Introduction
Generalized anxiety disorder (GAD) is a chronic mental disorder characterized by excessive fear and uncontrolled worries. GAD has the lowest rate of remission after treatment when compared with other anxiety disorders (Steinert et al., Reference Steinert, Hofmann, Leichsenring and Kruse2013). One explanation for low remission rates of GAD may be that the cognitive mechanisms underlying this disorder are poorly understood, leading to poor treatment development (Kinney et al., Reference Kinney, Boffa and Amir2017).
Recently, researchers have reported that patients with GAD tend to focus on threat-related stimuli; this selective processing of information is defined as attentional bias (Mogg and Bradley, Reference Mogg and Bradley2005). Cisler and Koster (Reference Cisler and Koster2010) proposed three components of attentional bias in anxiety: facilitated attention to threat, difficulty disengaging attention from threat, and avoidance of threat. Attentional bias modification training (ABM) is a novel therapy in which patients with anxiety disorders are trained to shift their attention away from a threat-related stimulus (Bar-Haim, Reference Bar-Haim2010). Numerous studies have applied ABM in treatments of patients with GAD and proved the effect on the reduction of anxiety (Amir et al., Reference Amir, Beard, Taylor, Klumpp, Elias, Burns and Chen2009; Cisler and Koster, Reference Cisler and Koster2010). However, a recently review of these studies indicated that use of ABM for treating GAD exhibited a small effect size (Mogoaşe et al., Reference Mogoaşe, David and Koster2014). Therefore, clear evidence that ABM is an effective treatment for patients with anxiety remains lacking and more research in this area is warranted (Clarke et al., Reference Clarke, Notebaert and Macleod2014).
On the basis of cognitive models of psychopathology, cognitive behavioural therapy (CBT) works on the premise that maladaptive information processing (e.g. attention and interpretation biases) has a causal role in maintaining worry and anxiety in people with GAD, and anxiety symptoms will be mitigated if these maladaptive thinking patterns are corrected (Beck and Clark, Reference Beck and Clark1997; DeRubeis et al., Reference DeRubeis, Siegle and Hollon2008). Engagement in CBT encourages participants to consciously identify, monitor and challenge unhelpful and distressing interpretations of their experiences by behavioural exercises where participants are exposed to their feared situations (DeRubeis et al., Reference DeRubeis, Siegle and Hollon2008; Mathews, Reference Mathews2006). Randomized controlled trials (RCTs) have demonstrated that CBT can be efficacious in reducing anxiety symptoms (Hofmann and Smits, Reference Hofmann and Smits2008) and threat-related bias (Tobon et al., Reference Tobon, Ouimet and Dozois2011).
Currently, the development of modern technology has allowed for using the internet to conduct CBT at home. Internet-based cognitive behavioural therapy (ICBT) is vital to many people who might profit from treatment for psychiatric disorders (primarily anxiety and depression), especially those who are reluctant to attend mental health clinics to seek help (Kessler et al., Reference Kessler, Demler, Frank, Olfson, Pincus, Walters and Zaslavsky2005). Recent reviews suggest ICBT is feasible for anxiety disorders, and the effectiveness of ICBT and face-to-face CBT are equivalent for anxiety disorders (Andersson et al., Reference Andersson, Titov, Dear, Rozental and Carlbring2019). Even if ICBT is gradually being implemented, the process is slow and needs to be better documented.
The Unified Protocol for Trans-diagnostic Treatment of Emotional Disorders (UP) is used as the protocol of ICBT in present study. UP is a novelty cognitive behaviour group therapy (CBGT) to treat emotion disorder patients (Bullis et al., Reference Bullis, Fortune, Farchione and Barlow2014). It is an emotion-focused, cognitive behavioural intervention consisting of five core modules or components that target temperamental characteristics, particularly neuroticism and resulting emotion dysregulation, underlying all anxiety, depression and related disorders. A previous study has shown that UP produces symptom reduction equivalent to criterion standard evidence-based psychological treatments for anxiety disorders with less attrition, compared with single-disorder protocols (Barlow et al., Reference Barlow, Farchione, Bullis, Gallagher, Murray-Latin, Sauer-Zavala and Boswell2017).
Recently, there has been a new trend to develop an intervention combining ABM with other treatments to treat anxiety patients. Cognitive bias modification (CBM), which combines ABM and interpretation bias modification, has been developed as a newly emerging technique to reduce anxiety and depression symptoms (Bowler et al., Reference Bowler, Mackintosh, Dunn, Mathews, Dalgleish and Hoppitt2012). Although a recent review shows that CBM is an effective short-term treatment for adults with anxiety, the effect sizes of CBM in published studies are moderate or relatively small and none of these studies revealed a lasting effect of CBM on reduction of anxiety, or any other negative emotional outcome (Jones and Sharpe, Reference Jones and Sharpe2017). CBT and ABM target different cognitive aspects of anxiety. CBT modifies explicit and voluntary attention through verbal intervention (a top-down approach), while ABM alters implicit and involuntary attentional biases through computer-based training (a bottom-up approach). Thus, ABM may augment the effectiveness of CBT. Based on this theoretical hypothesis, Amir and Taylor (Reference Amir and Taylor2012) have examined this potential synergistic effect in adults with GAD without a control group. Shechner et al. (Reference Shechner, Rimon-Chakir, Britton, Lotan, Apter, Bliese, Pine and Bar-Haim2014) have demonstrated this synergistic effect in clinical adolescents with GAD. However, to our knowledge, there is no RCT that has yet evaluated the effectiveness of an intervention combining ICBT and ABM for adults with GAD.
