9.1 Introduction
Our vulnerability to infectious diseases reminds us of how interconnected we are – to each other and to the organisms that share our environment. Because living in a bubble is impractical, we develop protective infrastructure (sanitation, surveillance, and vector control systems) and medical countermeasures (vaccines and antimicrobials). Because pathogens often outpace our ability to combat them, we use social controls to separate the sick and exposed (isolation and quarantine) and urge individuals to adopt protective behaviors (e.g. hand hygiene, appropriate use of antimicrobials). Each of these strategies relies – to varying degrees – on public health law and policy. Each will be crucial as we adapt to the infectious disease impacts of climate change.
In the United States and many other countries, legal frameworks and infrastructure for controlling the spread of infectious disease date back to the turn of the twentieth century. Public health laws developed to combat cholera, smallpox, tuberculosis, and polio using nineteenth-century technology continue to provide the basic framework for determining the obligations and authority of health officials and constraints on that authority derived from individual rights. These legal frameworks and the infrastructure on which they rely remain outdated and underfunded in spite of increased attention to the emergence of new threats, such as HIV/AIDS and bioterrorism, and renewed concerns about old threats, such as pandemic influenza. The infusion of funding and legal reforms to enhance public preparedness for bioterrorism and pandemic influenza in the early twenty-first century has limited relevance to climate change adaptation.
The fragmentary nature of the US public health system hinders its capacity to respond effectively and efficiently to infectious disease threats. Public health powers are still predominantly exercised at the local and state level, notwithstanding the federal government’s growing role in public health emergency preparedness and response. Health departments at every jurisdictional level play a principal role in infectious disease control, but they are increasingly occupied by the gargantuan task of regulating and supporting the healthcare system. By comparison, public health functions (e.g. surveillance, contact tracing, epidemiological investigation, and social distancing) receive little attention. Through a process of specialization within the administrative state, health departments have become more focused on the medical model, while other agencies have emerged to focus on environmental protection, sanitation systems, agriculture, food and drug safety, the workforce, and other social concerns relevant to preventing and responding to disease outbreaks.
