LEARNING OBJECTIVES
After reading this article you will be able to:
• understand what EMDR is and how it is conducted
• understand the approved indications and contraindications for the use of EMDR
• appreciate the availability of evidence supporting the effectiveness of EMDR in treating PTSD.
In March 2002, the UK was gripped by the story of Milly Dowler, a 13-year-old schoolgirl who went missing and 6 months later was found to have been murdered. Following their traumatic experiences with the investigation and trial, which generated strong public criticism of the way the Dowler family had been treated in court, Milly's mother Sally and sister Gemma were diagnosed with post-traumatic stress disorder (PTSD). They have since spoken about how they were able to heal from this tragic experience through their engagement in eye movement desensitisation and reprocessing (EMDR) therapy (Williams Reference Williams and Bell2018).
Post-traumatic stress disorder
Potentially traumatic events
Potentially traumatic events (PTEs) such as the experiences of the Dowler family are unfortunately prevalent in everyday life. They are defined in the DSM-5 as events that include directly experiencing or witnessing threatened death, serious injury or sexual violence or learning that such an event has occurred to a loved one (American Psychiatric Association 2013). Several population studies have shown that a significant proportion of people have experienced at least one PTE in their lifetime. For example, Costello et al (Reference Costello, Erkanli and Fairbank2002), studying 1420 children and adolescents and their parents or guardians in the USA, estimated that one-quarter of this population had experienced at least one high-magnitude (extreme stressor) event by age 16 and one-third had experienced a low-magnitude (other potentially stressful) event in the preceding 3 months. Hepp et al (Reference Hepp, Gamma and Milos2006), in a study involving 4547 adults in Switzerland, found the weighted lifetime prevalence of PTEs to be 28%. The most commonly occurring PTEs include the unexpected death of a loved one, motor vehicle accidents and being assaulted (Breslau Reference Breslau, Kessler and Chilcoat1998).
Given the high prevalence of PTEs, it is important to study how these experiences can affect mental and physical health. Although not all adverse life events result in PTSD, there has been a wealth of evidence connecting the two (Santiago Reference Santiago, Ursano and Gray2013; Kessler Reference Kessler, Aguilar-Gaxiola and Alonso2017). Where PTSD does occur, the disorder is defined in DSM-5 as consisting of exposure to actual or threatened death, serious injury or sexual violence; presence of one or more intrusion symptoms associated with the traumatic event; persistent avoidance of stimuli associated with the traumatic event; presence of negative cognitions and associated mood symptoms; and changes in arousal and reactivity associated with the traumatic event. These changes should have been present for more than 1 month and must be associated with impairment in functioning (American Psychiatric Association 2013).
Prevalence of PTSD
Helzer et al (Reference Helzer, Robins and McEvoy1987) estimated the prevalence of PTSD in the general American population to be 1%, rising to 3.5% in civilians exposed to physical assault and unwounded Vietnam veterans and reaching 20% in wounded Vietnam veterans. A later study (Kessler Reference Kessler, Sonnega and Bromet1995) put the prevalence at 7.8% for the general American population, whereas a more recent systematic review (Santiago Reference Santiago, Ursano and Gray2013) found an estimated prevalence of 28.8% (range 3.1–87.5%) at 1 month, reducing to 17.0% (range 0.6–43.8%) at 12 months following exposure to trauma. It is thought that the effects of trauma could be differential over the life course. Ogle et al (Reference Ogle, Rubin and Berntsen2013) found that events that occurred with greater frequency early in life were associated with more severe PTSD symptoms compared with events that occurred with greater frequency during later decades of life. The experience of PTEs has been connected with the development of sleep disturbances (Milanak Reference Milanak, Zuromski and Cero2019), depression (Tracy Reference Tracy, Morgenstern and Zivin2014), substance use (Khoury Reference Khoury, Tang and Bradley2010), and other trauma- and/or stressor-related disorders, such as acute stress disorder, adjustment disorder and bereavement-related disorders (O'Donnell Reference O'Donnell, Alkemade and Creamer2016).