Present study
In the current study, we evaluated the effectiveness of an intervention combining ICBT (UP protocol) and ABM for individuals with GAD. Consistent with the literature, all the participants in our RCT had a principal diagnosis of GAD and were divided into two groups. The treatment group received an intervention combining ICBT (UP protocol) and ABM and the control group received an intervention combining ICBT (UP protocol) and attentional bias modification placebo training (ABM-placebo). We proposed two hypotheses: (1) both the treatment group and control group would reduce anxiety symptoms and the attentional bias towards threat at post-treatment and 1-month follow-up, and (b) ABM would enhance treatment outcomes. Specifically, participants in the ICBT (UP protocol)+ABM condition would achieve greater reduction in anxiety symptoms and attentional bias towards threat, compared with participants in the ICBT (UP protocol)+ABM-placebo condition.
Method
Participants
Using the G*Power statistical package (version 3.0.10) with a value of 0.05, the calculation of sample size for this evaluation was based on previous similar studies (Amir and Taylor, Reference Amir and Taylor2012; Teng et al., Reference Teng, Hou, Chang and Cheng2019). For example, a study of GAD (n = 21) that used the same CBT protocol as the present study found medium to large effect sizes in an open trial (d = 1.69–2.6) (Amir and Taylor, Reference Amir and Taylor2012). A sample size of 20 participants will be necessary to report medium effect sizes on the outcome.
A CONSORT diagram illustrating the flow of participants throughout the study is presented in Fig. 1. Participants were recruited from the First Affiliated Hospital of Wenzhou Medical University. One hundred and fifty individuals were chosen from the psychiatric out-patient clinic to participate in the clinical interviews. Participants were eligible for the study if they were: (1) assigned a principal (most interfering and severe) diagnosis of GAD on DSM-4; (2) at least 18 years old; (3) scored at least 45 on the Beck Anxiety Inventory (BAI); and (4) volunteered to participate in the study and provided their signed informed consent. Exclusion criteria were as follows: (1) presented a current high risk of suicide; (2) currently taking anti-depressants or anxiety drugs; or (3) had received at least eight sessions of cognitive behavioural therapy within the past five years. Clinical interviews were completed by the psychiatrists using the Structured Clinical Interview for the DSM-4 (Spitzer et al., Reference Spitzer, Gibbon, Skodol, Williams and First1994). Fifty individuals did not meet the criteria, and 37 individuals refused to join in our program after interview. According to these criteria, in total, 63 participants were enrolled in the study, ranging in age from 18 to 36 years old (M = 26.09, SD = 4.93). More than half of the participants were female (57.1%). See Table 1 for a further description of participants’ demographic characteristics.

Figure 1. Flowchart of the recruitment and study procedure. IBCT, internet-based cognitive behavioural therapy; ABM, attentional bias modification training; ABM-placebo, attentional bias modification placebo training.
Table 1. Descriptive statistics for two groups

Procedure
This study was a randomized trial conducted between February 2019 and December 2019 at the First Affiliated Hospital of Wenzhou Medical University in Wenzhou, China. Sixty-three participants were divided randomly into either the treatment group (ICBT+ABM; 31 participants) or the control group (ICBT+ABM-placebo; 32 participants) by using block randomization (each block contained four numbers placed in sequentially numbered opaque sealed envelopes). The randomization was performed by a researcher who was not involved in the participant’s assessment and intervention. Therefore, until the end of the study, patients with GAD were blinded to which group they were in. Secondly, 63 participants completed a baseline assessment and started 8 weeks of treatment sessions (BL; ICBT+ABM = 31 and ICBT+ABM-placebo = 32), then 58 participants completed a post-treatment session (PT; ICBT+ABM = 29 and ICBT+ABM-placebo = 29). Finally, 50 participants returned for a 1-month follow-up assessment (FU; ICBT+ABM = 26 and ICBT+ABM-placebo = 24). During the study, five participants left the study as they required medication treatment due to increased anxiety. Eight participants did not return in follow-up sessions as they were from the countryside, and it was not convenient for them to come to the hospital.
ICBT was conducted via WeChat (social mobile application). ABM and ABM-placebo were conducted via personal computers at home. All assessments were conducted on computers (19-inch computer screen, screen resolution 1440 × 900) in the psychological assessments room at the First Affiliated Hospital of Wenzhou Medical University.
