No CrossRef data available.
Article contents
Evaluating the Generalizability of an Electronic Algorithm to Identify Vancomycin-Associated Acute Kidney Injury
Published online by Cambridge University Press: 16 September 2024
Abstract
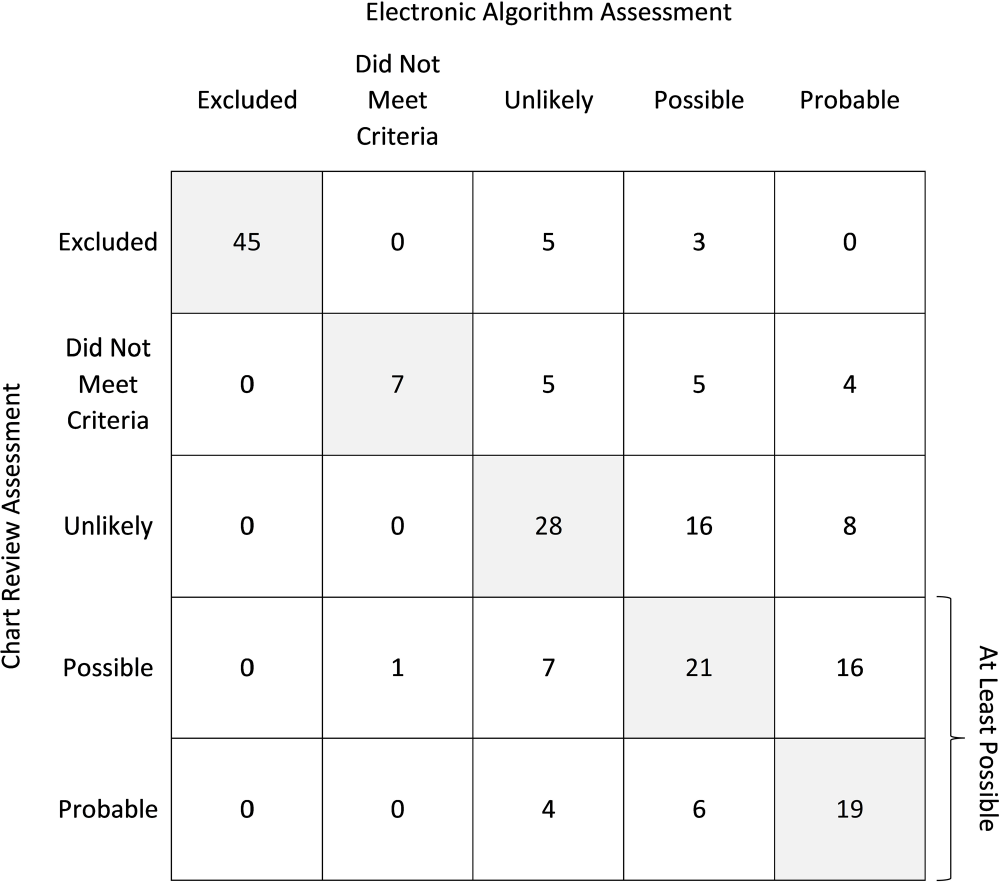
Introduction: Vancomycin-associated acute kidney injury (V-AKI) is a common adverse reaction; however, there is currently no method to systematically monitor its incidence. We previously developed and internally validated an electronic algorithm to identify cases of V-AKI using structured electronic health record data at the Johns Hopkins Hospital, which demonstrated excellent agreement with chart review (percent agreement 92.5%; weighted kappa coefficient 0.95), as well as excellent sensitivity (89.7%) and specificity (98.2%) in detecting at least possible V-AKI events. The objective of this study was to evaluate the generalizability of the V-AKI electronic algorithm. Methods: We identified a retrospective cohort of adult and pediatric patients who received ≥1 dose of intravenous vancomycin while admitted to University of Virginia (UVA) Medical Center from 1/2021-1/2023. An increase in creatinine (Cr) of ≥0.3 mg/dL within 48 hours or ≥50% increase in baseline Cr within 7 days, occurring after the first dose and up to 72 hours after the last dose of IV vancomycin, was considered a potential V-AKI event. The electronic algorithm was executed at UVA with only limited contextualization of hospital specific variables (e.g., procedure names). Patients were categorized as excluded/not meeting criteria, or as having an unlikely, possible or probable V-AKI event using a causality framework. A random subset of the cohort underwent chart review by a blinded reviewer for external validation. Percent agreement and a weighted kappa coefficient were calculated. The sensitivity and specificity in identifying at least possible V-AKI events was determined. Results: The electronic algorithm was validated using 200 cases and demonstrated 60.0% percent agreement with chart review (Figure). The weighted kappa coefficient was 0.75. The algorithm was 83.8% sensitive and 71.4% specific in detecting at least possible V-AKI events. Among the 80 discrepant cases, there was only a 1-category difference in 62.5% of cases. The most common reasons for discrepant assessments, which were partly due to inconsistencies in chart review, included disagreement regarding timing of AKI onset (18.6%) and whether renal function returned to baseline (16.3%). Conclusions: An electronic algorithm to identify V-AKI events was successfully implemented at another institution. Although agreement with chart review was only fair, sensitivity in detecting at least possible V-AKI events remained excellent. The electronic algorithm may be useful for systematically and reproducibly identifying V-AKI events across institutions in a scalable manner to inform stewardship interventions. However, further refinement of the algorithm and improvement in consistency of chart review assessments is needed.
Disclosure: Lindsay Donohue: Advisor – Abbvie
- Type
- Antibiotic Stewardship
- Information
- Antimicrobial Stewardship & Healthcare Epidemiology , Volume 4 , Issue S1: SHEA Spring 2024 Abstracts , July 2024 , pp. s54
- Creative Commons
- This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Copyright
- © The Author(s), 2024. Published by Cambridge University Press on behalf of The Society for Healthcare Epidemiology of America