In addition to their effects on mental health, it has been well established that PTEs have negative effects on physical health. A cross-sectional study of 38 051 participants across 14 countries by Scott et al (Reference Scott, Koenen and Aguilar-Gaxiola2013) found a dose–response association between the number of adverse life events and the odds of developing a physical health condition (OR = 1.5, 95% CI 1.4–1.5 for one adverse life event; OR = 2.1, 95% CI 2.0–2.3 for five or more), independent of PTSD and other mental illnesses. Implicated physical health conditions were arthritis, back and neck pain, heart disease, high blood pressure, diabetes and peptic ulcer disease. Keyes et al (Reference Keyes, McLaughlin and Demmer2013), studying more than 2500 adult African Americans in Detroit, Michigan, found that respondents with the highest levels of PTE exposure (eight or more events) had an average age at diagnosis of an adverse physical health condition that was 15 years earlier than respondents with no exposure. Furthermore, there was a positive correlation between the number of PTEs and the risk of developing arthritis.
A meta-analysis by Pacella et al (Reference Pacella, Hruska and Delahanty2013) examined the association between PTSD and physical health outcomes. The results revealed a significantly greater number of general health symptoms and general medical conditions, as well as a poorer overall health-related quality of life in those with PTSD. PTSD was found to be associated with an increased frequency and severity of pain, cardiorespiratory symptoms and gastrointestinal complaints. There is also substantial evidence that PTSD is associated with an increased risk of cardiovascular disease (Buckley Reference Buckley, Tofler and Prigerson2013). This association has been observed across military and civilian populations and exists independent of other risk factors. It has been postulated that PTSD may lead to adverse physiological changes, which then lead to transient ischaemia, plaque disruption and thrombosis, resulting in the development of acute coronary syndrome. Hence, the recognition and treatment of trauma, PTSD and related sequelae should be considered important public health goals (Magruder Reference Magruder, McLaughlin and Elmore Borbon2017).
Psychotherapeutic interventions
A variety of psychotherapeutic options are available for the treatment of traumatic experiences and PTSD, including prolonged exposure therapy, cognitive–behavioural therapy (CBT) and cognitive processing therapy. However, EMDR has recently been gaining favour in the treatment of these conditions. It is distinguished by its potential to reduce the symptoms associated with traumatic memories in fewer sessions, as well as its ability to resolve trauma without the patient necessarily needing to discuss the details of the event in great depth. This article therefore aims to cover what EMDR therapy is, what the procedure entails, the evidence supporting its efficacy in treating PTSD, and indications and contraindications for its use.
What is EMDR?
EMDR is a psychotherapeutic technique that is used to help people recover from traumatic experiences. It was initially developed in the late 1980s by psychologist Francine Shapiro as a treatment for PTSD. Shapiro had accidentally discovered that making saccadic eye movements while concentrating on her own distressing memories resulted in the disappearance of recurring, disturbing thoughts. She noticed that if these memories were subsequently retrieved, they occurred without any of their disturbing emotional correlates. Shapiro then began to test the effects of these saccadic eye movements on traumatic memories in hundreds of treatment sessions with clients and, based on her clinical observations, she developed the eye movement desensitisation (EMD) procedure. In this procedure, the individual would follow the therapist's finger with their eyes as it was moved rapidly from side to side 10–20 times while they simultaneously visualised the traumatic event and internally held on to the associated negative cognitions. Shapiro's preliminary testing suggested that EMD had the ability to desensitise a traumatic memory within a short period of time to produce positive cognitive and behavioural changes. The efficacy of EMD was formally evaluated in a randomised controlled study in which 22 volunteers who suffered from traumatic experiences were randomly assigned to a treatment group that received EMD or a control group. Those in the control group were instructed to imagine and describe the memory without eye movements. The results suggested that a single session of EMD was effective in reducing the anxiety and changing the cognitions associated with traumatic memories, with the effects being maintained at the 3-month follow-up (Shapiro Reference Shapiro1989). Shapiro continued to develop the EMD procedure based on feedback from clients and other clinicians and over time, developed the current eight-stage process that was eventually renamed EMDR.
The modern EMDR procedure is a highly structured process that is typically undertaken in a series of sessions with a trained therapist (the details of the procedure are discussed in the next section). The basis of EMDR lies in the belief that negative cognitions are not the cause of present dysfunction but rather are a symptom of inadequate processing of past traumatic experiences. Therefore, EMDR has evolved into a comprehensive approach that seeks to address the past, present and future. Termed the ‘three-pronged approach’, focus is given to past traumatic events that underlie the person's symptoms, current triggers and worries that cause distress, and the development of skills and behaviours required for future wellness (Shapiro Reference Shapiro2007). It continues to utilise bilateral sensory stimulation, which may include saccadic eye movements, rhythmic sounds or tactile stimulation on the hands, during the active recall of traumatic memories.