The ICBT procedure
The ICBT program was administered using a trans-diagnostic psychological treatment protocol that consisted of a therapist manual and a self-help manual (Barlow et al., Reference Barlow, Farchione, Bullis, Gallagher, Murray-Latin, Sauer-Zavala and Boswell2017). The therapist manual and self-help manual were structured as follows: (1) establish goals to enhance treatment motivation; (2) provide psychological education regarding GAD and emotions; (3) learn about awareness and perception of emotions; (4) challenge automatic thought and cognitive flexibility; (5) identify and prevent emotional avoidance patterns; (6) improve awareness and tolerance of emotion-related physical feelings; (7) expose participants to intrinsic and situational emotions; and (8) review treatment and make future plans. Sixty-three participants were divided into 10 separate groups. Therapists were randomly assigned to each group to teach the courses according to the therapist manual. Therapist courses were held weekly for ninety minutes by video calls via the social media app WeChat. After every course, participants would be asked to complete the eight modules of the CBT self-help manual, with one module each week. An assistant checked participant progress each week and recorded any problems, and therapists would provide feedback to each participant. Therapists for the study included three licensed psychologists with 10 or more years of therapy experience. They regularly conducted CBT and had been systematically trained in UP programs organized by the Chinese association for mental health. Supervision of therapists was performed as a 90-minute group supervision conducted by one experienced CBT supervisor every 2 weeks. All treatment sessions were videotaped for both supervision and the assessment of treatment integrity. Twenty per cent of treatment session videos were randomly selected and rated for adherence and competence by an external team of expert raters using standardized adherence ratings. Treatment fidelity scores was good to excellent (mean score = 4.16, total score 5).
Experiment condition: ABM procedure
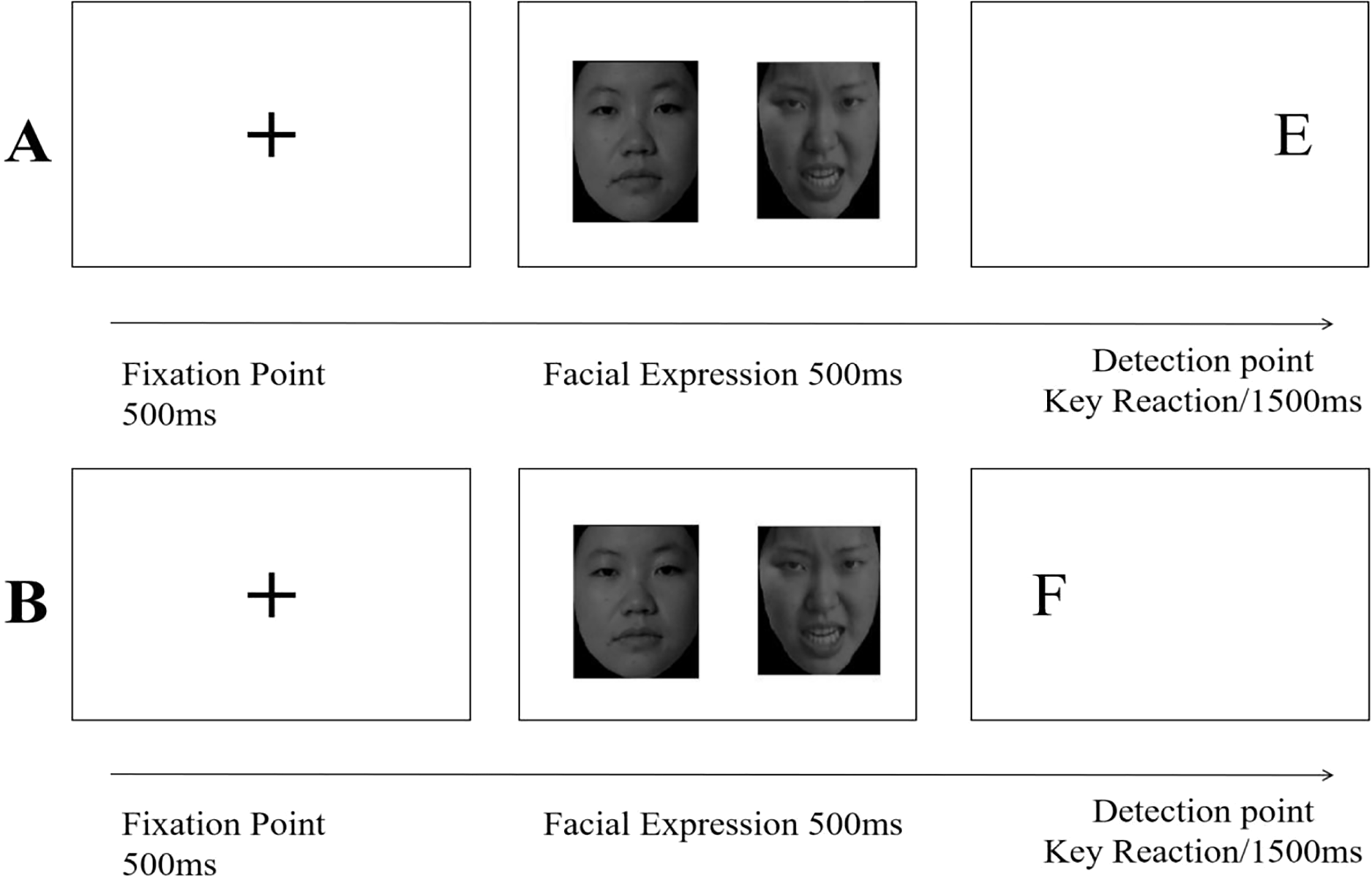
ABM training was conducted using a modified dot-probe paradigm. Pictures of emotional faces were chosen from a Chinese emotional face-picture system (Gong et al., Reference Gong, Huang, Wang and Luo2011). Forty images were selected from the angry face database and the corresponding (same person or similar) images were selected from the neutral face database. Thus, 40 angry–neutral pairs of face images were used: 20 for the attention bias assessment (ABA) task and 20 for ABM/ABM-placebo training. The images were 5 cm × 5 cm. Within each block, angry–neutral face pairs were shown side by side in 80 trials. The remaining 20 trials contained neutral–neutral pairs. For each trial, a fixation cross (+) appeared at the centre of the computer screen for 500 ms, after which a pair of face images were displayed side by side (random left/right assignment) for 500 ms. Then, the letter probe (‘E’ or ‘F’) randomly replaced one of the two images. The participants were required to indicate the location of the letter by pressing a key on the keyboard (key ‘F’ and ‘J’, for letter ‘E’ and ‘F’, respectively) as quickly and accurately as they could. The next trial began after pressing the key or after 1500 ms (see Fig. 2 for a diagram of the task). During the ABM condition, when the angry–neutral face pair was presented, the letter always replaced the neutral face. This way, ABM intended to train participants reducing bias toward threat repeatedly. Over time, an implicitly learned bias away from threat is induced because such contingency provides prediction about target location.