The public health response to environmentally sensitive infectious disease threats such as Dengue fever, hantavirus, West Nile virus, and Zika virus provide a window into how well the system is adapting to climate change. In the words of United Nations Environment Programme Executive Director Achim Steiner, “The spread of Zika, just as with Ebola, has sent a strong signal to the international community that there is a need for increased attention to the linkages between environment and health.”Footnote 1 The warning signs are clear. Infectious disease threats that are unresponsive to available medical countermeasures, that emerge slowly, those that disproportionately affect people living in low-income households, neighborhoods, and countries, or that relatively well-off people can use their personal resources to protect themselves against tend to get short shrift.
This chapter discusses public health law as a tool for adapting to the infectious disease impacts of climate change. In Section 9.2, I discuss how climatic conditions are affecting interactions between the agents, vectors, and hosts of disease within our changing environment, leading to changing patterns of vector-borne, zoonotic, food-borne, and waterborne illness. Section 9.3 focuses on the public health law toolkit for infectious disease control, including laws that facilitate surveillance, access to medical countermeasures, vector control, health education and communication, social distancing, and public health emergency preparedness and response. In Section 9.4, I introduce two principles that should guide adaptation to the infectious disease impacts of climate change: One Health and Health in All Policies. Finally, I offer some concluding reflections on the potential influence of climate change adaptation on the development of public health law and policy.
9.2 Infectious Disease Risks Associated with Climate Change
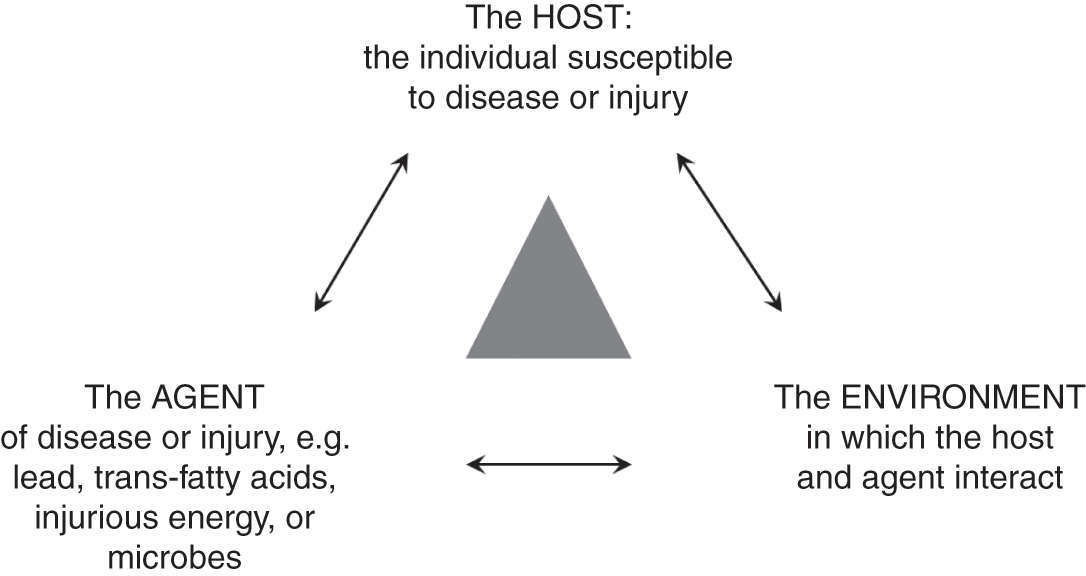
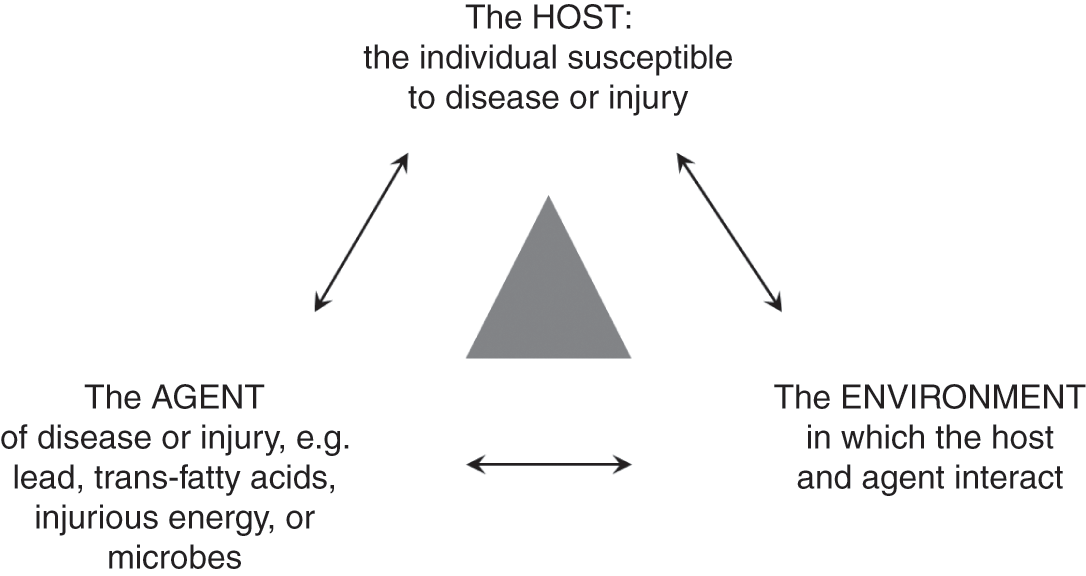
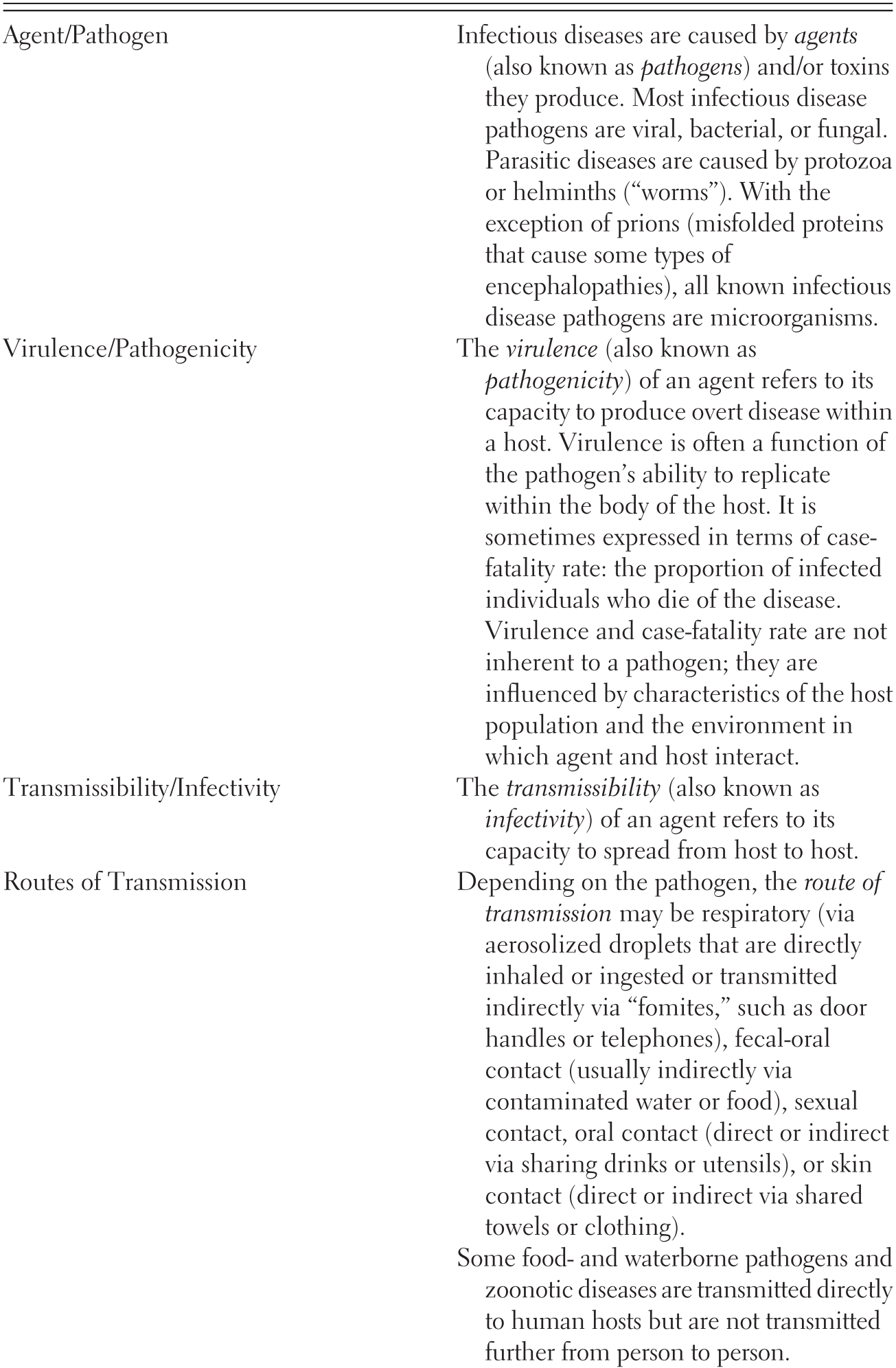
Epidemiologists describe patterns of infectious disease as being produced by the interaction between the agent of disease or pathogen (viruses, bacteria, fungi, protozoa, helminths, or prions) and the host (the somewhat eerie scientific term used to describe the infected individual) within an environment (broadly defined so as to include social, economic, and cultural factors in addition to features of the built and natural environment).Footnote 2 Vectors may mediate the relationships among host, agent, and environment (see Figure 9.1). Experts typically categorize infectious diseases in terms of type of agent (e.g. viral, bacterial, fungal, and parasitic diseases), the infectivity and transmissibility of the pathogen within a specified host population under specified environmental conditions, and the routes by which it is transmitted. Table 9.1 provides definitions for these and other key terms.
