In December 2019, several cases of pneumonia of unknown cause were reported in Wuhan, China that were later recognized as a novel coronavirus infection, named coronavirus disease 2019 (COVID-19) by the World Health Organization (WHO). Reference Huang, Wang and Li1 COVID-19 has been included in the laws of the People’s Republic of China in the prevention and treatment of infectious diseases as a class B infectious disease. All provinces and cities in China have taken first-level public health emergency responses to contain the transmission of the disease and protect vulnerable populations. The epidemic has spread across China as well as into 213 countries and territories. 2 The COVID-19’s socioeconomic impacts have already far exceeded those of severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS), and the pandemic has become a worldwide major public health concern. As of June 21, 2020, the global number of confirmed cases of COVID-19 exceeded 9 million, leading to over 470 thousand of fatalities. 2 We attempted to describe the clinical characteristics of fatalities in patients with COVID-19, which may inform the clinical management of patients with severe COVID-19.
METHODS
This was an Internet-based data intelligence study. We constituted a cohort of COVID-19 deaths through retrieving the clinical information on COVID-19 fatalities from nonduplicating incidental reports in Chinese provincial and metropolitan city Health Commission and other governmental official websites between January 23 and March 10, 2020. The reported clinical characteristics included the patient’s age, sex, initial onset symptoms, pre-existing chronic diseases, direct cause of death, date of admission, date of diagnosis, and date of death. The study cohort included 100 cases of COVID-19 fatalities. The study was approved by the research ethics committee of Henan University. Informed consent was waived, because the study was based on publicly available anonymized incidental fatality reports.
Statistical Analysis
SPSS (version 22.0) software was used for statistical analysis. Mean ± standard deviations (SD) and median (inter-quartile range) were presented for continuous variables, while frequency and percentage were presented for categorical variables.
Patient and Public Involvement
Patients were not involved in the study, which is based on anonymized incidental COVID-19 fatality reports from governmental websites.
RESULTS
Approximately 6 of 10 COVID-19 fatalities (64.0%) were males (Table 1). The average age was 70.7 ± 13.5 y (median: 72.5 y), and approximately 8 of 10 patients (84.0%) were over 60 y of age. The mean duration from admission to diagnosis was 2.2 ± 2.8 d (median: 1). The average duration from the diagnosis to death was 9.9 ± 6.5 d (median: 9 d).
TABLE 1 Clinical Characteristics of COVID-19 Fatalities (n = 100)
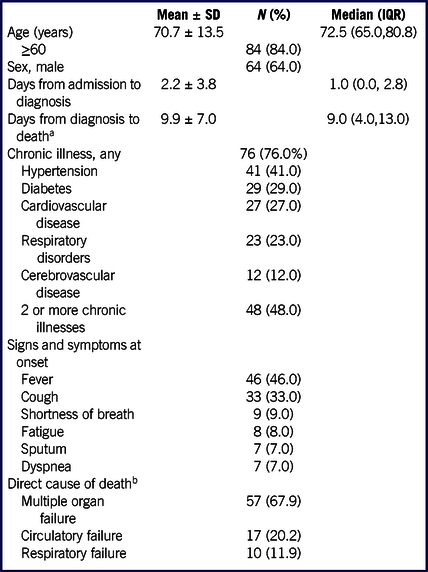
a A total of 12 cases were missing data on the time from diagnosis to death.
b A total of 16 cases were missing data on direct cause of death.
Approximately 3 of 4 fatal COVID-19 cases (76.0%) had 1 or more pre-existing chronic illnesses. The prevalence rates were 41.0% for hypertension, 29% for diabetes, 27.0% for coronary heart disease, 23% for respiratory disorders, 12% for cerebrovascular disease, 3% for cancers, 5% for abnormal renal function, and 2.0% for Parkinson’s disease. Approximately half of patients (48%) had 2 or more chronic diseases.
Fever (46.0%), cough (33.0%), shortness of breath (9.0%), fatigue and weakness (8.0%), sputum (7.0%), and dyspnea (7.0%) were the common symptoms at onset, whereas palpitations and diarrhea were less frequent. Among the 100 COVID-19 fatalities, 16 cases were missing data on direct cause of death. Of the 84 COVID-19 cases with known direct cause of death, the top 3 common direct causes of death were multiple organ failure (67.9%), circulatory failure (20.2%), and respiratory failure (11.9%), and were similar (P = 0.50) for males and females: multiple organ failure (64.8% vs 73.3%, respectively), circulatory failure (24.1% vs 13.4%, respectively), and respiratory failure (11.1% vs 13.3%, respectively).
