sample comprised males (82.5%) of French nationality (85.3%), with a median age of 40. More than two-thirds of the participants suffered from schizophrenia. On average, the participants had spent 8.6 years (standard deviation: ±7.9) on the streets. They had addictive disorders, with 46.3% having substance dependence and 39.5% alcohol dependence. The mean RAS index was 63.5 (±15.7) at baseline in both groups. Most baseline characteristics were similar between the treatment groups (Table 1). A total of 255 (78%) HF participants answered the 24-month questionnaire compared to 197 (63%) TAU participants. At the end of the 2-year follow-up period, 55 and 45% of the HF and TAU participants who had responded to the M24 interview signed the consent form for the extension of the follow-up; among these, 98 (69%) and 88 (61%) completed the follow-up at 48 months, respectively. We compared characteristics at baseline between complete and incomplete cases at 48 months of follow-up, with significant differences found for site and study group (p < 0.05) (eTable 2 in the online Supplementary material).
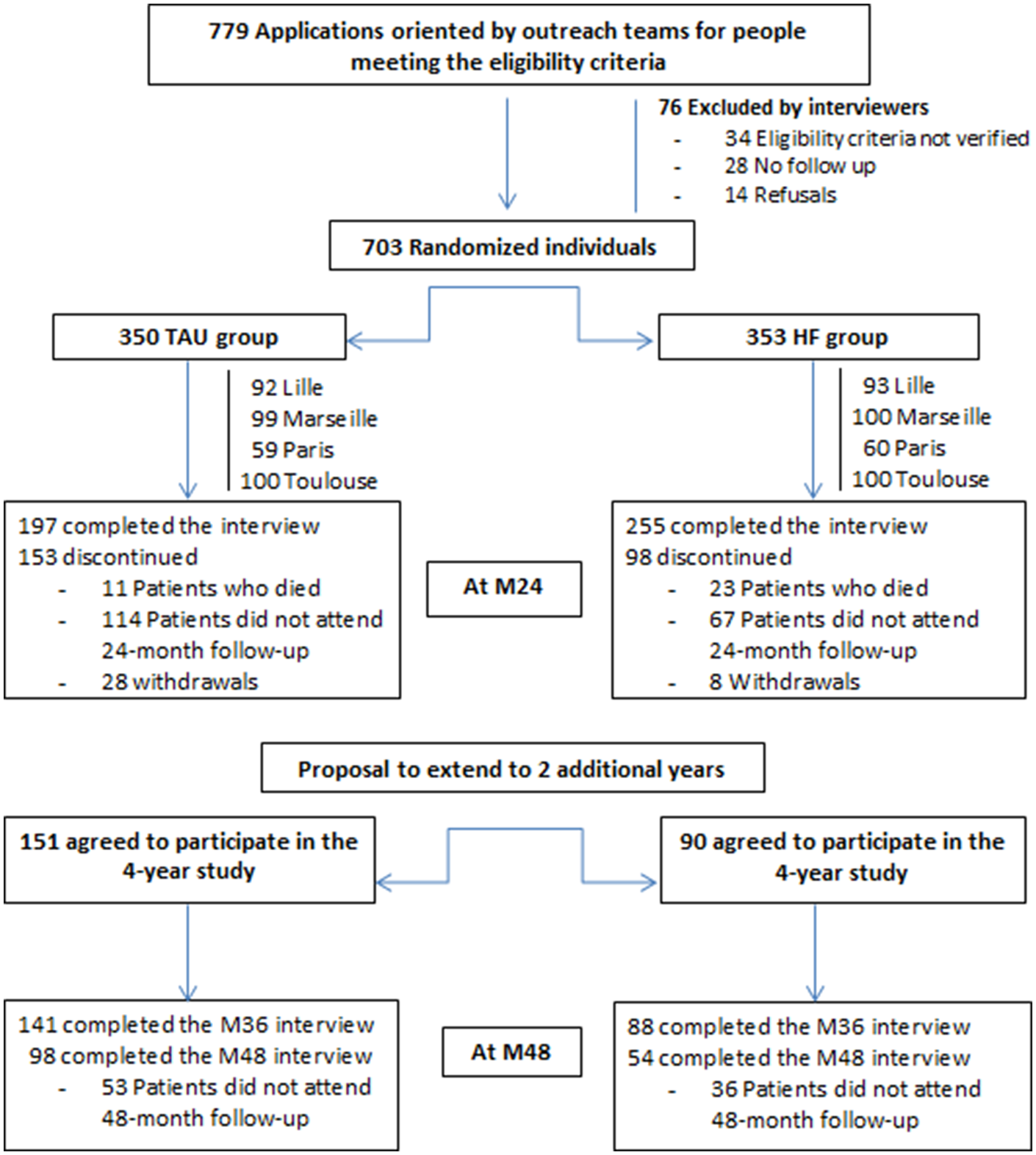
Fig. 1. Flow of participants in the Un Chez Soi d'Abord trial including the extension for an additional 2 years (in total 4 years). TAU, Treatment-As-Usual; HF, Housing First.
