4 Mechanical ventilation
Practical Emergency Resuscitation and Critical Care, ed. Kaushal Shah, Jarone Lee, Kamal Medlej and Scott D. Weingart. Published by Cambridge University Press. © Kaushal Shah, Jarone Lee, Kamal Medlej and Scott D. Weingart 2013.
Introduction
When a patient in respiratory distress is intubated, the endotracheal (ET) tube by itself does not alleviate or reverse the underlying cause of respiratory distress. Mechanical ventilation, however, can be used to mitigate the effects of the disease process and allow the body time to heal.
Mechanical ventilation drastically alters normal respiratory physiology. We normally breathe by generating negative pressure in the thoracic cavity, while mechanical ventilation uses positive pressure at the airway opening to create a gradient that drives the flow of gas into the lungs.
Initiating mechanical ventilation is not without consequence. If done inappropriately, morbidity and mortality can dramatically increase because of the development of certain complications:
Ventilator-induced lung injury (VILI):
Lung disease does not take place uniformly throughout the lungs.
Tidal volumes preferentially inflate healthy lung tissue. Therefore, if the tidal volumes are high, this can cause stress to the alveolar–capillary interface of the normal lungs.
Barotrauma occurs as a result of excessive airway pressures and can result in a pneumothorax, a pneumomediastinum, or alveolar rupture.
Atelectrauma occurs with the continuous closing and reopening of alveoli.
Barotrauma, volutrauma, and atelectrauma can lead to the activation of an inflammatory cascade causing further injury known as biotrauma.
Ventilator-associated pneumonia (VAP):
Definitions
Inspiration: Gas flows into the lungs.
Expiration: Ventilator flow is stopped and the exhalation circuit is opened to allow gas to escape from the lungs.
Triggering: Initiation of breath.
Can be machine initiated after a set amount of time has elapsed since the last breath.
Can be patient initiated in response to a reduction of airway pressure below a preset threshold, or in response to the detection of inspiratory flow.
Limit: A parameter that is used to control inspiration. Ventilation can be either volume or pressure limited.
Cycling: Switching from inspiration to expiration.
Can occur because a certain amount of time has passed, a preset volume has been delivered, or a preset decrease in flow rate has occurred.
Minute ventilation (VE) = Tidal volume (Vt) × Respiratory rate (RR).
Common ventilator settings
Fraction of inspired oxygen (FiO2): The percentage of oxygen being delivered to the patient. It ranges between 21% and 100%.
Positive end-expiratory pressure (PEEP): Positive airway pressure applied by the ventilator at the end of expiration. PEEP prevents alveolar collapse at the end of expiration and “recruits” alveoli to participate in respiration, thereby improving gas exchange.
Respiratory rate (RR): Number of breaths delivered per minute.
Tidal volume (Vt): Volume in mL delivered in a single breath.
Inspiratory flow rate (IFR): The rate of air entry in L/minute during inspiration.
Inspiratory pressure: Set pressure used to inflate the lungs during inspiration.
Inspiratory time (Ti): The time over which the Vt is delivered.
I:E ratio: The ratio of inspiratory time to expiratory time. A normal I:E ratio is 1:2 to 1:3. Increasing the I:E ratio can improve oxygenation by increasing the mean airway pressure. A longer inspiration will result in a longer period of high pressure, thus increasing the mean airway pressure over the entire respiratory cycle.