DISCUSSION
In this Internet-based data intelligence study, we observed that the majority of COVID-19 deaths were elderly (approximately 8 of 10) and males (6 of 10), and most fatalities (3 of 4) occurred in patients with chronic illnesses. The findings were consistent with a recent report in a hospital-based study, Reference Chen, Wu and Chen3 and with the WHO report on COVID-19 in China, 4 and demonstrate the usefulness of an Internet-based data intelligence study. Previous studies have not clarified the direct causes of death. Our data indicate that the most common direct cause of death is multiple organ failure (approximately 2 of 3). The initial onset symptoms are not so much saliently worrisome, but the median duration from diagnosis to death was only 9 d, indicating that the disease can worsen rapidly, costing life.
The function of innate immunity and neutrophil function may degrade with aging, exposing the elderly to the more deleterious impact of the new coronavirus infection. Similar to SARS and MERS, COVID-19 presents a clear male sex bias. Reference Channappanavar, Fett and Mack5 Compared with males, the immune response in females may be more vigorous with higher antibody levels following exposure to an infectious agent; Reference Moxley, Posthuma and Carlson6 thus, females may be less vulnerable to the deleterious consequence of COVID-19 infection. It has been speculated that women’s lower susceptibility to viral infections may be related to genetic factors associated with the X chromosome and sex hormones. Another possible explanation for the higher incidence and more male COVID-19 fatalities may be due to that males are likely to spend more time outdoors, increasing the chances of exposure to the virus.
Consistent with previous reports, most (approximately 3 of 4) fatalities occurred in patients with chronic illnesses. Reference Chen, Wu and Chen3,Reference Onder, Rezza and Brusaferro7 The top 4 were hypertension (41.0%), diabetes (29.0%), coronary heart disease (27.0%), and respiratory disorders (23.0%). Previous studies indicate that COVID-19 shares the same receptor with SARS-COV, and the angiotensin-converting enzyme-2 (ACE2) sensitive cell surface receptors mediate the entry of the virus into the target cells. Reference Lu, Zhao and Li8 ACE2, the functional receptor of SARS-COV, is expressed in the islet, through which the virus may invade and destroy the pancreatic islet cells, thus may aggravate diabetes and accelerate the disease progression. The immune system plays a crucial role when the body is confronted with viruses or bacteria. For patients with diabetes, especially those with poor blood glucose control, long-term exposure to hyperglycemia may lead to decreased immune function. Other chronic illnesses may also compromise the patient’s immune defense system leading to severe consequences.
Multiple organ failure, respiratory failure, and circulatory failure were the main direct causes of deaths. Similar to MERS-CoV, Reference Zumla, Hui and Perlman9 multiple organ failure appears to be a common direct cause of death in COVID-19 fatalities. The COVID-19 infection may lead to increased blood capillary permeability of the lungs, Reference Ackermann, Verleden and Kuehnel10 aggravating inflammation and apoptosis, with lung injuries leading to respiratory distress syndrome. The virus may set off an immune inflammatory response storm, causing tissue damages in multiple organs leading to multiple organ failure.
This study has some limitations. First, we did not have the laboratory data in this Internet reports-based study. The reported clinical characteristics are relatively limited in Internet reports. It is unclear whether there is a selection bias in Internet reports of COVID-19 fatalities compared with those fatalities in the general population. However, our data on age and sex distributions of COVID-19 deaths are consistent with the recent report on 113 deaths in a single large hospital-based study in Wuhan, China. Reference Chen, Wu and Chen3
In conclusion, COVID-19 deaths are mainly elderly and patients with chronic diseases, especially cardiovascular disorders and diabetes. Multiple organ failure is the most common direct cause of death. Our findings may inform clinical health-care professionals in better management of severe COVID-19 patients in fighting the emerging pandemic.
Acknowledgments
We acknowledge Zhong-Xiang Wang (School of Nursing and Health, Zhengzhou University) for his helpful suggestions and spiritual support.
Author Contributions
All authors contributed to the development of the conceptual framework of this study. P.X.W. and Z.C.L. initiated the study, supervised the collection of research data. Y.J.S., Y.J.F., and C.J. collected the data. B.L. contributed to data interpretation. Y.J.S. analyzed the data and drafted the manuscript. All authors contributed to critical revisions of the study, and approved the final version for publication.
Funding Statement
This work was supported by research grants from the Foshan COVID-19 Emergency Technology Project (2020001000376) and the Canadian Institutes of Health Research (CIHR grant # 155955).
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethics Statement
The study was approved by the research ethics committee of Henan University (HUSOM 2020-0 11), and informed consent was waivered because the study was based on publicly available anonymized incidental fatality reports.
Data Availability Statement
The study data are available from the corresponding author upon reasonable request.