Table 1. Baseline characteristics of participants (N = 703)
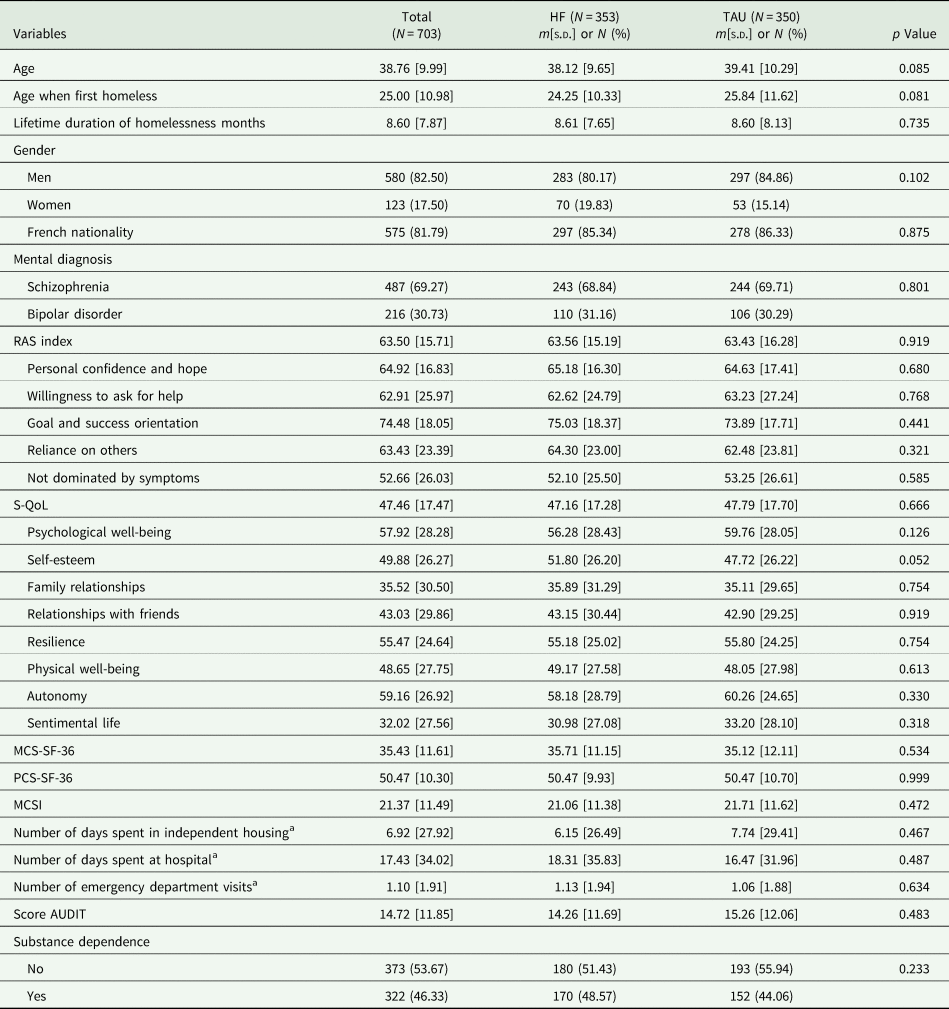
RAS, Recovery Assessment Scale; MCSI, Modified Colorado Symptom Index; SF-36, Medical Outcomes Study 36-item Short Form Health Survey; PCS, physical composite score; MCS, mental composite score; S-QoL, Subjective Quality of Life Questionnaire; AUDIT, Alcohol Use Disorders Identification Test.
a Over the last 6 months.
Table 2 shows the effect size of the group on the outcomes obtained from the linear and generalised mixed models. We found no statistically significant changes between the HF and TAU groups over time in the RAS index and its subscales, with both groups improving from baseline to 48 months (for details at each time point, see eTable 3 in the online Supplementary material).