| Agent/Pathogen | Infectious diseases are caused by agents (also known as pathogens) and/or toxins they produce. Most infectious disease pathogens are viral, bacterial, or fungal. Parasitic diseases are caused by protozoa or helminths (“worms”). With the exception of prions (misfolded proteins that cause some types of encephalopathies), all known infectious disease pathogens are microorganisms. |
| Virulence/Pathogenicity | The virulence (also known as pathogenicity) of an agent refers to its capacity to produce overt disease within a host. Virulence is often a function of the pathogen’s ability to replicate within the body of the host. It is sometimes expressed in terms of case-fatality rate: the proportion of infected individuals who die of the disease. Virulence and case-fatality rate are not inherent to a pathogen; they are influenced by characteristics of the host population and the environment in which agent and host interact. |
| Transmissibility/Infectivity | The transmissibility (also known as infectivity) of an agent refers to its capacity to spread from host to host. |
| Routes of Transmission | Depending on the pathogen, the route of transmission may be respiratory (via aerosolized droplets that are directly inhaled or ingested or transmitted indirectly via “fomites,” such as door handles or telephones), fecal-oral contact (usually indirectly via contaminated water or food), sexual contact, oral contact (direct or indirect via sharing drinks or utensils), or skin contact (direct or indirect via shared towels or clothing). |
| Some food- and waterborne pathogens and zoonotic diseases are transmitted directly to human hosts but are not transmitted further from person to person. | |
| Vector-borne disease | Vector-borne diseases are transmitted via a vector organism (e.g. mosquito, tick, or rodent) that carries the pathogen from person to person. |
| Zoonotic disease | Zoonotic diseases are transmitted from an animal to a person. An infected animal becomes an intermediary host. An animal population susceptible to a pathogen that is transmissible to humans is sometimes referred to as an animal reservoir of disease. It is difficult to control zoonotic disease within a human population if the disease remains present in an animal reservoir. In some cases, a disease first emerges within an animal population and then develops the capacity to be transmitted from animal to person. |
| Waterborne disease | Waterborne diseases are caused by pathogens that live in contaminated water, which the human host ingests. They may be deposited in water by infected humans or animals. |
| Water-related disease | Water-related diseases encompass waterborne diseases as well as water-washed diseases (those that are transmitted easily from person to person in the absence of good hygiene practices) and some vector-borne diseases (those transmitted by vector organisms that are affected by how wet or dry the climate is). |
| Food-borne disease | Food-borne diseases are caused by pathogens that live in contaminated food, which the human host ingests. They may or may not also be transmissible from person to person. |
| Endemic | The endemic level of a disease refers to its usual prevalence in a given geographic area. A disease is endemic to an area if it is steadily present there. |
| Outbreak | A disease outbreak occurs when a disease is present in greater numbers than expected in a given place during a given time. |
| Epidemic | An infectious disease epidemic occurs when a disease spreads rapidly to many people. |
| Pandemic | A pandemic occurs when an epidemic has spread across a wide region of the globe. |
Climate change is expected to change the geographic and seasonal distribution of a wide range of infectious diseases.Footnote 3 Pathogens, vector organisms, and intermediary animal hosts are all living organisms. They typically depend on particular environmental, climatic and weather conditions to support the various stages in their lifecycle.Footnote 4 Climate-related factors can affect the number and type of pathogens, vector organisms, and animal hosts in any given geographic area. These factors can also affect the virulence and transmissibility of many pathogens. Globally, epidemiologists estimate that about half of all vector-borne disease risk and 94 percent of diarrheal illness risk is attributable to modifiable environmental factors.Footnote 5 For example, higher average temperatures or rainfall can create more favorable breeding conditions for a vector population like mosquitos, increasing the risk that they will transmit diseases like Zika virus and West Nile virus to humans living in the area. Patterns of alternating drought and flooding can cause waterborne pathogens like cholera to become concentrated in small pools of water during times of drought before being washed into larger bodies of water (where people get their drinking water, wash their clothes, or play) during periods of flooding. An animal reservoir population may be weakened by malnutrition or loss of habitat, creating ripe conditions for the emergence of a new zoonotic disease, such as Ebola virus. Changes in the natural environment – whether caused by climate change, deforestation, desertification, or any combination of human-caused or natural processes – also affect the social, economic, cultural, and built environments. The impacts of climate change on food and water security, natural disasters, and national security could also make human populations more vulnerable to infection as a result of social, economic, and cultural instability, degradation of the built environment, and malnutrition.