Figure 2. Trials of attentional bias assessment, ABM and ABM-placebo. Two stimuli differing in emotional valence (threat or neutral) are presented at the same time usually for 500 ms and then followed by a letter. In the attentional bias assessment task and attentional control condition (ACC), a letter is replaced at either of the locations that the two stimuli were presented, with the same frequencies (i.e. 50%, trials A and B are equally mixed). By contrast, in the attentional bias modification, a letter is always replaced at the location of a neutral stimulus (i.e. 100%, only B trials).
Control condition: ABM-placebo procedure
ABM training was conducted using a basic dot-probe task (MacLeod et al., Reference MacLeod, Rutherford, Campbell, Ebsworthy and Holker2002). In the ABM-placebo condition, the letter replaced the neutral and disgust faces with equal frequency (same task as the ABA). Thus, neither angry nor neutral faces had signal value regarding the position of the letter.
The ABM and ABM-placebo programs were sent to participants via email. Each training session lasted for 30 minutes. After completing CBT, participants were asked to complete ABM/ABM-placebo on their personal computers at home. The frequency of ABM and ABM-placebo training were once a week for 8 weeks.
Self-report measures
The Beck Anxiety Inventory (BAI) is a 21-item self-report inventory used to assess adult anxiety level (Beck et al., Reference Beck, Steer, Beck and Newman1993). Items are rated on a 4-point scale (0 to 3). Index scores range from 0 to 63, with higher scores representing severe anxiety. A total score of more than 45 indicates clinical anxiety symptoms (Beck et al., Reference Beck, Steer, Beck and Newman1993). A large number of studies have confirmed the applicability and effectiveness of this scale in patients with clinical anxiety (Bardhoshi et al., Reference Bardhoshi, Duncan and Erford2016; De Ayala et al., Reference De Ayala, Vonderharr-Carlson and Kim2005; Steer et al., Reference Steer, Ranieri, Beck and Clark1993). In this study, the reduction of the scores of the BAI was used as primary outcome measure. Cronbach’s alpha ranged from 0.67 to 0.82 across measurement phases.
The Automatic Thought Questionnaire (ATQ) is used to assess the frequency of negative automatic thoughts which represent the explicit negative cognitive bias (Hollon et al., Reference Hollon and Kendall1980). The questionnaire includes four cognitive components of negative automatic thoughts: (1) poor adaptation; (2) negative self-concept; (3) low self-confidence; and (4) helpless. The ATQ includes 30 items such as ‘I can’t cope with these things at once’, ‘I’m a loser’ and ‘I am weak’. Items are rated on a 5-point scale that measures the frequency of automatic negative statements about the self (1, ‘not at all’; 5, ‘all the time’). The index score is the sum of all items representing negative thoughts, thus a high total score indicates a high level of automatic negative self-statements.
The Dysfunctional Attitudes Scale (DAS) is a 40-items scale used to assess dysfunctional attitudes which represent the intrinsic negative cognitive bias (Weissman, Reference Weissman and Beck1978). The DAS includes two factors. The first factor has been interpreted as ‘perfectionism’. Both labels refer to the tendencies to endorse high personal standards, be concerned about negative evaluation by others, and interpret mistakes and shortcomings as failures. For example, the item ‘If I do not do well all the time, people will not respect me’. The second factor has been interpreted as ‘approval by others’. These are different labels for the same tacit belief: that one’s happiness and self-worth is dependent on the receipt of approval, support and love from others. ‘My value as a person depends greatly on what others think of me’ is an example of an item that loads on the second factor. Items are rated on a 7-point scale (1, ‘totally disagree’; 7, ‘totally agree’). The index score is the sum of all items, with higher scores indicating more dysfunctional attitudes. Cronbach’s alpha ranged from 0.65 to 0.71 across measurement phases.