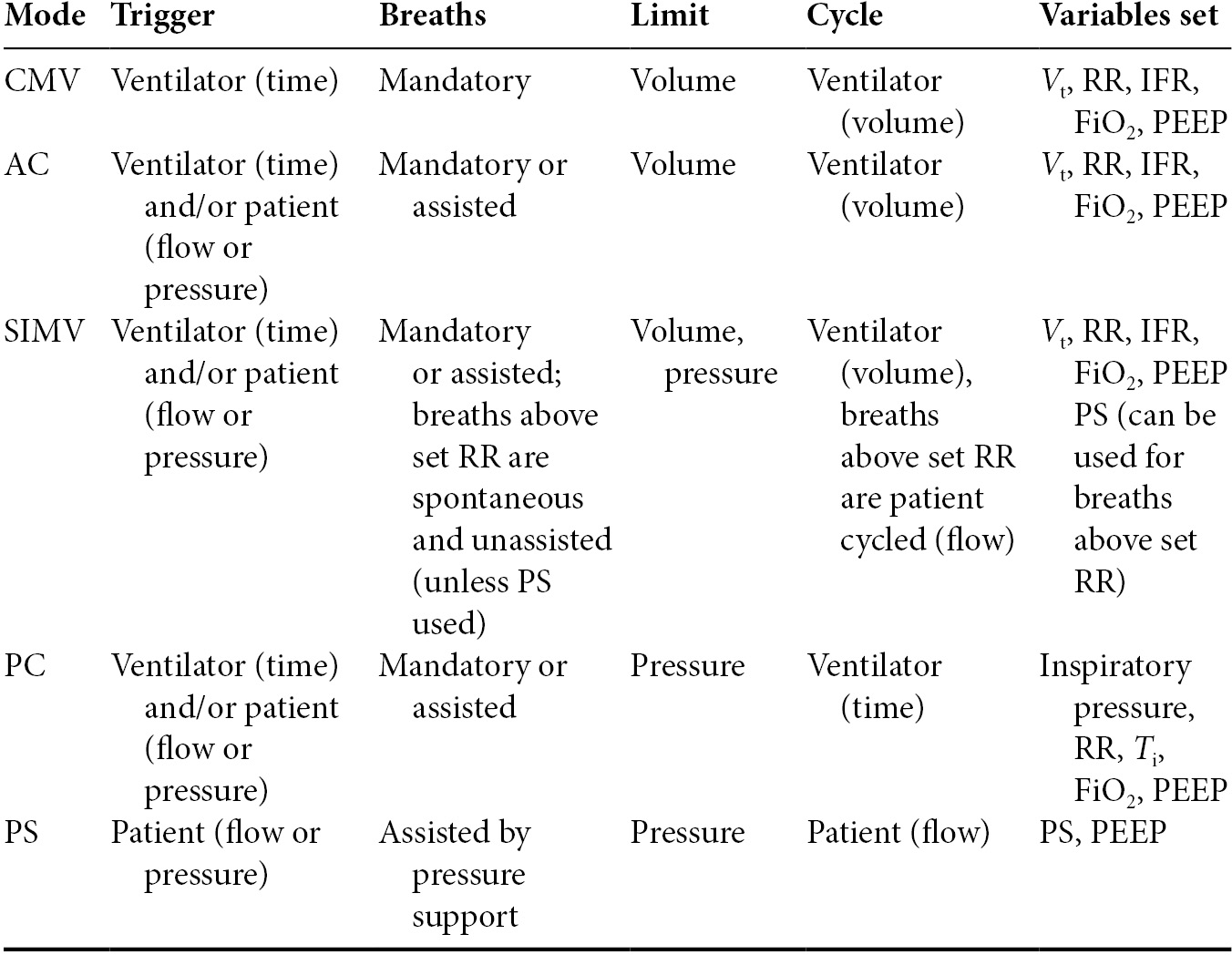
Modes of ventilation (Table 4.1)
Controlled mandatory ventilation (CMV): The ventilator controls all aspects of ventilation. A set RR and Vt are delivered by the ventilator. This mode is usually a volume-controlled mode but can also be a pressure-controlled mode. The patient has no ability to initiate breaths, breathe over the set RR, or influence the characteristics of the breath. This mode is mostly used in heavily sedated and paralyzed patients in the operating room.
Assist volume control: Commonly referred to just as Assist Control (AC). This is a volume-cycled mode of ventilation that delivers the same Vt during every breath. Breaths can be triggered by the patient or the machine. There is a set RR and Vt but the patient can breathe over the set RR. If the patient does not initiate a breath after a set time, the ventilator will initiate the breath. All patient-triggered breaths are assisted by the ventilator to produce the set Vt. This is a commonly used mode for patients in respiratory distress and has become the mode of choice in the ED.
Synchronized intermittent mandatory ventilation (SIMV): SIMV represents a combination of breathing types. It is a mix of ventilator triggered and controlled breaths and the patient’s spontaneously triggered and controlled breaths. If the patient is breathing below the set RR, then the breaths are machine assisted. If the patient is breathing above the set RR, then the patient’s breaths are spontaneous and unassisted. Unlike AC there is no guarantee of a set Vt for every breath because the Vt for the unassisted breaths depends on the patient’s respiratory effort and lung mechanics.
