Introduction
Emotional dysregulation, which is present in 3% to 20% of children and youth, is commonly defined as the inability to recognize, evaluate, regulate, and manage the intensity and quality of emotions (i.e., fear, anger, and sadness) in a personal and socially acceptable way.Reference Paulus, Ohmann, Mohler, Plener and Popow 1 -Reference Brotman, Schmajuk and Rich 3 Studies have described emotional dysregulation as a transdiagnostic construct shared across various psychiatric disorders, including attention deficit hyperactivity disorder, schizophrenia, bipolar disorder, major depressive disorder, and trauma-related disorders.Reference Paulus, Ohmann, Mohler, Plener and Popow 1 -Reference Brotman, Schmajuk and Rich 3 Deficits in emotional regulation are associated with the altered functioning in the rostral and subgenual regions of the anterior cingulate cortex (ACC), the orbitofrontal and the dorsomedial prefrontal cortex (PFC), and regions involved in executive and attentional control (i.e., the dorsal ACC, ventrolateral PFC, and dorsolateral PFC) and reward functioning (i.e., amygdala and nuclear accumbens), which also contribute to the pathomechanisms of schizophrenia, bipolar disorder, and major depressive disorder.Reference Paulus, Ohmann, Mohler, Plener and Popow 1 , Reference Portugal, Rosa and Rao 4
A recent study of 448 children and adolescents with schizophrenia found that approximately 20% of young patients were coaggregated with a spectrum of emotional dysregulation conditions and revealed that higher emotional dysregulation symptoms were related to an increased risk of acute inpatient and emergency service utilization.Reference Jerrell, McIntyre and Deroche 5 De Loore et al.Reference De Loore, Gunther and Drukker 6 suggested that emotional dysregulation moderated the severity of schizophrenia-associated positive symptoms, especially auditory hallucination Further evidence has indicated that the spectrum of affective mood disorders, including bipolar disorder, major depressive disorder, dysthymic disorder, and cyclothymic disorder, may be a disorder of emotional dysregulation.Reference Brotman, Schmajuk and Rich 3 , Reference Townsend and Altshuler 7 , Reference Leibenluft 8 Mitchell et al.Reference Mitchell, Timmins, Collins, Scavone, Iskric and Goldstein 9 reported that approximately 25% of adolescents with bipolar disorder (I: N = 30, II: N = 46, and not otherwise specified: N = 40) exhibited severe emotional dysregulation symptoms, which were not associated with subtypes of bipolar disorder They also determined a positive relationship of parent-reported family conflict and greater functional impairment with emotional dysregulation.Reference Mitchell, Timmins, Collins, Scavone, Iskric and Goldstein 9 Brotman et al.Reference Brotman, Schmajuk and Rich 3 demonstrated that adolescents with severe emotional dysregulation were more likely to be diagnosed with a depressive disorder (odds ratio [OR]: 7.2, confidence interval [CI]: 1.3–38.8) than those without However, no head-to-head comparative study assessed the emotional dysregulation symptoms among adolescents with first-episode schizophrenia, bipolar disorder, and major depressive disorder.
The role of appetite hormones, namely insulin, leptin, adiponectin, and ghrelin in the pathomechanisms of emotional dysregulation, has remained unclear.Reference Gold 10 Previous studies have reported that insulin resistance and glucose intolerance states may acutely emerge in anticipatory stress, indicating elevated glucose levels in the brain that establish premonitory and proinflammatory states against a subsequent threat.Reference Gold 10 -Reference Zarouna, Wozniak and Papachristou 13 Stress is related to emotional dysregulation and is commonly noted in patients with severe mental disorders,Reference Davis, Holmes, Pietrzak and Esterlis 11 -Reference Zarouna, Wozniak and Papachristou 13 which may require clinicians and researchers to clarify the connections between appetite hormones, emotional dysregulation, and severe mental disorders. For example, a 9-year follow-up study found that adolescents with greater leptin concentrations and abdominal adiposity had the easier emergence of depressive symptoms during the follow-up.Reference Milaneschi, Sutin and Terracciano 14 Hafner et al.Reference Hafner, Zierer and Emeny 15 reported a positive association between social isolation, which often occurs in schizophrenia and depressive states, and leptin levels. Other studies have explored the regulatory role of ghrelin in the reward system, particularly in the amygdala, which is significantly associated with emotional regulation.Reference Carlini, Varas, Cragnolini, Schioth, Scimonelli and de Barioglio 16
In this study, we compared the emotional dysregulation symptoms and levels of appetite hormones between adolescents with first-episode severe mental disorder (schizophrenia, bipolar disorder, and major depressive disorder) and with a control group. To avoid the confounding effect of obesity on the aforementioned associations, we only enrolled nonobese adolescents. We hypothesized that adolescents with first-episode severe mental disorder were more likely to have emotional dysregulation symptoms and appetite hormone dysregulation compared with the control group. In addition, we hypothesized a positive relationship between emotional and appetite hormone dysregulation among adolescents with first-episode severe mental disorder.