Attentional bias assessment (ABA)
ABA was conducted using a basic dot-probe task. The task was the same as the ABM-placebo task. Within each block, angry–neutral face pairs were shown side by side in 80 trials, with angry faces appearing on the right or left of neutral faces with equal probability. The formal task of ABA contained two blocks of 100 trials. The task lasted 10 minutes.
Three scores were calculated from the task data (Koster et al., Reference Koster, Crombez, Verschuere and De Houwer2004): (1) attentional bias scores (ABS): overall index, reflecting the degree of attentional bias to threat stimuli; (2) attentional alertness scores (AAS): vigilance index, reflecting the acceleration of attention to threat stimuli; and (3) attentional disengagement scores (ADS): disengagement index, reflecting the degree of difficulty to disengage attention away from the threat stimuli. Incorrect responses and response time greater than two standard deviations were not included in the final analyses. The task was programmed using e-prime 2.0 software (Psychology Software Tools, Inc., USA). Specifically, the scores for these three variables were calculated using the following equations:
 \begin{align}{\rm{ABS}} &= {\mkern 1mu} {\rm{response}}\,{\rm{time}}\left( {{\rm{letter}}\,{\mkern 1mu} {\rm{replaced}}\,{\mkern 1mu} {\rm{the}}\,{\mkern 1mu} {\rm{angry}}\,{\rm{face}},\,{\rm{in}}\,{\mkern 1mu} {\rm{angry }} - {\rm{ neutral}}{\mkern 1mu} \,{\rm{face}}\,{\mkern 1mu} {\rm{pairs}}} \right)\\
&\quad - {\rm{response}}{\mkern 1mu} \,{\rm{time}}{\mkern 1mu} \left( {{\rm{letter}}\,{\mkern 1mu} {\rm{replaced}}\,{\rm{the}}\,{\rm{neutral}}{\mkern 1mu} \,{\rm{face}},\,{\rm{in}}\,{\rm{angry}} - {\rm{neutral}}\,{\rm{face}}\,{\rm{pairs}}} \right)\end{align}
\begin{align}{\rm{ABS}} &= {\mkern 1mu} {\rm{response}}\,{\rm{time}}\left( {{\rm{letter}}\,{\mkern 1mu} {\rm{replaced}}\,{\mkern 1mu} {\rm{the}}\,{\mkern 1mu} {\rm{angry}}\,{\rm{face}},\,{\rm{in}}\,{\mkern 1mu} {\rm{angry }} - {\rm{ neutral}}{\mkern 1mu} \,{\rm{face}}\,{\mkern 1mu} {\rm{pairs}}} \right)\\
&\quad - {\rm{response}}{\mkern 1mu} \,{\rm{time}}{\mkern 1mu} \left( {{\rm{letter}}\,{\mkern 1mu} {\rm{replaced}}\,{\rm{the}}\,{\rm{neutral}}{\mkern 1mu} \,{\rm{face}},\,{\rm{in}}\,{\rm{angry}} - {\rm{neutral}}\,{\rm{face}}\,{\rm{pairs}}} \right)\end{align}
 \begin{align}{\rm{AAS}} &= {\rm{response}}\,{\mkern 1mu} {\rm{time}}\left( {{\rm{letter}}\,{\rm{replaced}}\,{\rm{the}}\,{\rm{neutral}}\,{\rm{face}},\,\,{\rm{in}}\,{\rm{neutral}} - {\rm{neutral}}\,{\rm{face}}\,{\rm{pairs}}} \right)\\
&\quad- {\rm{ response}}\,{\rm{time (letter}}\,{\rm{replaced}}\,{\rm{the}}\,{\rm{angry}}\,{\rm{face,}}\,{\rm{in}}\,{\rm{angry}} - {\rm{neutral}}\,{\rm{face}}\,{\rm{pairs)}}\end{align}
\begin{align}{\rm{AAS}} &= {\rm{response}}\,{\mkern 1mu} {\rm{time}}\left( {{\rm{letter}}\,{\rm{replaced}}\,{\rm{the}}\,{\rm{neutral}}\,{\rm{face}},\,\,{\rm{in}}\,{\rm{neutral}} - {\rm{neutral}}\,{\rm{face}}\,{\rm{pairs}}} \right)\\
&\quad- {\rm{ response}}\,{\rm{time (letter}}\,{\rm{replaced}}\,{\rm{the}}\,{\rm{angry}}\,{\rm{face,}}\,{\rm{in}}\,{\rm{angry}} - {\rm{neutral}}\,{\rm{face}}\,{\rm{pairs)}}\end{align}
 \begin{align}{\rm{ADS}} &= \;{\rm{response}}\,{\rm{time}}\,\left( {{\rm{letter}}\,{\rm{replaced}}\,{\rm{the}}\,{\rm{neutral}}\,{\rm{face,}}\,{\rm{in}}\,{\rm{angry}} - {\rm{neutral}}\,{\rm{face}}\,{\rm{pairs}}} \right)\\
&\quad - {\rm{ response}}\,{\rm{time}}\,{\rm{(letter}}\,{\rm{replaced}}\,{\rm{the}}\,{\rm{neutral}}\,{\rm{face, in}}\,{\rm{neutral}} - \,{\rm{neutral}}\,{\rm{face}}\,{\rm{pairs)}}\end{align}
\begin{align}{\rm{ADS}} &= \;{\rm{response}}\,{\rm{time}}\,\left( {{\rm{letter}}\,{\rm{replaced}}\,{\rm{the}}\,{\rm{neutral}}\,{\rm{face,}}\,{\rm{in}}\,{\rm{angry}} - {\rm{neutral}}\,{\rm{face}}\,{\rm{pairs}}} \right)\\
&\quad - {\rm{ response}}\,{\rm{time}}\,{\rm{(letter}}\,{\rm{replaced}}\,{\rm{the}}\,{\rm{neutral}}\,{\rm{face, in}}\,{\rm{neutral}} - \,{\rm{neutral}}\,{\rm{face}}\,{\rm{pairs)}}\end{align}
Data analyses
Statistical analysis was performed using SPSS version 22, and p≤0.05 was set as the limit for statistical significance. An independent sample t-test was used to ensure pre-treatment equivalence between two groups. Categorical data were analysed using the chi-square test. To examine changes in primary and secondary outcome, we conducted a 3 (pre vs post vs follow-up) × 2 (experimental vs control group) mixed analysis of variance (MANOVA). The group × time interaction was also examined by the MANOVA. In order to test specific effects, post-hoc tests were employed. BAI scores, ATQ scores, DAS scores, and the three attentional bias scores were entered as outcome variables, comprising the canonical variable used in the MANOVA analyses.