Pressure control (PC): PC is an assist control mode of ventilation in which the desired inspiratory pressure is set. This mode is similar to assist volume control but instead of a set Vt being delivered a set pressure is delivered. Breaths can be triggered by the machine or the patient. In this mode the RR and Ti are set which will determine the I:E ratio. Each breath is assisted by the machine and the set pressure is delivered. An advantage of this mode is the pressure limit can be set to limit barotrauma and this may improve patient ventilator synchrony. A disadvantage of this mode is that Vt will vary with each breath based on the patient’s thoracic compliance, airway resistance, and patient effort. Therefore, a set minute ventilation will not be guaranteed.
Pressure support (PS): This mode of ventilation provides partial support. The patient is spontaneously breathing and the ventilator will augment each breath with a set inspiratory pressure. The patient sets his or her own respiratory rate and Vt. This mode necessitates an intact ventilatory drive and is commonly used as a weaning modality.
Strategies of ventilation
Outlined below are two ventilation strategies that can be used in critically ill patients in the emergency department. Both of these strategies utilize the assist control (AC) volume cycled mode of ventilation.
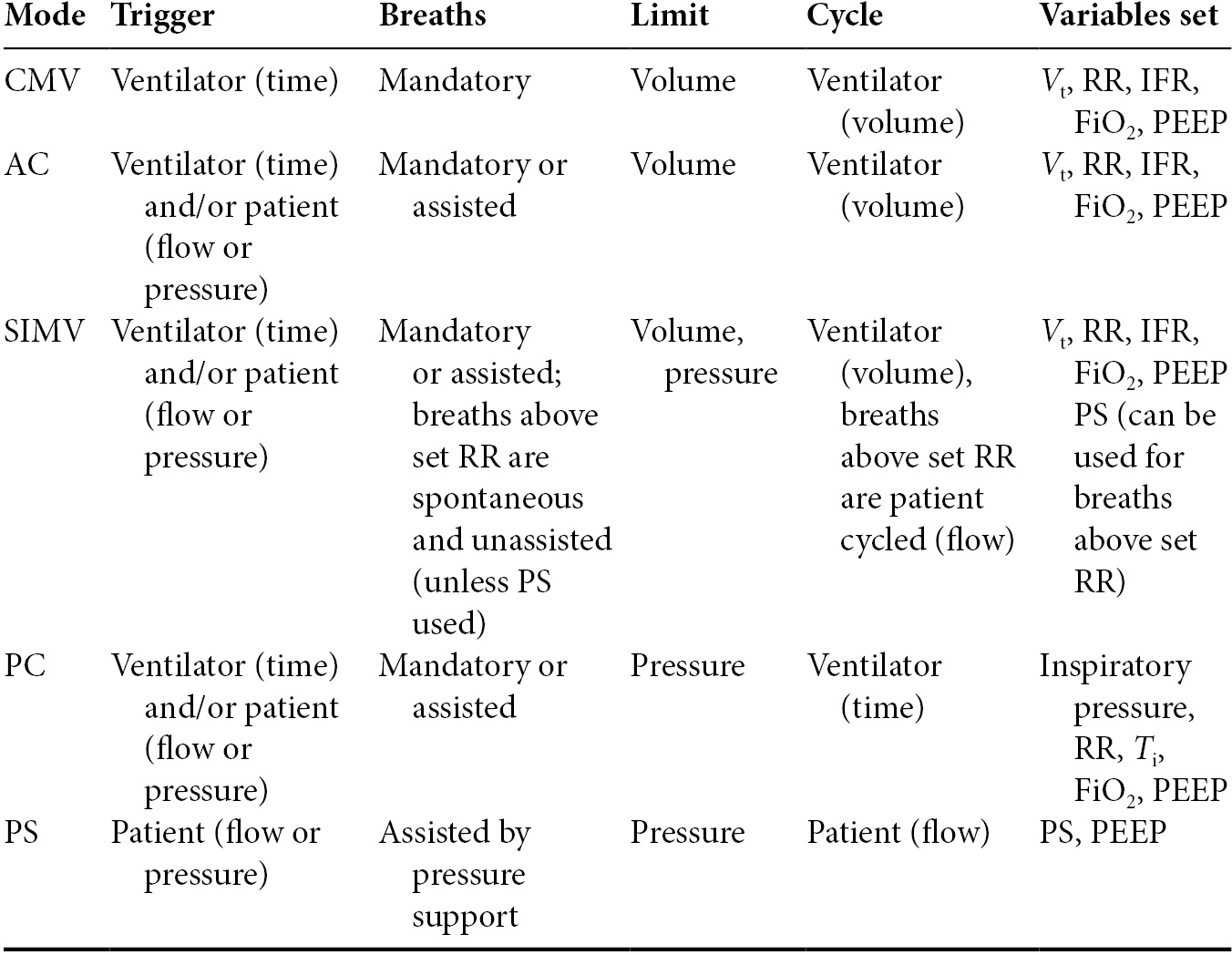
Lung protective strategy (Figure 4.1)
This strategy is designed for patients with acute lung injury (ALI) or acute respiratory distress syndrome (ARDS), or who are at risk for lung injury. The majority of patients fit into this category.