Methods
Participants
Adolescents aged between 12 and 19 years who met the criteria specified in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) for schizophrenia, bipolar disorder, or major depressive disorder were enrolled in this study. They had a first episode of illness, and were in a relatively stable condition (Clinical Global Impression—Severity scale ≤4) to compliantly complete the study assessment. Patients with intellectual disability, neurodevelopmental disorder, substance/alcohol-use disorder, eating disorder, organic mental disorder, obesity (body mass index, BMI >30; BMI percentile >95th percentile), pregnancy or breastfeeding, severe autoimmune/immune diseases, stroke, epilepsy, and unstable physical illnesses were excluded. We also enrolled age-, sex- and BMI-matched healthy controls without any of the mentioned physical conditions or psychiatric disorders based on the Mini International Neuropsychiatric Interview Kid. Demographic characteristics, including age, sex, BMI, and BMI percentile, were recorded and clinical assessments, including 17-item Hamilton Depression Rating Scale (HDRS),Reference Hamilton 17 Young Mania Rating Scale (YMRS),Reference Biggs, Ziegler and Meyer 18 and Positive and Negative Syndrome Scale (PANSS),Reference Andreasen and Olsen 19 were examined. The Institutional Review Board of the Taipei Veterans General Hospital approved our study, and it was performed in accordance with the Declaration of Helsinki. All patients and their parents provided written informed consent prior to their inclusion in the study.
Measurement of appetite hormones
Fasting serum samples were collected between 9 and 12 AM in serum separator tubes, clotted for 30 min, and stored at −80 °C until use. The appetite hormones, including leptin, ghrelin, insulin, adiponectin, were examined. Ghrelin was measured using a radioimmunoassay (RIA) kit (Peninsula Laboratories, Inc., San Carlos, CA, USA). Insulin concentrations were analyzed using an RIA kit (Coat-A Count Insulin; Diagnostic Product Corporation, Los Angeles, CA, USA). Serum adiponectin level was measured using a quantitative Human Adiponectin ELISA Kit (B-Bridge International, Inc., Mountain View, CA, USA). All assays were performed according to the vendor’s instructions. The final absorbance of each sample of the mixture was measured and analyzed at 450 nm using an ELISA plate reader with Bio-Tek Power Wave Xs and Bio-Tek’s KC junior software (Winooski, VT, USA). The standard range was considered as specified in the vendor’s instructions. A linear regression R-square value of approximately 0.95 was considered a reliable standard curve.
Assessment of emotional regulation
Child Behavior Checklist (CBCL) is a checklist that parents complete to detect emotional and behavioral problems in children and adolescents, and is commonly used in previous studies.Reference Hua, Chen and Chen 20 , Reference Biederman, DiSalvo and Vaudreuil 21 The sum of subscale scores for anxious/depressed, aggressive behavior, and attention problems of CBCL was used as the clinical marker of emotional regulation (Dysregulation Profile, CBCL-DP).Reference Biederman, Spencer and Petty 22
Statistical analysis
For between-group comparisons, the analysis of variance (F-test) was used for continuous variables and Pearson’s test was used for categorical variables. Kolmogorov–Smirnov tests indicated that appetite hormones were not normally distributed; they were then transformed using a log. Generalized linear models (GLMs) with the adjustment of age, sex, BMI or BMI percentile, and scores of HDRS, YMRS, and PANSS were used to compare levels of appetite hormones, including leptin, ghrelin, insulin, adiponectin, and CBCL-DP scores between groups. GLMs with the adjustment of group, age, sex, and scores of HDRS, YMRS, and PANSS were performed to examine the associations among levels of appetite hormones, BMI or BMI percentile, and CBCL-DP scores. A two-tailed P value of less than.05 was considered statistically significant. All data processing and statistical analyses were performed using the SPSS version 17 software (SPSS Inc.).