Theoretical underpinnings
The theory behind how EMDR works is based on the adaptive information processing model. When new experiences are processed by the brain, they are assimilated into already existing memory networks, which are the basis of our perceptions, attitudes and behaviours. According to this model, trauma causes a disruption in this information processing, resulting in unprocessed experiences being stored maladaptively in their own neural network, unable to link up with other networks that hold adaptive information. These unprocessed memories still contain the thoughts, emotions and physical sensations that occurred at the time of the event and so when they are triggered, these distressing elements are re-experienced, causing the symptoms of PTSD (Solomon Reference Solomon and Shapiro2008). Therefore, the goal of EMDR is to reprocess traumatic memories by changing the way they are stored in the brain to relieve the distressing symptoms associated with them. It is not known exactly how EMDR achieves this effect; however, it is thought that bilateral stimulation while recalling a traumatic memory helps to accelerate the innate processing system to facilitate the linkage of this unprocessed memory to adaptive memory networks.
A significant amount of research has been conducted to both further elucidate its mechanism of action and further characterise its efficacy in treating trauma, in addition to a variety of mental illnesses. On the basis of this research, EMDR has been recognised by many organisations, including the American Psychiatric Association, the American Psychological Association, the International Society for Traumatic Stress Studies, and the World Health Organization, as an effective treatment for trauma and PTSD.
How is EMDR done?
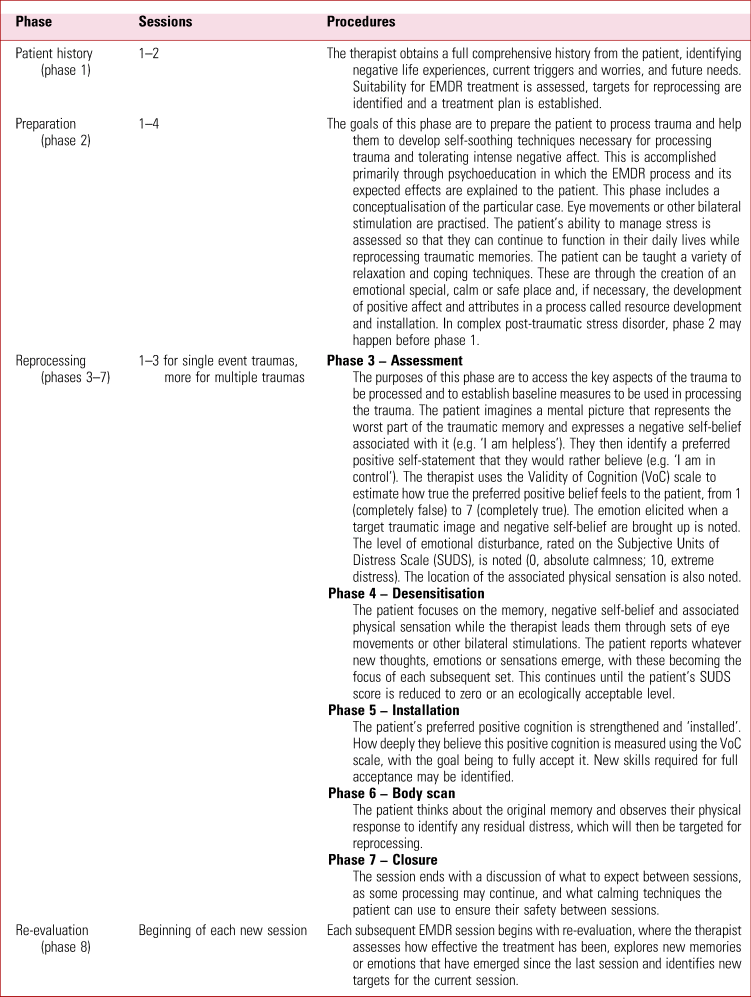
The EMDR procedure utilises a highly structured, systematic approach comprising eight phases that focus on identifying the negative life experiences that are causing dysfunction, reprocessing and desensitising those memories, and developing the necessary skills and behaviours for future success. Its procedure is divided into history taking (phase 1), preparing the patient (phase 2), reprocessing the memory (phases 3–7) and re-evaluation of treatment effects (phase 8). Although EMDR is typically delivered one to two times per week for a total of 6–12 sessions, the timeline depends on the patient; those who have experienced a single-event trauma generally require fewer sessions, whereas those with more complex histories may require more sessions. A typical EMDR therapy session usually lasts from 60 to 90 min. An overview of the EMDR procedure is given in Table 1. A detailed case example illustrating the full EMDR procedure can be found in Shapiro (Reference Shapiro2007).