Table 2. Effect size based on group × time interaction
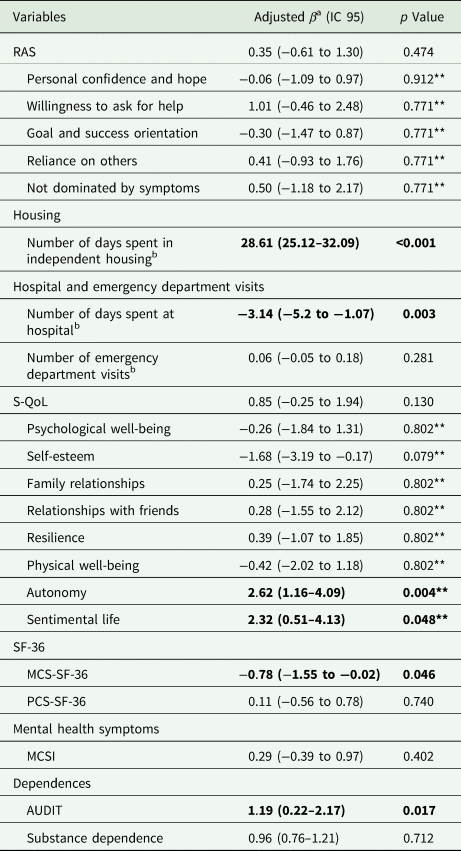
RAS, Recovery Assessment Scale; MCSI, Modified Colorado Symptom Index; SF-36, Medical Outcomes Study 36-item Short Form Health Survey; PCS, physical composite score; MCS, mental composite score; S-QoL, Subjective Quality of Life Questionnaire; AUDIT, Alcohol Use Disorders Identification Test. Values in bold indicate statistically significant results
a Models adjusted on gender, age, mental diagnosis, site, time and following interactions: gender × group, age × group, diagnostic × group, site × group.
b Over the last 6 months.
**p Value adjusted using FDR method (False Discovery Rate).
The dimensions of ‘autonomy’ and ‘sentimental life’ of the S-QoL scale improved in both groups, while the mean change from baseline to 48 months improved significantly more in the HF group than in the TAU group (adjusted β = 2.62 (1.16–4.09), p = 0.004 and adjusted β = 2.32 (0.51–4.13), p = 0.048, respectively). The HF group participants exhibited improved SF-36 MCS (−0.78 (−1.55 to −0.02), p = 0.046) over the 4-year follow-up. The number of days spent in independent housing increased more in the HF group than in the TAU group (28.6 (25.1–32.1), p < 0.001). The number of hospital days decreased more in the HF group than in the TAU group (−3.14 (−5.20 to −1.07), p = 0.003). We did not find any differences in the number of emergency department visits (0.06 (−0.05 to 0.18), p = 0.281). There was a greater increase in alcohol misuse over time in the HF group than in the TAU group (1.19 (0.22–2.17), p = 0.017). In contrast, we found no statistically significant differences between the groups for psychoactive substance dependence (1.13 (0.98–1.30), p = 0.087); more than one-quarter of participants were still diagnosed with substance dependency at 48 months (36 v. 22%, respectively).
Discussion
In homeless people with severe mental illness, the persistent improvements observed in housing stability, hospital service use, subjective QoL and the SF-36 MCS in our study demonstrate the sustainable clinical benefits beyond 2 years provided by housing subsidies with an ACT support team. These results are consistent with those reported in the two other large RCTs on the HF programme (Stefancic and Tsemberis, Reference Stefancic and Tsemberis2007; Stergiopoulos et al., Reference Stergiopoulos, Mejia-Lancheros, Nisenbaum, Wang, Lachaud, O'Campo and Hwang2019). Stefancic and Tsemberis noted that over the course of 4 years, the majority of HF users were able to maintain permanent and independent housing, while most participants in the control group still had not reached the endpoint of permanent, independent housing (Stefancic and Tsemberis, Reference Stefancic and Tsemberis2007). Stergiopoulos et al. found significantly more days spent in stable housing among HF participants than TAU participants at all time points over a 6-year period, while they observed no differences in general and disease-specific QoL or community functioning (Stergiopoulos et al., Reference Stergiopoulos, Mejia-Lancheros, Nisenbaum, Wang, Lachaud, O'Campo and Hwang2019).