For the intent-to-treat analysis, data analysis was based on all patients who were assigned to one of the two groups. We applied last observation carried forward to account for the uncertainty resulting from missing outcome data.
Results
Participants
Our primary analyses focused on 63 people who accepted ICBT combined with ABM or ABM-placebo. Their demographic and characteristics are shown in Table 1. The participants in the two groups did not differ significantly in demographic variables at pre-test.
Effects of ICBT and ABM on self-report measures of anxiety
The mean BAI scores in the two groups were both above clinical cut-offs (45 points) prior to treatment. There was no statistical difference between the two groups at pre-treatment in the mean BAI scores (t = 0.35, p = 0.73), mean ATQ scores (t = 1.26, p = 0.22), and mean DAS (t = 1.24, p = 0.23). Furthermore, we found no significant differences in attentional bias scores (t = 0.13, p = 0.90), attentional alertness scores (t = 0.07, p = 0.95), or attentional disengagement scores (t = 0.29, p = 0.77) between the two groups at pre-treatment. The mean self-report scale results and mean letter-probe task results for the two participant groups are displayed in Table S1 in Supplementary material.
A significant time main effect on BAI scores was observed in two groups from pre-treatment to post-treatment and follow-up (p < 0.05). The group main effect was not significant (p > 0.05). Sequential Bonferroni adjusted post-hoc comparisons revealed that all participants demonstrated a reduction in mean BAI score by 23.50 points (95% CI = 14.16–32.84, p < 0.05, d = 2.11) at post-treatment and 21.15 points (95% CI = 11.81–30.49, p < 0.05, d = 1.86,) at follow-up. BAI scores in two groups were both below clinical cut-offs (45 points) at post-treatment and follow-up. The group × time interaction effect was not significant on BAI score (p > 0.05). The results of MANOVA are presented in Table S2 in Supplementary material. Figure 3 shows the change in BAI scores, respectively, for the two groups from pre-treatment to follow-up.

Figure 3. Changes in BAI scores, ATQ scores and DAS scores. The error bars denote SD.
Significant time main effects on mean ATQ scores and DAS scores were observed in two groups from pre-treatment to post-treatment and follow-up (all p < 0.05). The group main effect on DAS score was not significant (p > 0.05), while the group main effect on mean ATQ was significant (F 2,60 = 7.570, η2 = 0.123 p < 0.05). Sequential Bonferroni adjusted post-hoc comparisons for the time main effect revealed that all participants demonstrated a reduction in ATQ score by 31.40 points (95% CI = 15.49–47.31, p < 0.05, d = 1.50) at post-treatment and 30.45 points (95% CI = 14.54–46.36, p < 0.05, d = 1.35) at follow-up. All participants demonstrated a reduction in DAS score by 55.15 points (95% CI = 38.93–71.37, p < 0.05, d = 1.68) at post-treatment and 55.40 points (95% CI = 39.18–71.62, p < 0.05, d = 1.64) at follow-up. The group × time interaction effect was not significant on DAS scores and ATQ scores (p > 0.05). Figure 3 shows the change in ATQ and DAS scores, respectively, for the two groups from pre-treatment to follow-up.