TABLE 1 Overview of eye movement desensitisation and reprocessing (EMDR) treatment procedures
It is important to note that EMDR, although most commonly done via saccadic eye movements, may also be carried out with auditory stimulation, tapping or alternate tactile stimulation. Patients might listen through headphones, follow flashing lights, be tapped on the shoulders or thighs if appropriate, hold on to tactile pulsers, or wear tactile pulsers in their socks and shoes. EMDR has been used not only with adults but also with children, adolescents and the elderly (Wanders Reference Wanders, Serra and de Jongh2008; Gielkens Reference Gielkens, Vink and Sobczak2018; Hoogsteder Reference Hoogsteder, ten Thije and Schippers2022).
Information and training
The following professional associations are among those offering information on EMDR and approved training:
• EMDR Association UK (https://emdrassociation.org.uk/)
• EMDR All-Ireland Association (https://emdrireland.org/)
• EMDR International Association (EMDRIA) (https://www.emdria.org/).
How is EMDR different from other therapies?
Eye movement desensitisation and reprocessing is different from other psychotherapies in a variety of ways. Perhaps the greatest difference is that EMDR does not directly challenge the emotions, thoughts and behaviours associated with traumatic experiences as other therapies, such as CBT, do. Instead, EMDR focuses on the memories themselves, aiming to change the way the memory has been processed and stored in the brain in order to alter the negative emotions and cognitions and alleviate symptoms that stem from the trauma. This focus is core to the theory behind EMDR, which views negative emotions and cognitions not as the cause of symptoms but as symptoms themselves of inadequately processed events. Another significant difference between EMDR and other trauma-focused therapies, such as exposure therapy, is that EMDR does not include extended exposure to the distressing memory or talking in great detail about the trauma. Also, there is no major homework involved. Finally, those who are good candidates for EMDR may be able to complete therapy and achieve resolution of their symptoms in fewer sessions than with most common psychotherapies (Nijdam Reference Nijdam, Gersons and Reitsma2012).
EMDR is considered an integrative therapy that embraces aspects of cognitive therapy, the free association of psychodynamic therapy, and mindfulness with brief but interrupted exposure to emotionally activating memories while focusing on dual attention or somatic stimuli (Shapiro Reference Shapiro2018).
Approved indications for EMDR
The effectiveness and role of EMDR in the management of PTSD appears to be incontrovertible. Across various medical jurisdictions and internationally relevant organisations, the role of EMDR has been comprehensively defined and its usefulness established in the psychological management of PTSD. EMDR is recognised as a standard treatment for PTSD in the UK, Canada and the USA. A summary of the guidelines and recommendations from a number of countries and specialist organisations can be found in Box 1.
BOX 1 Approved indications for eye movement desensitisation and reprocessing (EMDR) in various countries and specialist organisations
UK
National Institute for Health and Care Excellence (NICE) guidelines (2018) recommend the consideration of EMDR for children and young people aged 7 to 17 years with a diagnosis of PTSD if they do not respond to trauma-focused cognitive–behavioural therapy (CBT) and present more than 3 months after a traumatic event.
In adults, the guidelines recommend:
• considering EMDR for a diagnosis of PTSD or clinically important symptoms of PTSD if presenting between 1 and 3 months after non-combat-related trauma and this is the individual's preferred therapy
• offering EMDR for a diagnosis of PTSD or clinically important symptoms of PTSD if presenting more than 3 months after non-combat-related trauma.
Canada
Clinical practice guidelines recommend EMDR as an effective first-line option for the treatment of PTSD. They report that the benefits are maintained during long-term follow-up of up to 10 years after treatment (Katzman Reference Katzman, Bleau and Blier2014).