Results
In all, 22 adolescents with schizophrenia, 31 with bipolar disorder, 33 with major depressive disorder; and 41 age-, sex- and BMI-matched healthy controls were enrolled in this study (Table 1). Patients with schizophrenia had the highest scores of PANSS (P < .001), those with bipolar disorder had the highest scores of YMRS (P < .001), and those with major depressive disorder had the highest scores of HDRS (P < .001) compared with the control group (Table 1). Before and after the adjustment, CBCL-DP scores did not differ between patients with schizophrenia, bipolar disorder, and major depressive disorder, and were higher in three patient groups (all P < .05) than in the control group (Table 1 and Figure 1).
Table 1. Demographic Characteristics, Appetite Hormone Levels, and Clinical Symptoms between Groups

Abbreviations: BD, bipolar disorder; BMI, body mass index; CBCL, child behavior checklist; CGI-S, clinical global impression—severity scale; DP, dysregulation profile; HC, healthy control; HDRS, 17-item Hamilton depression rating scale; MDD, major depressive disorder; PANSS, positive and negative syndrome scale; SCZ, schizophrenia; SD, standard deviation; YMRS, Young Mania rating scale.

Figure 1. Estimated marginal means of CBCL-DP scores between groups. (a) BMI adjusted, (b) BMI percentile adjusted. BD, bipolar disorder; BMI, body mass index; CBCL, child behavior checklist; DP, dysregulation profile; HC, healthy control; HDRS, 17-item Hamilton depression rating scale; MDD, major depressive disorder; PANSS, positive and negative syndrome scale; SCZ, schizophrenia; YMRS, Young Mania rating scale.
GLMs with the adjustment of age, sex, BMI or BMI percentile, and scores of HDRS, YMRS, and PANSS showed that patients with bipolar disorder had higher log-transformed levels of insulin (P = .029 and .021) and lower log-transformed levels of leptin (P = .018 and.014) compared with the control group (Figure 2). In addition, GLMs with the adjustment of group, age, sex, and scores of HDRS, YMRS, and PANSS found the positive association between BMI and CBCL-DP scores (P < .05), but no relationship between appetite hormone levels and CBCL-DP scores (Table 2). Interestingly, GLMs with the adjustment of group, age, sex, and scores of HDRS, YMRS, and PANSS showed a positive association between log-transformed ghrelin levels (P = .028) and CBCL-DP scores (Table 2).
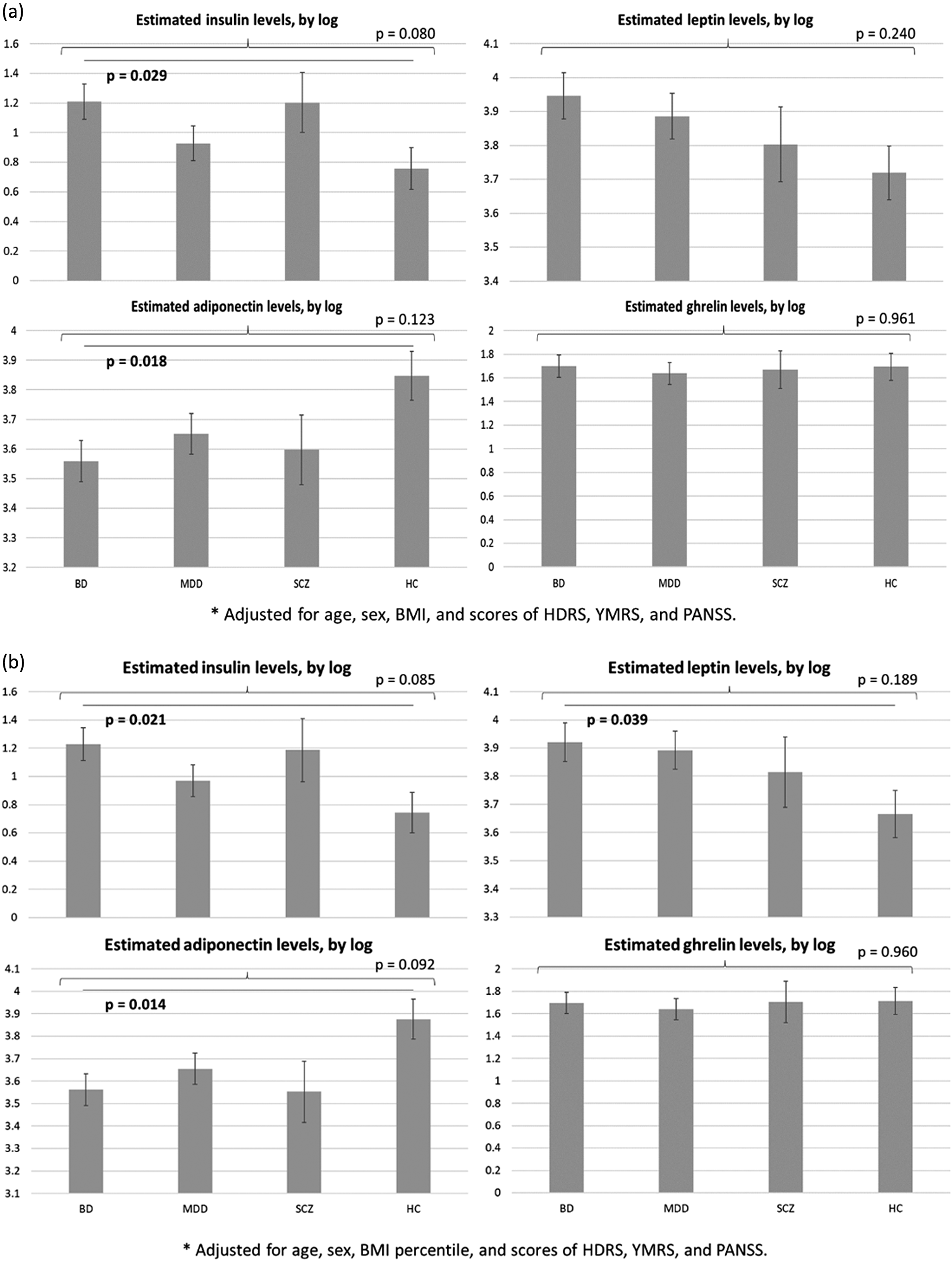