Effects of ICBT and ABM on dot-probe task of attentional bias
Significant time main effects on ABS, AAS, and ADS were observed in two groups from pre-treatment to post-treatment and follow-up (F ABS(2,60) = 5.879, F AAS(2,60) = 4.064, F ADS(2,60) = 3.441, p < 0.05). The group main effect was not significant (p > 0.05). Sequential Bonferroni adjusted post-hoc comparisons for the time main effect revealed that: (1) all participants demonstrated a reduction in ABS by 0.83 points (95% CI = 0.16–1.50, p < 0.05, d = 0.96) at post-treatment and 0.77 points (95% CI = 0.10–1.44, p < 0.05, d = 0.86) at follow-up; (2) all participants demonstrated a reduction in AAS by 0.91 points (95% CI = 0.40–1.78, p < 0.05, d = 0.78) at post-treatment and 0.82 points (95% CI = –0.05–1.69, p < 0.05, d = 0.70) at follow-up; (3) all participants demonstrated a reduction in ADS by 0.76 points (95% CI = –0.07–1.58, p < 0.05, d = 0.71) at post-treatment and 0.75 points (95% CI = –0.07–1.57, p < 0.05, d = 0.71) at follow-up. The group × time interaction effects were not significant on the three attentional bias scores (p > 0.05). MANOVAs for the three attentional bias scores are presented in Table S3 in Supplementary material. Figure 4 show the change in ABS, AAS and ADS during the pre-treatment to follow-up, respectively.

Figure 4. Changes in attentional bias scores, attentional alertness scores and attentional disengagement scores. The error bars denote SD.
Discussion
Our first aim was to examine whether the ABM plus ICBT and the ABM-placebo plus ABM would reduce the anxiety symptom and the attentional bias towards threat at post-treatment and 1-month follow-up. The results suggested that both the two groups showed reductions in the scores of BAI, DAS, ATQ and ABA after treatment and at 1-month follow-up. Our second aim was to examine whether participants in the ICBT+ABM condition would achieve greater reduction in anxiety symptom and attentional bias towards threat, compared with participants in the ICBT+ABM-placebo condition. The results suggested although two groups were equivalent in reducing scores of BAI, DAS and ABA at any assessment point, the ICBT plus ABM group was superior to the ICBT+ABM-placebo in reducing the scores of ATQ after treatment and at 1-month follow-up.
Similar to our study, McEvoy and Perini (Reference McEvoy and Perini2009) divided patients with social phobia (n = 81) into cognitive behaviour group therapy (CBGT) with ABM or with relaxation training (RT). ABM did not potentiate greater change on any outcome variable, with both groups achieving significant improvements on all measures. Unlike our study, previous studies have demonstrated that, compared with a control task, ABM facilitated attentional disengagement from threats in patients with social anxiety disorder (Amir et al., Reference Amir, Beard, Taylor, Klumpp, Elias, Burns and Chen2009; Schmidt et al., Reference Schmidt, Richey, Buckner and Timpano2009). Other studies have also reported that the treatment group showed greater reduction in self-rated anxiety symptoms than the control group (Baker et al., Reference Baker, Hellberg, Jacoby, Losiewicz, Orr, Marques and Simon2020; Shechner et al., Reference Shechner, Rimon-Chakir, Britton, Lotan, Apter, Bliese, Pine and Bar-Haim2014; White et al., Reference White, Sequeira, Britton, Brotman, Gold, Berman, Bar-Haim, Leibenluft and Pine2017).One explanation for similar clinical outcomes between treatment and control groups in the present study is that the techniques used in cognitive behavioural therapy, such as behavioural experiments and thought challenging, already promote reduction of anxiety symptoms by increasing attentional flexibility and control. Second, although the control group received the attentional control condition, it might not be the most effective control. ABM-placebo may result in participants becoming fatigued of focusing on the threat stimuli and encourage them to pay more attention to neutral stimuli. A third possible explanation is that the treatment setting was not conducive to produce a differential effect. Generally, long-term training and sufficient intensity per training are recommend for attentional bias modification. To date, there is no consensus on the number of whole treatment sessions and the number of treatment trials per training. Hence further study is needed to modify and adjust the treatment settings. Finally, we should consider that the effectiveness of CBT relies on the cognitive load. Previous study has found CBM-I (cognitive bias modification for interpretation) and CBT might differ in the resilience of their effects when under cognitive load (Bowler et al., Reference Bowler, Mackintosh, Dunn, Mathews, Dalgleish and Hoppitt2012). Thus, although interventions do not differ in efficacy, they may differ in their effects under cognitive load. To investigate this possibility, we should include a measure of AB change under cognitive load.
In the present study, the treatment group showed greater reduction in ATQ scores than the control group. To date, this is the first study to use the ATQ as an outcome measure for attentional bias modification. An intervention study found the reduction of anxiety disorder symptoms was significantly associated with a decrease in negative automatic thoughts (McEvoy and Perini, Reference McEvoy and Perini2009). One study has reported that automatic thoughts are positively correlated with anxiety (Palos and Viscu, Reference Palos and Viscu2014). A more recent study has also shown that cognitive appraisal moderates the influence of attentional bias on state anxiety (Liu et al., Reference Liu, Shen and Li2019). An automatic thought is a belief that is naturally triggered by specific stimuli, related to self-evaluation, and leads to adverse behavioural reactions. This is similar to the principle of attentional bias, which occurs quickly and is related to specific stimuli. Although CBT and ABM target different cognitive aspects of anxiety (top-down vs bottom-up), bottom-up and top-down systems exert mutual influences on each other to determine whether thoughts and actions are engaged towards adaptive goals or towards processing threat information that is unrelated to current goals, and which could potentially pose a danger to the individual (Mogg et al., Reference Mogg and Bradley2016). Based on their interaction, several theoretical models have been developed to explain the mechanisms related to anxiety susceptibility, including biases in bottom-up processes of automatic threat evaluation and automatic initial orienting to threats, as well as disturbances in top-down cognitive control processes, including controlled attentional, elaboration, and over-ride of bottom-up biases (Bar-Haim et al., Reference Bar-Haim, Lamy, Pergamin, Bakermans-Kranenburg and van IJzendoorn2007; Beck et al., Reference Beck and Clark1997; Eysenck et al., Reference Eysenck, Derakshan, Santos and Calvo2007). In light of these findings, automatic thoughts may play an initial and important role in the processing of the anxiety. Although there was no between-group difference on other indexes during the period of study, as negative automatic thoughts continued to reduce, the treatment groups may have greater reduction in DAS, BAI and the three attentional bias scores than the control group in the long-term outcome. To investigate this possibility, future studies should employ a longer follow-up period of 3 months or longer.