The effects of climate change on the natural environment vary from region to region. Some places become more arid, others become wetter. Many experience both extremes – drought and flooding – more frequently. Many places become warmer while some experience greater extremes of hot and cold temperatures. In many places, weather patterns are less stable, with unseasonable conditions occurring more frequently. In many cases, climate change will redistribute weather patterns, causing vector and reservoir populations to move to higher or lower altitudes or latitudes. Weather conditions and landscape features can generate highly localized patterns of infectious disease transmission.Footnote 6 The result may be a reduction in endemic infectious diseases for some regions and increases in others, shifts in the seasonal distribution of outbreaks, and increased risk of emerging infectious diseases with pandemic potential.Footnote 7
9.2.1 Vector-borne
Vector-borne diseases, especially mosquito-borne diseases, are highly sensitive to environmental changes.Footnote 8 Globally, climate change is expected to expand the geographic and seasonal range of mosquito-borne illness while also shifting it in some places. For example, mosquitoes may be able to thrive at higher altitudes – where temperature and moisture conditions were previously inhospitable to mosquitoes. This is concerning because infectious disease outbreaks tend to be more pathogenic when they occur in a population that has not previously experienced much exposure to the disease.Footnote 9 If the southeastern United States were to experience a rapid increase in Dengue fever, for example, we would expect to see higher rates of morbidity and mortality because only a small percentage of the population (those who have resided or traveled in areas where Dengue is endemic) will have previously been exposed. Other mosquito-borne diseases that may be affected by climate change include malaria, Zika virus, West Nile virus, and chikungunya.Footnote 10 Hantavirus (transmitted by rodents) and Lyme disease (transmitted by ticks) are also sensitive to changing weather patterns.Footnote 11 There is also a risk that changing climatic conditions could create opportunities for the emergence of new vector-borne diseases.Footnote 12
9.2.2 Zoonotic
Diseases that can be spread from animals to people, known as zoonotic diseases or zoonoses, are also highly sensitive to environmental changes that alter the habitats of animal populations and bring them into closer contact with human populations. The most pathogenic infectious diseases that emerged in the late twentieth century – HIV, Ebola virus, and avian influenza – began with animal to human transmission before the pathogens became transmissible from person to person. Newly emerging zoonotic diseases warrant particular concern because of the risk that they will become efficiently transmissible from person to person before effective medical countermeasures can be developed and disseminated. Any infectious disease that can thrive in an animal reservoir population is extremely difficult to eradicate. Smallpox, the only infectious disease to be successfully eradicated, was a relatively simple target in part because it lacked an animal reservoir. Poliovirus and measles are similarly attractive targets for eradication because they, too, lack an animal reservoir (though they are less susceptible to eradication because unlike individuals infected with smallpox, who exhibit visible signs of disease during the entire period in which they are contagious, those infected with polio and measles are contagious prior to the onset of visible symptoms).Footnote 13 In contrast, Ebola virus continues to circulate in animal populations between outbreaks in human populations, making it virtually impossible to eradicate even after an effective vaccine becomes widely available.Footnote 14
9.2.3 Food-borne
Epidemiological studies have documented that warmer temperatures are associated with an increased likelihood of food-borne disease outbreaks.Footnote 15 Warmer temperatures promote proliferation of pathogens in hospitable food items. Additionally, higher average ocean surface temperatures combined with increased runoff from sewage systems create favorable conditions for bacteria, increasing the risk of contaminated seafood.Footnote 16 Warmer conditions at facilities for agricultural production, livestock processing, and food manufacturing and packaging could also increase the risk of food-borne illness.Footnote 17
9.2.4 Waterborne
Changes in moisture and patterns of drought and flooding affect a number of diseases carried by water.Footnote 18 Some water-related illnesses sensitive to climatic conditions, such as those caused by toxin-producing algae, are not technically infectious.Footnote 19 Others, such as cholera, are highly virulent and pathogenic bacterial infections. The risk of giardiasis, which is caused by a parasite typically deposited in water by infected small mammals and then ingested by humans, is also linked to climate change. Rising surface water temperatures may also increase the risk of acquiring infectious illnesses through swimming and other water sports.Footnote 20
Many waterborne diseases sensitive to climate are exacerbated by increased agricultural run-off. Nitrogen and phosphorous, common fertilizer ingredients, create ripe conditions for harmful algae blooms in bodies of water near or downstream from concentrated agricultural operations, posing a risk to bathers who inadvertently ingest water when they swim or contract skin infections, in addition to posing a risk of food-borne illness for those who consume contaminated shellfish. Concentrated animal confinement facilities can also contribute to contamination of ground and surface water, increasing the prevalence of infectious agents that have developed resistance to antibiotics commonly used at subtherapeutic doses in animal feed for growth promotion purposes.Footnote 21
When infrastructure crumbles – because of a natural disaster, state collapse, or some combination of the two – water-related disease outbreaks soon follow. Cholera in particular is the characteristic disease indicator of a failing state.Footnote 22 Cholera and other diarrheal illnesses are especially sensitive to breakdowns in basic sanitation infrastructure for the removal of human waste, as seen in Haiti following an earthquake in 2010. Because climate change stresses governments, economic systems, and infrastructure, it heightens the probability of social failures that lead to disease outbreaks, even as it also makes environmental conditions more hospitable for the spread of disease.
9.3 Public Health Law Tools for Adapting to the Infectious Disease Impacts of Climate Change
Climate change will make the work of “ensur[ing] the conditions required for people to be healthy”Footnote 23 considerably more challenging in coming decades. Although public health law has broadened its scope to encompass noncommunicable disease threats and injuries, the law of infectious disease control remains at its core. As policymakers seek to adapt to the health consequences of climate change they are turning to legal frameworks, human resources, and technical infrastructure devoted to public health surveillance, development of and access to medical countermeasures, vector control, health education and communication, social distancing, and public health emergency preparedness and response.
9.3.1 Surveillance
Responding effectively to infectious disease threats requires good information. Public health authorities conduct continuous and systematic surveillance to monitor outbreaks in human and animal populations.Footnote 24 Laws mandate that healthcare providers, laboratories, and other parties report individual cases of disease to health department registries. Case reports may trigger epidemiological investigations to identify the source of an outbreak. Analysis and interpretation of case reports and diagnostic test results also inform planning, policy formation, and evaluation of public health interventions.Footnote 25 Surveillance will be particularly important to ensure detection and tracking of gradual changes in the geographic and seasonal distribution of infectious disease as a consequence of climate change.
Rapid detection and response to infectious disease outbreaks is a global priority. In response to concerns about pandemic influenza, the World Health Assembly adopted revised International Health Regulations (IHR) in 2005, which obligate member states to ensure adequate infrastructure to detect infectious disease threats with potential for international spread.Footnote 26 Lack of adequate resources has resulted in the majority of member states failing to satisfy IHR requirements. In 2014, only sixty-four member states reported that they were in full compliance, while eighty-one requested an extension and forty-eight failed to file a report.Footnote 27 Full implementation and strengthening of the IHR, with an eye toward the health impacts of climate change, should be a global health and climate adaptation priority.
Surveillance raises concerns about health information privacy. An infectious disease diagnosis may affect an individual’s employment, personal relationships, and other aspects of life. Much of public health law with respect to surveillance systems is aimed at balancing between collective needs for accurate, traceable information to inform disease control efforts and individual interests in the privacy, confidentiality, and security of sensitive information.Footnote 28 Public health information infrastructure, and the regulatory regimes that govern it, which are discussed in Chapter 6 of this volume, are crucial to climate adaptation.