Figure 2. Estimated marginal means of appetite hormone levels between groups. (a) BMI adjusted, (b) BMI percentile adjusted. BD, bipolar disorder; BMI, body mass index; HC, healthy control; HDRS, 17-item Hamilton depression rating scale; MDD, major depressive disorder; PANSS, positive and negative syndrome scale; SCZ, schizophrenia; YMRS, Young Mania rating scale.
Table 2. GLMs with Adjustment of Group, Age, Sex, and Symptom Scores between BMI or BMI Percentile, Appetite Hormone Levels, and CBCL-DP Scores
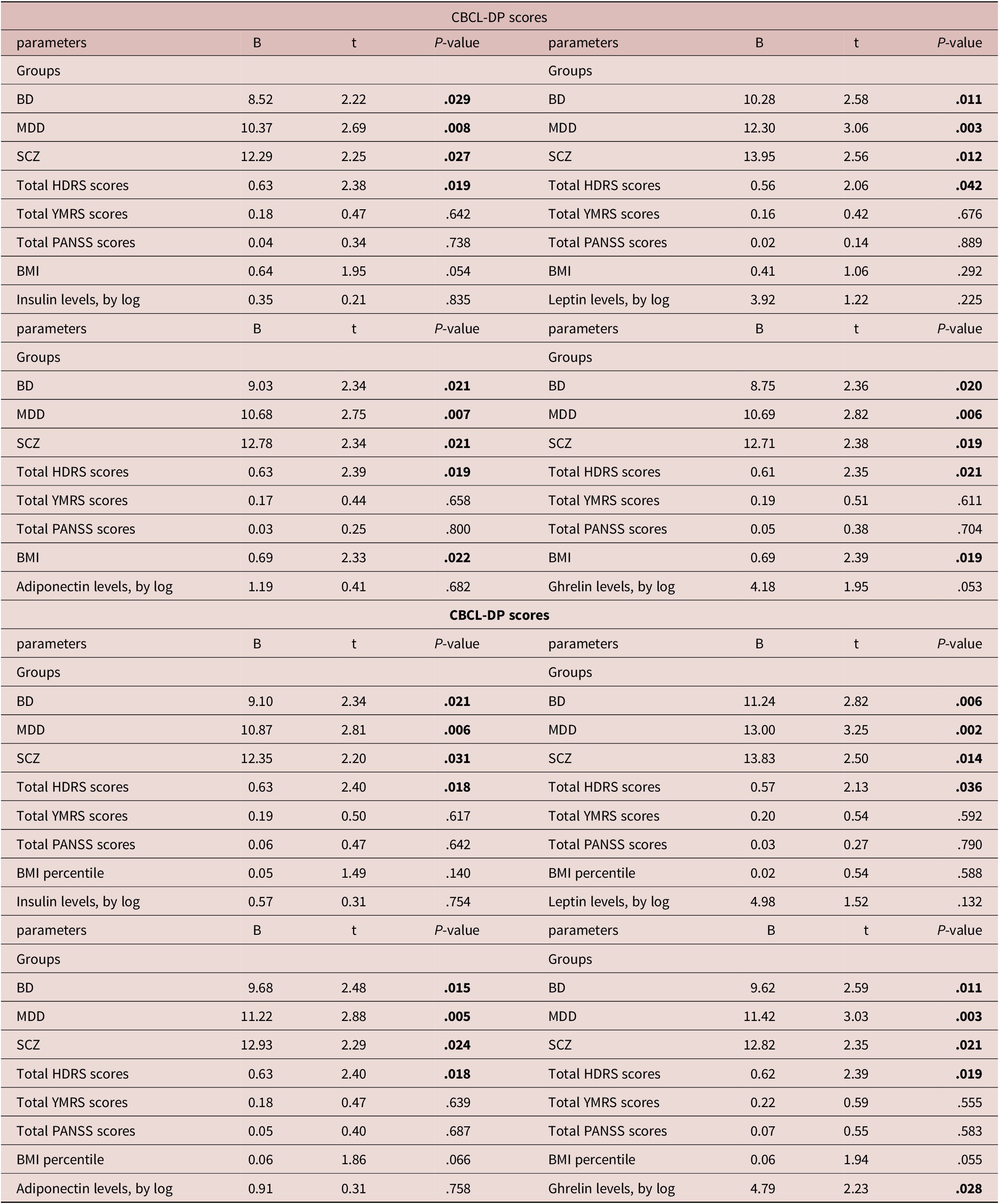
Abbreviations: BD, bipolar disorder; BMI, body mass index; CBCL, child behavior checklist; DP, dysregulation profile; HC, healthy control; HDRS, 17-item Hamilton depression rating scale; MDD, major depressive disorder; PANSS, positive and negative syndrome scale; SCZ, schizophrenia; YMRS, Young Mania rating scale.
Discussion
Our results partially supported the hypothesis that adolescents with first-episode schizophrenia, bipolar disorder, and major depressive disorder would exhibit greater emotional dysregulation symptoms than the control group. Adolescents with first-episode bipolar disorder reported higher levels of insulin and lower levels of adiponectin compared with the controls. Interestingly, we found the positive associations of BMI and ghrelin levels with emotional dysregulation symptoms, even though obese adolescents were excluded and clinical symptoms were controlled for in our study.