USA
The American Psychological Association's (APA's) clinical practice guideline for the treatment of PTSD does not give recommendations for using EMDR as a first- or second-line intervention.
The guideline does conditionally recommend EMDR as an intervention for PTSD; however, the guideline review panel believes that this recommendation could be changed from ‘conditional’ to ‘strong’ in future updates, in light of their review of evidence in randomised trials published after the publication of the systematic review used for the guideline (Courtois Reference Courtois, Sonis and Brown2019).
The APA's practice guideline for the treatment of patients with acute stress disorder and PTSD indicates that EMDR is an effective treatment for core symptoms of acute and chronic PTSD. However, it does not recommend EMDR as an early or preventive intervention for PTSD (Ursano Reference Ursano, Bell and Eth2004).
World Health Organization
The WHO (World Health Organization 2013) recommends EMDR as a ‘standard’ intervention for consideration for adults with PTSD, with the quality of evidence rated as moderate and on a par with individual CBT with a trauma focus.
It also recommends EMDR as a ‘standard’ intervention for consideration for children and adolescents with PTSD, although the quality of evidence is rated as low.
International Society for Traumatic Stress Studies
The ISTSS practice guidelines (Forbes Reference Forbes, Bisson and Mondon2020) ‘strongly’ recommend EMDR therapy for the treatment of children and adolescents with clinically relevant post-traumatic stress symptoms. EMDR therapy within the first 3 months of a traumatic event is recommended as an early psychosocial intervention for the treatment of PTSD symptoms in adults.
EMDR is ‘strongly’ recommended as a psychological treatment for adults with diagnosed PTSD.
Evidence supporting the effectiveness of EMDR for PTSD
Since 2000, at least 12 systematic reviews and meta-analyses and numerous randomised controlled trials (RCTs) have investigated the effectiveness of EMDR as a treatment for PTSD. These studies and their findings are summarised in supplementary Table 1, available at https://doi.org/10.1192/bja.2022.32.
Considering the more recent of these studies, a systematic review and meta-analysis by Cuijpers et al (Reference Cuijpers, van Veen and Sijbrandij2020) analysed 77 studies and came to the conclusion that EMDR had a large treatment effect size when compared with control conditions in the short-term treatment of PTSD. Their review involved all age groups and considered the use of EMDR for any mental health problem. A systematic review and meta-analysis by Lewis et al (Reference Lewis, Roberts and Andrew2020) showed that, along with trauma-focused CBT, EMDR had the highest level of evidence in the treatment of PTSD. Their analysis included 141 RCTs and 8171 participants. Another meta-analysis, by Chen et al (Reference Chen, Hung and Tsai2014), considered studies reported between 1991 and 2013 that investigated the effects of EMDR not only on symptoms of PTSD but also on symptoms of depression and anxiety. They found that there was a moderate treatment effect size on the reduction of PTSD symptoms. As well, there was a moderate reduction in depressive and anxiety symptoms. Finally, a significant reduction in PTSD symptoms in children treated with EMDR was reported in a meta-analysis by Rodenburg et al (Reference Rodenburg, Benjamin and de Roos2009). Additionally of note was a meta-analysis by Lee & Cuijpers (Reference Lee and Cuijpers2013), who set out to investigate whether the use of eye movements was a necessary component for the reprocessing of traumatic memories. They found a significant, medium effect size advantage with the use of eye movements compared with no eye movements.
In summary, several systematic reviews and meta-analyses have established EMDR as an effective treatment for PTSD in children, adolescents and adults, thereby providing strong evidence to support its place in current guidelines and recommendations.
EMDR for specific traumatic experiences
The abovementioned studies explored the use of EMDR in treating PTSD. However, research has also been conducted into the use of EMDR to treat symptoms stemming from specific types of trauma in patients with or without subsequent PTSD.
Grief and loss
The death of a loved one can be a very distressing experience. In line with the adaptive information processing model, it is thought that the associated memories may be improperly stored in the brain, preventing access to adaptive information, such as positive memories of the deceased. Therefore, EMDR may facilitate appropriate movement through the mourning processes, reducing dysfunctional symptoms in those who are struggling with grief. This idea has been supported by the results from three RCTs.