9.3.2 Access to Effective Medical Countermeasures
Medical countermeasures – including vaccines and antimicrobials – are powerful tools for preventing and treating infections and controlling the spread of communicable diseases associated with climate change. Because the market typically fails to provide adequate incentives to develop and produce vaccines and antimicrobials, law plays a role in promoting the development of new countermeasures, ensuring their safety, and securing appropriate access.Footnote 29
In addition to mechanisms designed to encourage private investment and provide direct public investment in research and development of countermeasures for routine medical needs, the United States has adopted special measures to encourage development of new countermeasures for biological agents determined by the Department of Homeland Security to pose a material threat. Some of the targeted agents, such as Ebola, are climate-sensitive. For example, the Biomedical Advanced Research and Development Authority (BARDA), part of the U.S. Department of Health and Human Services, awards grants to private firms to assist with clinical trials and the development of manufacturing capacity to produce new vaccines, treatments, and diagnostic tools for public health emergencies.Footnote 30
The countermeasures successfully developed with public investment are often stockpiled in government facilities for rapid deployment in response to a public health emergency. In an emergency, an official declaration following prescribed procedures may also trigger exceptions or enhanced flexibility with respect to legal requirements designed to ensure the safety of drugs, vaccines, and medical devices.Footnote 31 An emergency may also necessitate the development and implementation of protocols for rationing scarce medical resources.Footnote 32
Most of the population is ready and willing to take advantage of medical countermeasures. In rare cases, however, individuals prefer to decline recommended vaccinations and treatment, due to distrust of government and scientific recommendations or unwillingness to accept the risks associated with vaccination, particularly when the benefits of herd immunity accrue to the community at large. In the United States, vaccination laws are focused primarily on ensuring that children are vaccinated for several preventable communicable diseases prior to entering school.Footnote 33 These provisions are regularly challenged in court on a variety of constitutional grounds, including First Amendment protection of religious freedom and Fourteenth Amendment substantive due process rights to bodily integrity and decisional privacy. Judges have consistently upheld school vaccination requirements, holding that the Due Process Clause does not protect a fundamental right of a parent “to refuse to have her child immunized before attending public or private school where immunization is a precondition to attending school.”Footnote 34 Additionally, courts have consistently held that compulsory vaccination laws, which are laws of general applicability and do not target particular religious groups or views, need not allow for religious exemptions to be constitutional.Footnote 35 Adult vaccination mandates are rare, though many institutional healthcare providers (e.g. hospitals and long-term care facilities) have adopted policies requiring employees to be vaccinated.Footnote 36 Mandatory vaccination may be particularly fraught in an emergency context, when vaccines may be recently developed under loosened safety requirements. Dicta in the Supreme Court’s landmark opinion in Jacobson v. Massachusetts (upholding a compulsory smallpox vaccination law applicable to adults as well as children) suggests that a compulsory vaccination law that made no exception for medical contraindications (such as an allergy or immune deficiency) would probably run afoul of the Fourteenth Amendment.Footnote 37 As a matter of balancing state interests against individual rights, however, a public health emergency (such as the frequent smallpox outbreaks during Jacobson’s time or the outbreak of a novel infectious disease associated with changing environmental conditions) justifies more intrusive measures than maintenance of community immunity against more routine threats, such as measles.
Coercive government measures are rarely needed to compel compliance with recommended medical treatment because most individuals who are actually or potentially infected desire treatment. Where a patient is unwilling or unable to comply with treatment recommendations, however, health officials (primarily at the state and local level) may order compulsory treatment, including under conditions of confinement.Footnote 38 Although the US Supreme Court has recognized a constitutionally protected liberty interest in refusing unwanted medical treatment in cases involving abortion, terminal illness, and mental illness, it has not directly addressed the question of what the Fourteenth Amendment requires for confinement of individuals who are actually or potentially infected with a contagious disease. The lower courts have relied heavily on cases reviewing civil commitment of individuals with mental illness, which balance individual liberty against state interests by requiring a showing that the individual poses a danger to himself or others, that treatment is in the individual’s medical interest, and that the medication is administered by a licensed physician acting in accordance with professional standards.Footnote 39 Additionally, treatment must be necessary to significantly further important government interests in light of less intrusive alternatives.Footnote 40 The Fourteenth Amendment also protects the patient’s right to due process to ensure that confinement or conditional release is warranted on a case by case basis.Footnote 41 These standards may prove problematic in cases where a treatment is new and its effectiveness is unproven, such as with an emerging zoonotic disease like Ebola. On the other hand, lack of effective medical countermeasures heightens the state’s interest in controlling the spread of disease, which would probably justify confinement, as discussed in the section on quarantine and isolation.
Compulsory application of effective medical countermeasures may be justified by the harm principle. Although we tend to conceive of vaccination and medical treatment in terms of their benefit to the infected individual, medical countermeasures also play a crucial role in slowing the spread of disease from person to person. When immunization levels are sufficiently high, outbreaks are quickly contained because there are too few vulnerable hosts for the pathogen to spread beyond a small number of individuals.Footnote 42 Similarly, antimicrobials typically reduce or eliminate a patient’s ability to infect others.Footnote 43 In some cases, compulsory treatment may be necessary to ensure that the full course of treatment is completed, thus reducing the risk that the pathogen will develop resistance as a consequence of being exposed to subtherapeutic doses of medication.Footnote 44
Antimicrobial resistance is a mounting global health crisis. In addition to inappropriate use in human populations, the administration of subtherapeutic levels of antibiotics in animal feed as a growth-promotion strategy contributes to the evolution and transmission of resistant strains.Footnote 45 Regulation of veterinary use of antibiotics and industrial farming practices is thus crucial to maintaining the efficacy of available countermeasures. Unfortunately, and in spite of efforts by advocates and policymakers, such regulation has not been forthcoming in the United States.