Similar to Aubry et al.'s review (Aubry et al., Reference Aubry, Bloch, Brcic, Saad, Magwood, Abdalla, Alkhateeb, Xie, Mathew, Hannigan, Costello, Thavorn, Stergiopoulos, Tugwell and Pottie2020), we found no measurable effect on psychiatric symptom severity between the HF and TAU groups. Thus, the HF model at 2 years (Tinland et al., Reference Tinland, Loubiere, Boucekine, Boyer, Fond, Girard and Auquier2020) or over 4 years did not show a significant impact on clinical recovery among users, assessed in terms of a reduction in mental symptoms. Considering other recovery dimensions besides the clinical one, our results indicated no significant improvement in RAS scores (personal recovery) alongside the 4 years of follow-up in the HF group, with the HF group improving more rapidly, although the gap narrowed over time, with continued improvements in the TAU group. These non-significant findings need to be qualified by significant results for other outcomes. For example, the significant improvements in autonomy and sentimental life in the HF group denote improved recovery, as these outcomes are the aspects of the recovery process. Similarly, the RAS instrument did not perfectly cover the aspect of housing stability, which is another form of the recovery process. Although researchers consider it to be the best instrument to capture the non-clinical dimensions of recovery in people with mental illness (Shanks et al., Reference Shanks, Williams, Leamy, Bird, Le Boutillier and Slade2013; Salzer and Brusilovski, Reference Salzer and Brusilovskiy2014; van Weeghel et al., Reference van Weeghel, van Zelst, Boertien and Hasson-Ohayon2019), a unique instrument such as the RAS scale cannot be exhaustive in capturing all dimensions of the complex recovery process. We can see at least three reasons for observing no differences in the RAS domains. First, our study includes individuals with concentrated disadvantages associated with health-risk behaviours, including substance use and alcohol consumption, still prevalent after 4 years. In such situations, recovery dimensions such as personal confidence and hope, the willingness to ask for help, goal and success orientation, reliance on others, and no domination by symptoms may be very difficult to achieve, according to previous qualitative research (Henwood, Reference Henwood2015; Rhenter et al., Reference Rhenter, Moreau, Laval, Mantovani, Albisson, Suderie, Boucekine, Tinland, Loubiere, Greacen, Auquier and Girard2018a; Pahwa et al., Reference Pahwa, Smith, Yuan and Padgett2019). Second, Salzer and Brusilovskiy pointed out that experimental studies that failed to show statistically significant changes over time in recovery outcomes may have recruited people with relatively high recovery scores at baseline (Salzer and Brusilovskiy, Reference Salzer and Brusilovskiy2014). The mean RAS score (range: 24–120) was 81.5 (±17.1) at baseline in our two groups, so we wonder whether this score was too high to show a difference in the RAS outcomes between the two groups. Last, a re-evaluation of expectations is also likely over a 4-year period as living conditions change. This effect, called the ‘response shift’, is well known in QoL research (Schwartz et al., Reference Schwartz, Andresen, Nosek and Rahn2007; Boucekine et al., Reference Boucekine, Boyer, Baumstarck, Millier, Ghattas, Auquier and Toumi2015). Conventionally, three concepts of response shift have been distinguished: (i) changes in internal standards of measurement (recalibration); (ii) changes in the priority (i.e. importance) of the component domains of the target construct (re-prioritisation); and (iii) a redefinition of the target construct (re-conceptualisation). In practice, this reflects an adaptive process. The existence of a response shift would be relevant, as it would point to the capability to adapt (i.e. an expectation of personal recovery). A further investigation would involve measuring the response shift in our study to see if any of its components are present, indicating HF users' adaptation, thus demonstrating the HF model's effects on personal recovery.
However, the positive results in terms of housing stability, autonomy, relational environment, mental functioning and hospital use are counterbalanced by one main point: the increase in alcohol dependence in the HF group in comparison with the TAU group. This mixed finding on alcohol misuse is in line with several studies that have revealed that HF users continued to consume alcohol, and reported similar or increased alcohol use disorders after 1–2 years compared to TAU participants (Edens et al., Reference Edens, Mares, Tsai and Rosenheck2011; Padgett et al., Reference Padgett, Stanhope, Henwood and Stefancic2011; Collins et al., Reference Collins, Malone and Clifasefi2013; Asana et al., Reference Asana, Ayvaci, Pollio, Hong and North2018). For example, Collins et al. compared alcohol consumers with non-consumers in a large non-randomised controlled trial and found that active alcohol consumers were more likely to stay in the housing project than non-consumers (Collins et al., Reference Collins, Malone and Clifasefi2013). One may explain these findings by the role played by the recovery process in connection with the ACT team and its harm reduction approach. Thanks to recovery-oriented support, HF users can more readily acknowledge their drinking difficulties (i.e. an acquired capability in the sense of the overall recovery process). In contrast, TAU users are likely to hide their alcohol use because of an abstinence approach within standard services. While we cannot totally rule out that the participants in the HF group have a real problem with alcohol, the fact that HF users can speak freely about their addiction could partially explain the differences between the two groups. Our results, in relation to the previous findings cited in the literature, suggest that high housing outcomes are strongly anticipated with the HF programme, even among people with severe alcohol disorders. Despite this, public authorities should be recommended to strengthen support and counselling within the HF programme regarding alcohol issues and concomitant risks (drugs and related comorbidities) (Collins et al., Reference Collins, Malone and Clifasefi2013).