An RCT by Meysner et al (Reference Meysner, Cotter and Lee2016) randomly assigned 19 participants struggling with grief to 7 weeks of either EMDR or CBT. Participants in both groups improved on measures of grief, trauma symptoms and distress but not on a measure of quality of life. There were no significant differences in outcomes between the two groups, suggesting that both treatments were efficacious. Two weeks after completing this study, a semi-structured interview was conducted with participants to explore their experiences with the two approaches (Cotter Reference Cotter, Meysner and Lee2017). Participants in both groups reported developments in insight, a positive shift in emotions, increased activity, improved self-confidence and a healthier mental relationship with the deceased. Additionally, participants who received EMDR reported that distressing memories were fewer and felt more distant.
Additionally, two RCTs have assessed a combined treatment approach for grief. van Denderen et al (Reference van Denderen, de Keijser and Stewart2018) compared symptoms of complicated grief and PTSD in 85 individuals bereaved by homicide who were assigned to either an eight-session treatment encompassing CBT and EMDR or a waiting list. Compared with the waiting list, there was a significant reduction in complicated grief and PTSD symptoms following treatment with EMDR plus CBT. Lenferink et al (Reference Lenferink, de Keijser and Smid2020) randomly assigned 39 participants who had experienced loss related to a major plane crash to either cognitive therapy plus EMDR or a waiting list control. Changes in self-rated persistent complex bereavement disorder (PCBD), depression and PTSD levels were explored. The treatment group showed a significantly stronger decline in depression compared with waiting-list controls; however, there were no significant between-group differences found in PCBD and PTSD levels. Symptom reductions were correlated with reductions in maladaptive cognitive–behavioural variables.
The results of these studies suggest that, given the common overlap between trauma and grief in the experience of loss, EMDR may be effective in reducing the associated symptoms of distress; however, further research is needed to assess whether EMDR is effective on its own or if it is best utilised in combination with CBT.
Sexual assault
Three studies have investigated the use of EMDR in treating anxiety, depression and trauma symptoms in women who have experienced sexual assault. Rothbaum (Reference Rothbaum1997) randomised 21 participants who had been sexually assaulted to either three sessions of EMDR or a waiting list. Those treated with EMDR improved more on depression and PTSD scores compared with the control group. However, the author notes that the study suffered from a small sample size and a lack of comparable treatment as a control.
Scheck et al (Reference Scheck, Schaeffer and Gillette1998) conducted an RCT in which 60 women aged 16–25 who had experienced traumas such as rape or childhood molestation were randomly assigned to receive two sessions of either EMDR or active listening. Although both groups improved on measures of anxiety, depression and PTSD symptoms, greater improvements were found in the EMDR group, which were enough to place these participants in the normal range post-treatment. These results are limited by the few sessions of treatment offered, the self-report nature of the outcome measures and the lack of objective validation that the fidelity of the study protocol was adhered to.
Mankuta et al (Reference Mankuta, Aziz-Suleyman and Yochai2012) describe their experience of providing mental health services to women who had suffered severe sexual assault, which in some cases involved genital mutilation. In their short-term project in the Democratic Republic of Congo, 23 out of 26 women diagnosed with severe PTSD were successfully treated with EMDR. There was no presentation of exactly how data changed during or after EMDR. In a similar field study in the same country, EMDR was successfully used in individual and group therapy settings (Allon Reference Allon2015).
Although these studies demonstrate the potential value of EMDR in sexual assault services, at least one study has shown that EMDR is possibly being underutilised. In a cross-sectional study of the extent to which rape crisis centres in Texas, USA, utilise EMDR therapy, Edmond et al (Reference Edmond, Lawrence and Schrag2016) found a low rate of use (at 8%). Practitioner perceptions were hindered by uncertainty regarding EMDR's effectiveness, which the authors felt reflected a lack of familiarity with EMDR, although there was strong interest in receiving training. Although this result is not generalisable, its implications are that sexual assault services may not be delivering the full array of evidence-based treatments to this vulnerable population.