Market forces privilege development of pharmaceuticals that can sustain routine use by a significant population of patients who can afford expensive treatment. Public health emergency preparedness programs like BARDA have prioritized countermeasures for agents with the potential to be weaponized by terrorists or enemy states. Investment in countermeasures for infectious diseases that disproportionately burden the world’s poorest people has been paltry by comparison. Some of these historically neglected diseases, such as malaria, Zika virus, and Ebola virus, are particularly sensitive to changing environmental conditions. Climate change, by exacerbating health threats that disproportionately affect less privileged populations, is likely to expose longstanding injustices in health investment and governance.Footnote 46
9.3.3 Isolation, Quarantine, and Social Distancing
For some infectious agents, such as Ebola virus in 2014–2015 and Zika virus in 2015–2016, effective medical countermeasures like vaccines and antivirals are limited or entirely unavailable. Under these circumstances, particularly if the agent is highly infectious and virulent, it may be necessary to isolate infected individuals, quarantine those who have been or may have been exposed, and implement measures to limit social contact among the population at large. Even in cases where medical countermeasures are being used, these tools may be useful to limit the spread of disease during the treatment period.
Like compulsory vaccination and treatment, these tools implicate individual rights to liberty, bodily integrity, and autonomy. They are understandably controversial and are hotly debated by lawmakers, health officials, and judges, who must balance individual rights against collective needs – and demands – for health security. Under emergency conditions, political considerations and public panic may come into play. In Mayhew v. Hickox, for example, a Maine court enjoined state health authorities from enforcing travel restrictions on a nurse who had recently returned from treating patients infected with Ebola virus in West Africa.Footnote 47 The court’s order urged the nurse to respect public concerns, even while recognizing that those concerns were based on a misunderstanding of the actual risk posed by individuals who may have been exposed to Ebola virus but had not yet developed any symptoms of disease.
In the United States, most states have granted authority to health officials to initiate isolation and quarantine under routine circumstances on a case by case basis.Footnote 48 In some states, these statutes are limited to specified conditions, such as tuberculosis, requiring officials to reinvent the wheel when presented with a novel infectious disease outbreak. In other states, the statutes are drafted more broadly, allowing officials and courts greater flexibility. Most states also have special emergency procedures, which may grant health officials broader isolation and quarantine authority during a declared emergency. Federal isolation and quarantine authority is limited to prevention of international and interstate spread of disease, though new federal quarantine regulations released in early 2017 after a lengthy effort to modernize the rules governing federal authority for quarantine, isolation, and conditional release to prevent the interstate spread of communicable diseases take a fairly broad approach to determining when the risk of interstate transmission warrants federal involvement.Footnote 49 Virtually identical provisions apply to people arriving in the United States from foreign countries.Footnote 50
Government authority to isolate the sick, quarantine the exposed, and enforce social distancing for those at risk of exposure is particularly relevant to the potential emergence of new pathogens with pandemic potential. If, as some experts warn, climate change will increase the rate at which new pathogens emerge, legal authorities that permit infringement of individual liberty in the interest of collective needs to contain the spread of disease will continue to be tested.
9.3.4 Vector Control
For diseases carried from host to host by insects or rodents, vector control activities are a crucial component of infectious disease prevention. Fumigation with insecticides sprayed by trucks and airplanes is the most visible form of vector control, but other methods – including the treatment of breeding areas with larvicides – play a more important role in controlling the mosquitoes most likely to spread disease. Removal of standing water where mosquitoes may lay eggs and land use plans that divert human settlements away from high-risk breeding areas are also important strategies.
In the United States, vector control is conducted primarily by local government authorities, often organized through special vector control districts.Footnote 51 Federal regulations under the Federal Insecticide, Fungicide and Rodenticide Act (FIFRA) govern appropriate use of specific insecticides and larvicides. Past outbreaks of West Nile virus and Zika virus in the United States have spurred disputes between local authorities and citizen groups concerned about the potential harmful effects of spraying. In No Spray Coalition v. City of New York, for example, an environmental and public health advocacy group sought to enjoin the city’s pesticide use in response to an outbreak of West Nile virus.Footnote 52 After the courts dismissed the Coalition’s claim under other city, state, and federal environmental protection statutes, a federal district court ruled that its claim under the federal Clean Water Act (CWA) survived summary judgment because pesticide spraying near bodies of water might constitute discharge of a pollutant under the CWA. The city then agreed to pay $80,000 to five environmental protection nonprofit organizations, cover the plaintiffs’ legal fees, and hold two three-hour meetings between the city’s Department of Health and Mental Hygiene and the plaintiffs to discuss “health and environmental concerns pertaining to … pesticides and proposals for alternative and non-toxic approaches.”Footnote 53 No Spray Coalition continues to express concern about the potential health effects of pesticides, distrust for government-sponsored scientific assessments of risks and benefits, and preference for “natural” approaches to mosquito control using essential oils.Footnote 54
9.3.5 Food and Animal Safety
Enforcement of sanitary agricultural, livestock processing, and food manufacturing practices is essential to the prevention of zoonotic and food-borne illness. Controlling the spread of zoonotic and food-borne illness sometimes requires destruction of infected animals (e.g. poultry, hogs) and contaminated products (e.g. grain). In other cases, products may need to be diverted to markets for uses other than human consumption, reducing their value (e.g. farmers may be limited to selling salmonella-contaminated eggs on the “breaker” market where they are used for limited purposes). Compensation of property owners could be prohibitively expensive. In the United States, courts have determined that compensation may be constitutionally required (under the Takings Clause) where uninfected animals are destroyed (e.g. for testing purposes), but not for diseased animals.Footnote 55 Food safety and agricultural regulations may also provide for compensation, but these statutory provisions may be waived in the case of a declared emergency.Footnote 56
9.3.6 Health Education and Communication
Many infectious disease risks can be managed, at least in part, through protective individual behaviors. Health departments at every jurisdictional level – as well as departments with responsibility for other sectors, such as fishery management and recreation – play a role in developing and disseminating educational materials and public messages. Local authorities, for example, issue warnings urging individuals to avoid exposure to water and shellfish from designated areas due to recognized infectious disease risks. Health communication strategies also target specific groups, such as healthcare workers, to urge them to adopt more rigorous hand hygiene practices when working with patients in settings that are ripe for the spread of antibiotic-resistant strains of bacteria. Vector-control authorities also rely on communication strategies to inform residents about the need to survey their homes and property for small amounts of standing water (e.g. in potted plants, open containers outdoors) that might become breeding sites for mosquitoes. (See also Chapter 4).