As mentioned, emotional dysregulation works as a transdiagnostic construct shared across schizophrenia, bipolar disorder, and major depressive disorder.Reference Paulus, Ohmann, Mohler, Plener and Popow 1 -Reference Brotman, Schmajuk and Rich 3 A recent study of 22 patients with schizophrenia and 31 patients with major depressive disorder demonstrated that patient groups exhibited significantly lower overall levels of emotional functioning, including perception and regulation, compared with healthy controls, based on the Self-Report Emotional Ability Scale.Reference Weiss, Deisenhammer, Fink, Marksteiner, Canazei and Papousek 23 Kring et al.Reference Kring and Elis 24 reported that patients with schizophrenia had difficulties anticipating emotional events and maintaining or appreciating their emotional experiences, which further resulted in emotional dysregulation Increasing evidence suggests that emotional dysregulation is an endophenotype of bipolar disorder.Reference Miola, Cattarinussi, Antiga, Caiolo, Solmi and Sambataro 25 A meta-analysis study of 858 patients with bipolar disorder and 285 healthy controls revealed that patients with bipolar disorder showed significantly higher total scores on the Difficulties in Emotion Regulation Scale and subscale scores, including impulse control and emotional clarity.Reference Miola, Cattarinussi, Antiga, Caiolo, Solmi and Sambataro 25 Carruthers et al.Reference Carruthers, Rossell, Murray, Karantonis, Furlong and Van Rheenen 26 indicated that emotional dysregulation mediated the association between depressive tendencies and quality of life among clinically stable outpatients with bipolar disorder Our findings demonstrated that emotional dysregulation occurs in the early stage of severe mental disorders, such as the first episode.
Surprisingly, we only determined significant differences in appetite hormone levels (high insulin and low adiponectin) among adolescents with first-episode bipolar disorder after adjusting for BMI and clinical symptoms. Coello et al.Reference Coello, Vinberg and Knop 27 demonstrated that higher levels of insulin resistance measured by the Homeostasis Model Assessment for Insulin Resistance Index were noted in newly diagnosed patients with bipolar disorder than in the controls. Bond et al.Reference Bond, Kauer-Sant’Anna, Lam and Yatham 28 found that obese patients with first-episode bipolar disorder exhibited significantly greater fasting glucose levels than nonobese patients A meta-analysis of 65 studies investigating the adiponectin levels in adult patients with bipolar disorder and major depressive disorder revealed that patients with bipolar disorder, but not those with major depressive disorder, reported significantly lower adiponectin levels compared with healthy adults.Reference Vuong, Nothling and Lombard 29 In addition, Petruzzelli et al.Reference Petruzzelli, Marzulli and Giannico 30 revealed that adolescents with first-episode schizophrenia spectrum disorders had elevated levels of insulin and the Homeostatic Model Assessment for Insulin Resistance index compared with those with affective spectrum disorders Our previous studies of patients with severe mental disorder and their unaffected siblings have shown that the unaffected siblings of patients with schizophrenia, bipolar disorder, and major depressive disorder were more likely to be diagnosed with obesity, dyslipidemia, and type 2 diabetes mellitus later in life compared with the control group.Reference Huang, Chen and Huang 31 -Reference Li, Tsai and Bai 33 The findings of our present study additionally added to the evidence that appetite hormone dysregulation occurred not only in obese patients but also in nonobese patients. The aforementioned findings may explain the potential role of appetite hormone dysregulation in the pathophysiology of severe mental disorders, especially in bipolar disorder.
Increasing evidence suggests a positive relationship between obesity and emotional dysregulation.Reference Casagrande, Boncompagni, Forte, Guarino and Favieri 34 -Reference Jones, Kauffman, Rosenfield, Smits and Zvolensky 36 Jones et al.Reference Jones, Kauffman, Rosenfield, Smits and Zvolensky 36 demonstrated that emotional dysregulation was significantly associated with BMI through emotional eating, measured by the Dutch Eating Behavior Questionnaire in adult subjects without any severe mental disorder A study of 111 undergraduate students without any severe mental disorders or eating disorders revealed an association of being overweight with emotional dysregulation and disturbed eating behaviors.Reference Casagrande, Boncompagni, Forte, Guarino and Favieri 34 Favieri et al.Reference Favieri, Marini and Casagrande 35 highlighted the effect of maladaptive emotional regulation on overeating and being overweight in children and adolescents In this study, we found a positive relationship between BMI and emotional dysregulation symptoms in nonobese adolescents with first-episode severe mental disorder.