This study has some limitations. First, HF is a complex intervention that contains several interacting components, and our design does not allow for the examination of the intervention's individual elements. Second, blinding was not possible for the interviewers or participants (Hawthorne effect) (McCambridge et al., Reference McCambridge, Witton and Elbourne2014). In particular, sociologists observed that participants in the TAU group had a sense of unfairness in being attributed to the control group and overachievers (Rhenter et al., Reference Rhenter, Tinland, Grard, Laval, Mantovani, Moreau, Vidaud, Greacen, Auquier and Girard2018b). Third, our study was based on interviews with self-reported outcomes. However, to defend against this limitation, the measure of self-reported health care use is reliable in homeless people with mental illness (Bonin et al., Reference Bonin, Fournier, Blais, Perreault and White2007; Hwang et al., Reference Hwang, Chambers and Katic2016; Somers et al., Reference Somers, Moniruzzaman, Currie, Rezansoff, Russolillo and Parpouchi2016), and we deliberately chose tools measuring users' subjective perspectives as indicators. Finally, the persistence of non-significant results must be interpreted in light of the population studied and the duration of follow-up, which is probably still too brief to apprehend quantifiable changes in patients with schizophrenic or bipolar disorder. Considering the recovery process, this follow-up should ideally be continued over a period of 10 years, but this remains complicated in the context of effective dissemination of the model throughout the country. We cannot overlook the fact that the RAS tool does not in the end capture the entire recovery process that takes place in this population. Nonetheless, the positive and convergent effects observed in specific dimensions of recovery (the willingness to ask for help, reliance on others) in the first year and continued improvement in the QoL subscales (i.e. autonomy, sentimental life) at 4 years suggest that the HF programme enhances the relational environment, thereby enabling the recovery process of severely mentally ill homeless people.
Our findings highlight the persistence of better outcomes with the HF intervention compared to standard care in terms of housing stability, autonomy and the use of hospital services. The recommendations that can be drawn from our findings are that HF providers should promote all services designed to keep participants in housing, and further develop services to successfully manage their behavioural health, such as alcohol dependence, in the long run.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796022000026.
Data
Not all the data are freely accessible because no informed consent was given by the participants for open data sharing, but we can provide the data used in this study to researchers who want to use them, following approval by the ethics committee of the Aix Marseille University.
Acknowledgements
The authors would like to thank the hundreds of people who agreed to take part in the survey. We are also indebted to the field research team members. Specifically, we wish to thank: El-had Mohammed, Amandine Albisson, Pierre Allenou, Karine Baumstarck, Emma Beetlestone, Julien Billard, Philippe Birmes, Raphaël Bouloudnine, Emmanuelle Bourlier, Thomas Bosetti, Jean-Marc Colucci, Thierry Danel, Jacques Debieve, Achille Djiena, David Flahaut, Cécile Fortanier, Géraldine Guétière, Pascale Hérédia-Rodier, Emmanuelle Jouet, Patrick Le Cardinal, Jean-Marc Legagneux, Emilie Labeyrie, Jean Mantovani, Alain Mercuel, Delphine Moreau, Jean Naudin, Fanny Olive, Stefano Rampa, Elodie Requier, Jean-Luc Roelandt, Eglantine Simonnet, Guillaume Suderie, Aurélien Troisoeufs, Pierre-Pascal Vandini, René Wulfman and Thomas Gesmond. We thank Justine Buand for the English grammar correction. Special thanks go to the Dihal: Délégation interministérielle à l'habitation et au logement and Dr Pascale Estecahandy. In addition, we would like to thank members of the Canadian At Home/Chez Soi team for their help and advice in developing the French Housing First programme: Paula Goering, Jean-Pierre Bonin, Cécile Leclerc, Eric Latimer and Sonia Coté, as well as Tim Aubry. The authors alone are responsible for the findings.
Financial support
This work was supported by the DGOS, Programme Hospitalier de Recherche Clinique National (PHRC; DGOS/PF4/2010/24.02); DGOS, Programme de Recherche sur la Performance du Système de santé (PREPS, grant number 14-0065); Janssen Pharmaceutical Company; and the Fondation de France.
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The local ethics committee (Comité de Protection des Personnes Sud-Méditerranée V, France: trial number 11.050) and the French Drug and Device Regulation Agency (trial number 2011-A00668-33) approved this study.