9.4 Health Governance Principles for Adapting to the Infectious Disease Impacts of Climate Change
Public health law frameworks are supplemented and informed by a wide range of policy principles. Two of these have particular relevance to the infectious disease impacts of climate change: One Health and Health in All Policies. These principles seek to overcome the challenges posed by the traditional division of social, economic, and environmental programs into distinct silos, each with its own mandates, expertise, and organizational structure. One Health promotes intersectoral work among agencies and experts focused on human health, animal health, agriculture, and the natural environment. Health in All Policies seeks to integrate public health goals into the work of all sectors – those focused on the natural environment, animal health, and agriculture, as well as transportation, built environment, economic development, national security, and more.
9.4.1 “One Health”
Global health, veterinary medicine, agriculture, environmental protection, and other experts are coming together to promote the principle that animal health, human health, and environmental health are interconnected in reality and policy efforts to protect them should also be joined up (see Figure 9.2).Footnote 57
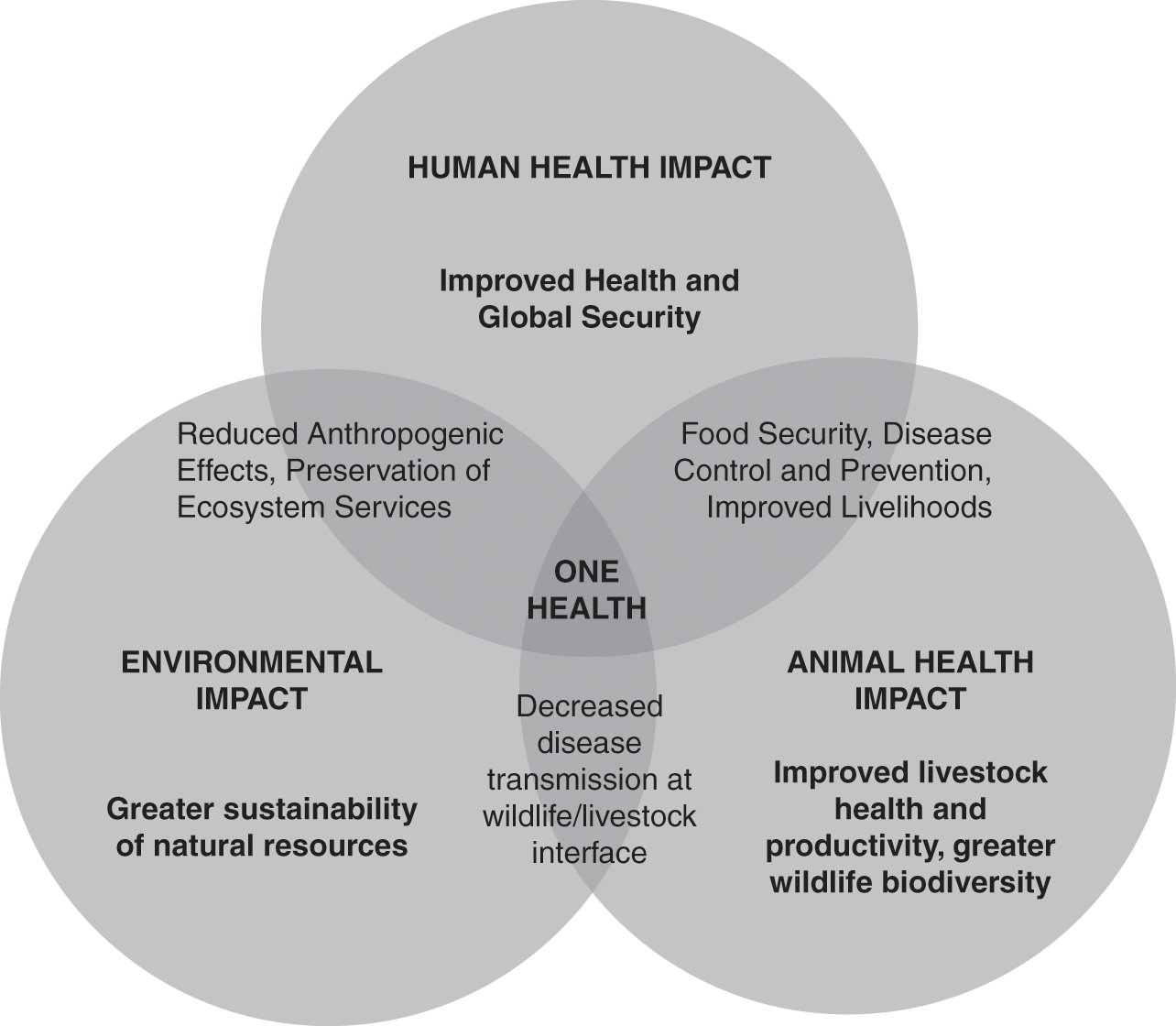
Figure 9.2 Thematic representation of One Health depicting potential added benefits of sectoral overlap.
The One Health principle has increased engagement between government agencies responsible for environmental, animal, and human health. In the United States, for example, the Centers for Disease Control and Prevention hosts a National Center for Zoonotic, Vector-Borne, and Enteric Diseases. The center draws on the expertise of dozens of on-staff veterinarians, who support surveillance, epidemiological investigation, and response efforts. Other federal agencies also combine veterinary and human health expertise to inform pandemic and bioterror preparedness efforts.Footnote 58
At the international level, the World Health Organization, Food and Agriculture Organization of the United Nations, and the World Organization for Animal Health coordinate their work on food safety and zoonotic diseases, as well as “other public health threats at the human-animal-ecosystem interface.”Footnote 59 Commentators note that these efforts are characterized by “general enthusiasm” but that advocates are struggling to “translate theory into action.”Footnote 60 Furthermore, these efforts have focused narrowly on diseases with pandemic potential, such as highly pathogenic avian influenza and severe acute respiratory syndrome (SARS), leaving other threats neglected.Footnote 61 To have a meaningful impact on climate change adaptation, One Health will require greater investment in infrastructure and human resources to hire and train staff across multiple areas of expertise.