Violence and abuse
Several studies have investigated EMDR's ability to reduce symptoms associated with trauma secondary to violence and abuse. Wright & Russell (Reference Wright and Russell2013) described the use of EMDR in the management of violent impulses secondary to combat exposure in the case of an active-duty marine. Following four sessions of EMDR, the marine showed improvements in obsessive violent impulses, traumatic grief and depression. The authors were careful to caution that their case demonstrates that ‘the ability to potentially intervene and prevent suicide and IPV [interpersonal violence], in whatever the numbers, can make a profound difference in the life course of those who would be victims, perpetrators, and their respective families’ members for generations to come’.
Brennstuhl et al (Reference Brennstuhl, Tarquinio and Strub2013) compared the efficacy of an EMDR emergency protocol (URG-EMDR) in treating 19 recent (defined as within 48 h) victims of physical violence in the workplace with that of eclectic therapy received by 15 similar victims. The workplaces were large-scale retail and civil service offices. Participants had to exhibit symptoms of acute stress disorder, as listed in DSM-IV, have clinical symptoms that could be attributed to the workplace incident and for which a consultation occurred within 48 h, and be first-time victims of violence or a PTE. Those taking any kind of medication were excluded. URG-EMDR resulted in a greater decrease in perceived stress and PTSD scores than eclectic therapy, to the extent that 3 months later, none of the EMDR-treated individuals exhibited symptoms of post-traumatic stress. The value of this study is that it showed that the early use of EMDR may prevent the onset of PTSD. However, the study was limited by a small sample size and a lack of longer-term follow-up. There was also no randomisation, although participants appeared broadly similar in characteristics.
Similarly, Tarquinio et al (Reference Tarquinio, Rotonda and Houllé2016) conducted an RCT investigating the efficacy of EMDR as an early intervention for workplace-based violence. In their study, 60 victims of workplace-based violence received one of three interventions: the EMDR Recent [Traumatic] Events Protocol (EMDR-RE, n = 19), Critical Incident Stress Debriefing (CISD, n = 23) or delayed EMDR-RE (n = 18). The first two interventions occurred 48 h after the event, while delayed EMDR-RE occurred 96 h thereafter. Three months on, post-traumatic stress scores were significantly lower in the EMDR-RE and delayed EMDR-RE groups compared with the CISD group. After both 48 h and 3 months, none of the EMDR-RE-treated victims showed PTSD symptoms. This study was limited by a lack of longer-term follow-up, small numbers and possible participation bias.
Evidence in the area of violence and abuse has focused more on victims of violence than on perpetrators. Interventions involving EMDR in this area are often complex and multifaceted, making it difficult to attribute improvements solely to EMDR treatment. Studies are often limited in sample size and often produce lower level evidence. Nevertheless, current evidence suggests that EMDR may be useful in resolving acute stress disorder associated with experiences of violence.
Cautions and contraindications for EMDR
There are situations where EMDR should be used with caution or where it may be contraindicated (Leeds Reference Leeds AM2009; Shapiro Reference Shapiro2002). Where a patient lacks sufficient trust to be truthful or there are dangerous or therapy-interfering behaviours, reprocessing may need to be postponed. For example, past and current acts of violence or violent urges would need to be carefully assessed and monitored to determine the individual's suitability for therapy. Patients need to have a safe means of managing emotional disturbances other than dissociating. Hence, past suicide attempts and self-harm, especially self-mutilation, need to be properly assessed. Severe life-threatening substance misuse may be problematic and may require that reprocessing be postponed until the patient is stable or in recovery. Patients should have adequate social support and should be able to contact the therapist or agreed support services for help if needed.
The general physical health of the patient must be considered as well. Severe general debility may mean that trauma processing should be put off until the patient is stronger. At times, it may be necessary for an individual to be admitted as an in-patient to minimise danger to self and others. A medical history of ocular defects, epile psy, pseudoseizures or neurological impairment would need to be carefully evaluated. Medications such as benzodiazepines can have a negative effect on the speed and generalisation of EMDR processing.
Psychosis is no longer considered an absolute contraindication for EMDR, although patients need to be properly assessed for its safe use, as it may not be appropriate in some cases of florid psychosis.
On occasion, life events, projects, work demands and schedules may make it necessary to postpone therapy. In circumstances where there is the potential for secondary gain if the illness continues, such as where there is an impending court case or outstanding compensation, the clinician and patient need to assess whether it is the appropriate time for therapy, as the patient might subconsciously resist its effects.