Our study also suggested the ICBT and home-delivered ABM are feasible in the treatment with the GAD adults. ICBT and other forms of internet interventions hold promise as a way to increase access to evidence-based psychological treatment. They can also serve as vehicles for innovation, which may subsequently inform face-to-face treatments
This study has several limitations. First, the sample size was small, resulting in the representativeness of the sample likely being insufficient, and limiting the generalizability of the present findings. Second, due to the limited condition, there were only two groups in study. Although the synergistic effects of the ICBT and ABM were demonstrated in present study, future research should add a CBT-only group and waiting-list group to further clarify these outcomes. Third, the study relied heavily on measures of manual reaction time to indirectly assess the components of attentional bias, and thus cannot fully delineate the time course and components of attentional bias. Eye-tracking technology that allows relatively direct and continuous measurements of overt visual attention is recommended for future studies to provide an important supplement to RT measures.
Despite the above-described limitations, results from this RCT suggest that ABM may augment response to CBT. This study adds to the growing ABM literature, laying the grounds for future work that should focus further on examining the most effective ABM protocol and the most efficient way to implement these as augmenting treatments to CBT, and clarifying the cognitive mechanisms underlying the anxiolytic effect of ABM.
Conclusion
Participants diagnosed with GAD were recruited for this study in which ICBT combined with ABM was provided through software on personal computers. A double-blind, randomized experimental design was adopted. At baseline, self-reported anxiety scores and RT-based attentional bias scores exhibited no significant differences between treatment and control groups. However, after treatment and at 1-month follow-up, individuals in the ICBT combined with ABM showed more reduction in their automatic thoughts than control participants. Regarding other self-reported scores and attentional bias scores, all participants exhibited significant improvement in the later stages of the training, but no between-group differences were observed. The experimental results demonstrated that ABM may be a useful augmentation to CBT to reduce anxiety. Further research should add CBT-only group and waiting-list group to clarify these outcomes. Eye-tracking technology is recommended for future studies to provide an important supplement to response time measures.
Supplementary material
To view supplementary material for this article, please visit: https://doi.org/10.1017/S1352465822000480
Data availability statement
The datasets generated and/or analysed during the current study are not publicly available due to ethical restrictions and personal data protection, but are available from the corresponding author on reasonable request.
Acknowledgements
We thank all the participants for their willingness to participate in the study and the time that they devoted to the study.
Author contributions
Zijiang Lin: Conceptualization (equal), Data curation (equal), Formal analysis (equal), Funding acquisition (equal), Investigation (equal), Methodology (equal), Writing – original draft (equal); Jiaying Zhang: Formal analysis (equal), Methodology (equal); Fenzan Wu: Formal analysis (equal), Investigation (equal); Kewei Xu: Project administration (equal), Resources (equal), Software (equal); Meiliu Peng: Project administration (equal), Resources (equal), Software (equal); Changlv Wang: Project administration (equal), Resources (equal), Software (equal); Chuang Yang: Project administration (equal), Resources (equal), Software (equal); Xinhua Yang: Writing – review & editing (supporting); Xinhua Shen: Writing – review & editing (supporting); Wei Wang: Funding acquisition (equal), Methodology (equal), Writing – review & editing (equal); Yanlong Liu: Conceptualization (equal), Data curation (equal), Formal analysis (equal), Funding acquisition (equal), Supervision (equal), Writing – review & editing (equal); Li Chen: Conceptualization (equal), Data curation (equal), Formal analysis (equal), Funding acquisition (equal), Investigation (equal), Project administration (equal), Supervision (equal), Writing – review & editing (equal).
Financial support
This work was supported by the Natural Science Foundation of Zhejiang Province (grant number: LY20H090009), Wenzhou (China) Municipal Sci-Tech Bureau Program (grant number: Y20190097), and Planted Talent Plan Projects for College Students in Zhejiang Province (grant number: 2020R413074). The funders had no role in study design, data collection, analysis, interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Conflicts of interest
All authors declare no competing interests.
Ethical standards
This study was approved by the Medical Ethics Committee of the First Affiliated Hospital of Wenzhou Medical University and was performed in accordance with the principles of the Declaration of Helsinki (Clinical Trial Registration no. YS20190327).







Comments
No Comments have been published for this article.