Finally, with regard to evidence that BMI percentiles, rather than BMI, may be more appropriate for pediatric samples, our study showed a positive association between log-transformed ghrelin levels, but not BMI percentile, and emotional dysregulation. Studies have reported the potentially compensatory effect of ghrelin in the cognitive function in several clinical conditions, such as type 2 diabetes and obesity, and neurodegenerative diseases,Reference Wittekind and Kluge 37 , Reference Pradhan, Samson and Sun 38 which may echo our finding of a positive relationship between ghrelin levels and CBCL-DP scores, the sum of subscale scores for anxious/depressed, aggressive behavior, and attention problems. Wittekind et al indicated a crucial role of ghrelin in the regulation of physiological anxiety.Reference Wittekind, Kratzsch and Mergl 39 Lopez-Aguilar et al.Reference Lopez-Aguilar, Ibarra-Reynoso and Malacara 40 and Raspopow et al.Reference Raspopow, Abizaid, Matheson and Anisman 41 demonstrated that impulsive and emotional eating was associated with ghrelin and cortisol dysregulation, which was suggested that emotional eating coupled with subjective feelings of hunger, might contribute to eating in response to a psychological stressor. Rossi et al.Reference Rossi, Cassioli and Gironi 42 further revealed that ghrelin levels were positively associated with emotional eating, particularly among those who experienced childhood trauma Evidence has supported a pivotal relationship of childhood trauma with the severe mental disorders as well as severe emotional dysregulation.Reference Teicher, Gordon and Nemeroff 43
Our study had several limitations. First, the cross-sectional design of our study precluded inference on the causal association of emotional dysregulation with BMI/BMI percentile and appetite hormone dysregulation among adolescents with a severe mental disorder. Second, patients continued taking their medications during the study assessment, which provided more realistic data. Studies have suggested a beneficial effect of medications on emotional dysregulation but a possible harmful effect on appetite hormones and BMI/BMI percentile. Our study design was more ethically appropriate with respect to high relapse risk in adolescents with a severe mental disorder. Third, eating behaviors were not assessed in this study, although patients with eating disorders were excluded. Further studies should clarify the effect of eating behaviors on emotional dysregulation, appetite hormones, and severe mental disorder. Fourth, BMI was in relationship with CBCL-DP scores, but this happened in only two of four of the GLMs in our study, which may be owing to the different weights of appetite hormone levels and their association with BMI in the models. Further studies would be necessary to validate our results.
In conclusion, adolescents with first-episode schizophrenia, bipolar disorder, and major depressive disorder exhibited significantly higher emotional dysregulation symptoms in the early stage of disease compared with the control group, which may indicate that emotional dysregulation is a transdiagnostic feature across severe mental disorders. In addition, adolescents with first-episode bipolar disorder reported higher levels of insulin and lower levels of adiponectin compared with the controls. The positive associations of BMI and ghrelin levels with emotional dysregulation symptoms were noted in nonobese adolescents with first-episode severe mental disorder. Our study may recommend clinicians to closely monitor BMI/BMI percentile and related appetite hormones among adolescents with first-episode severe mental disorder, particularly those with severe emotional dysregulation. Further studies must clarify the uni- or bidirectional association of emotional dysregulation with BMI/BMI percentile and appetite hormones among patients with severe mental disorder.
Acknowledgment
We thank Mr I-Fan Hu for his support and friendship.
Financial Support
The study was supported by grant from Taipei Veterans General Hospital (V111C-010,V111C-040, V111C-029), Yen Tjing Ling Medical Foundation (CI-109-21, CI-109-22,CI-110-30), Ministry of Science and Technology, Taiwan (MOST110-2314-B-075-026,MOST110-2314-B-075-024 -MY3, MOST 109-2314-B-010-050-MY3, MOST111-2314-B-075-014 -MY2, MOST 111-2314-B-075 -013), Taipei,Taichung, Kaohsiung Veterans General Hospital, Tri-Service General Hospital,Academia Sinica Joint Research Program (VTA112-V1-6-1) and Veterans GeneralHospitals and University System of Taiwan Joint Research Program (VGHUST112-G1-8-1).The funding source had no role in any process of our study.
Author Contributions
M-H.C., Y-M.B., and J-W.H. designed the study and wrote the protocol. M-H.C. and L-C.C. performed the statistical analyses and draft manuscript. Y-M.B., J-W.H., K-L.H., T-P.S. and S-J.T. reviewed the draft and revision, assisted with the preparation and proof-reading of the manuscript. All authors contributed substantially to the manuscript, and approved the final manuscript for submission. All authors are responsible for the integrity, accuracy and presentation of the data.
Disclosures
The authors do not have any conflicts of interest to declare. All authors have no financial relationships relevant to this article to disclose.