Lastly, it may be necessary to proceed with caution if the patient is pregnant. It may be appropriate in these circumstances to focus on recent trauma and avoid processing early adverse childhood trauma. Forgash et al (Reference Forgash, Leeds and Stramrood2013) observed that there is a dearth of RCTs or other scientific studies exploring the safety of EMDR treatment in pregnant persons. They advise that there is a high probability that EMDR will improve the pregnant person's quality of life and that the risks of adverse effects on the stability of pregnancy are probably low, but that they do remain unknown. Of course, there is a need for continuous supervision in such situations of increased risk if a decision is made to proceed with EMDR.
Summary and conclusions
Discovered by the late psychologist Francine Shapiro, EMDR has been in existence since 1987. Its primary approved use is for the treatment of PTSD. It is approved for the treatment of this condition in the USA, UK and Canada and by the World Health Organization. Earlier doubts about its efficacy have been dispelled by the emergence of meta-analyses and systematic reviews that show its superiority as a treatment for PTSD. The adaptive information processing model is used to explain the way EMDR works. According to the model, trauma causes a disruption in the normal processing of information, resulting in unprocessed experiences being stored maladaptively in their own neural network. These unprocessed memories contain thoughts, emotions and physical sensations that are reminiscent of the traumatic event and so when they are triggered, symptoms of PTSD are experienced. EMDR works by moving these frozen traumatic memories further on, to more adaptive networks where they are positively processed by the mind and body. Its processes target the past, present and future. Although commonly administered via saccadic eye movements, EMDR can also be done via bilateral tapping, alternate audio stimulation and bilateral tactile stimulation.
Conditions or situations in which EMDR may be contraindicated or should be used cautiously include ocular defects (for eye movement modality), epilepsy or pseudo-epilepsy, general physical debility, neurological impairment, past and current acts of violence and violent urges, past and current self-harm, poor social support, severe substance use, florid psychosis, pregnancy, ongoing legal processes and outstanding compensation claims.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bja.2022.32.
Acknowledgements
We are grateful to the Francine Shapiro (Electronic) Library of the EMDR International Association; the Mental Health Library at Parkwood Institute, St Joseph's Healthcare London, Ontario; and the library services of the University of Western Ontario, Canada. We thank Alexandra Richman, EMDR Approved Trainer and Approved Consultant (UK), for her practical support, and consultant psychiatrist Dr Carol McDaniel for her helpful comments on our draft paper.
Author contributions
All co-authors made equal contributions to the conception and design of the work and the acquisition, analysis or interpretation of data. All were also involved in drafting the work and revising it critically for important intellectual content. All co-authors gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
I.U. is a member of the BJPsych Advances editorial board and did not take part in the review or decision-making process of this article.
MCQs
Select the single best option for each question stem
1 According to the adaptive information processing model, the main target of EMDR therapy is:
a negative cognitions associated with a traumatic experience
b traumatic memories that have been improperly processed and stored in the brain
c a lack of self-confidence that one can face stressful situations
d maladaptive techniques for coping with symptoms of stress and trauma
e avoidance behaviours stemming from the traumatic experience.
2 As regards how EMDR is conducted:
a EMDR follows a loosely structured procedure that allows for a number of phases to be tailored to each patient
b EMDR requires patients to describe the traumatic memory in considerable detail
c EMDR may be carried out with auditory stimulation or tapping instead of eye movements
d EMDR does not incorporate a focus on developing coping skills and positive behaviours
e EMDR includes the completion of homework in between sessions.
3 Which of the following is false:
a EMDR is a recommended treatment for PTSD in adults
b EMDR is a recommended treatment for PTSD in children and adolescents
c EMDR is a recommended treatment for early post-traumatic stress symptoms in adults
d EMDR may be used in non-combat-related trauma
e EMDR is recommended for the prevention of PTSD in adults.
4 The evidence supporting the use of EMDR is:
a based on the highest level of evidence for PTSD
b based on a small number of randomised studies for PTSD
c based on lower-level evidence such as case reports
d inconclusive
e non-existent or based only on anecdotal reports.
5 Possible contraindications to the use of EMDR in treatment include:
a severe substance misuse
b general poor physical health
c self-mutilation in a person living in the community
d pregnancy
e all of the above.
MCQ answers
1 b 2 c 3 e 4 a 5 e







eLetters
No eLetters have been published for this article.