It is believed that all intubated and mechanically ventilated patients are at risk for ALI. This strategy should therefore be employed on most critically ill patients that are on a ventilator.
This ventilation strategy is derived from the ARDSNet study and has been shown to decrease mortality in patients with ALI/ARDS.
It prevents VILI by avoiding over-distension of the alveoli and preventing atelectrauma.
Figure 4.1. Ventilator settings for lung protective strategy.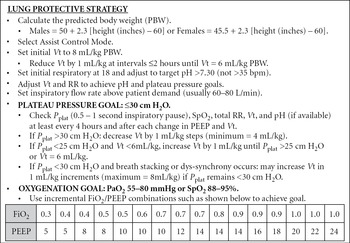
Obstructive strategy (Figure 4.2)
This strategy is designed for patients with obstructive lung disease (i.e., asthma or COPD) whose airways are constricted and therefore require a longer time to fully exhale.
They also require respiratory support for fatigued respiratory muscles during inspiration.
The basis of this strategy is to decrease the RR and adjust the IFR to achieve a prolonged I:E ratio (1:4 to 1:5). This will allow the patient sufficient time to fully exhale and avoid auto-PEEP or breath stacking.
Breath stacking is the phenomenon of delivering another breath before the lungs have completely exhaled. This results in an increased intrathoracic pressure and can cause a pneumothorax or hemodynamic instability secondary to a decrease in venous return.
Decreasing the respiratory rate results in retention of CO2 which in turn leads to a respiratory acidosis. This is referred to as permissive hypercapnia and is tolerated to a certain extent (PaCO2 <85 mmHg and pH >7.20).
Basic lung mechanics
There are two basic pressures that should be monitored in mechanically ventilated patients:
Peak inspiratory pressure is automatically measured by the ventilator. It is a function of the resistance in the airways and the compliance of the lung and chest wall.
Can be elevated in conditions that increase airway resistance, like asthma, COPD, small ET tubes, and ET tube obstruction.
Plateau pressure (Pplat) is measured after instituting a 0.5–1 second end-inspiratory pause. Since there is no airflow present at this time, the resistive component of the pressure is eliminated. Pplat is a reflection of the compliance of the lung and chest wall.
It is the more important pressure to monitor for risk of VILI because it is the pressure that is transmitted to the alveoli.
PIP and Pplat can help identify the cause of distress in a mechanically ventilated patient.
If PIP is high and Pplat is normal, airway resistance is likely high.
If PIP is high and Pplat is high, lung compliance is likely low.
If PIP is low and Pplat is low, suspect an air leak or tube dislodgment.
Sudden deterioration
Use the mnemonic DOPES on patients that are deteriorating while on the ventilator:
Dislodgment of tubes:
Check the ET tube position by direct visualization or by connecting it to quantitative EtCO2 capnography and looking for a loss of waveform.
Obstruction:
Usually from kinking of the ET tube or from a mucous plug.
Confirm with fiberoptic bronchoscopy if available.
Insert a suction catheter through the ET tube to remove the plug.
In some cases, the tube will have to be replaced.
Place a chest tube on the affected side.
If the patient is hypotensive and the side of the pneumothorax is not clear, bilateral chest tubes should be placed.
Equipment failure:
Disconnect the patient from the ventilator and ventilate with a bag valve apparatus until another ventilator is available.