9.4.2 “Health in All Policies”
The Health in all Policies principle reflects growing recognition that many of the determinants of population health are governed by laws and policies developed and implemented in nonhealth sectors.Footnote 62 It recognizes that responding effectively to public health threats often requires integrated, whole-of-government approaches, with lawmakers and government officials from multiple sectors working to harmonize their goals and strategies for achieving them.Footnote 63
Lawmakers in several countries across Asia and Europe have translated the Health in All Policies principle into a legal requirement that agencies conduct health impact assessments (HIAs) as part of the regulatory process. Some also require private commercial entities to assess the likely health impact of proposed infrastructure projects. (See Chapter 14.)
In other cases, policymakers and judges have incorporated consideration of health impacts into broader requirements for regulatory impact assessment. For example, in Association of Irritated Residents v. San Joaquin Valley, a California state court required a local air pollution district that encompasses eight counties to reassess a proposed regulation of confined animal agricultural facilities in light of anticipated impacts on public health, pursuant to a state statutory directive.Footnote 64
Health impact assessments are appealing from a common sense standpoint, but they face many challenges in practice. Affected industries and organizations may deploy financial resources and political capital to oppose implementation of health impact assessments as a legal requirement. As a procedural exercise, HIAs run the risk of becoming one more in a series of bureaucratic hurdles that slow down, but fail to otherwise influence, development projects. Evaluating their effectiveness requires careful analysis of whether and how HIA recommendations are accepted and implemented and whether the aims and objectives of the HIA were ultimately served by the procedural requirement.Footnote 65
9.5 Conclusion: Challenges and Opportunities
Responding to the infectious disease impacts of climate change presents multiple challenges and opportunities.Footnote 66 The infectious disease and other impacts of climate change are occurring in the midst of an ongoing transformation in public health law. Two key shifts in the scope and nature of public health law are particularly significant for climate change adaptation. First, the shift toward increasing integration between the public health and healthcare sectors. Second, the shift away from the behavioral model of public health that held sway among scientists and practitioners during the second half of the twentieth century and toward the social-ecological model, which is now favored by scientists but has encountered cultural, political, and legal resistance. Both of these shifts have implications for longstanding tensions in public health law and governance between individual interests and collective needs and between personal responsibility and public responsibility for health.
9.5.1 Integration of the Public Health and Healthcare Sectors
To the extent that responding to the infectious disease impacts of climate change prompt public health authorities and healthcare providers to better define channels of communication, while also giving healthcare providers a greater stake in protecting environmental and animal health, adaptation may also reinforce an ongoing shift toward greater integration between the public health and healthcare sectors. In the United States, for example, budgetary crises have led to stagnating or declining investments in public health infrastructure,Footnote 67 prompting public health advocates to take a greater interest in partnering with better-financed healthcare providers.Footnote 68 At the same time, tax and health care reimbursement incentives are giving healthcare providers a greater financial stake in patient outcomes and population-level drivers of disease and injury. In the context of a changing climate, these incentives could also prompt providers to take a more active interest in protecting the environment.
This integration presents opportunities to better serve healthcare and public health goals alike, but it also presents challenges. Public health advocates worry that the better financed and politically favored healthcare sector, with its emphasis on downstream treatment strategies (e.g. new drugs for malaria) will overwhelm the public health sector, with its emphasis on upstream prevention strategies (e.g. vector control and community siting strategies to minimize exposure to disease-carrying pests).Footnote 69
9.5.2 Controversy over the Social-Ecological Model of Health
To the extent that climate change adaptation activities provide a forum for advancing One Health, Health in All Policies, and integration of the public health and healthcare systems as general principles for health governance, they could reinforce an ongoing shift toward the social-ecological model of health. For most of the twentieth century, infectious disease control strategies relied principally on the agent model of disease. The agent model focused attention on combatting disease with agent-specific countermeasures (i.e. vaccines and antimicrobials). In the late twentieth century, policymakers and public health practitioners began to apply the behavioral model (which arose in response to noncommunicable disease threats) to infectious disease threats as well. The behavioral model shifted the focus from the agents of disease to the behaviors of human hosts. It emphasized health communication and education as key interventions, putting the onus on individuals to reduce risky behaviors (e.g. tobacco use, raw shellfish consumption) and adopt protective behaviors (e.g. condom use, mosquito repellant use). In contrast, the social-ecological model that emerged around the end of the twentieth century emphasizes the environments – physical, social, economic, etc. – in which the host and agent interact. It points policymakers toward structural, community-level interventions to create healthy living conditions, rather than relying predominantly on clinical interventions that target discrete agents of disease or behavioral interventions that focus on individual choices.
The social-ecological model is favored by most public health scientists for its descriptive power and normative thrust. It is also particularly well suited for adaptation to the health impacts of climate change, the scale and scope of which defy the technological solutionism that characterizes the agent model of health (e.g. medical countermeasures tailored to combat specific climate-sensitive pathogens) and the emphasis on individual responsibility to avoid health hazards (e.g. advising individuals to avoid shellfish) that characterizes the behavioral model of health. The social-ecological model is broad enough to encompass deployment of medical countermeasures and behavioral interventions while also digging deeper to examine the structural, social, and environmental determinants that shape access to and use of medical countermeasures, acceptance (or nonacceptance) of scientific and government advice, and many other factors such as urban planning and community resilience. Yet the social-ecological model faces many challenges. The behavioral model, with its individualistic orientation toward behaviors and choices, is a better fit for most people’s intuitive understanding of health as a primarily personal concern. The agent model, with its focus on medical countermeasures that allow private pharmaceutical companies to capture the benefits of public investment, enjoys political favor. In contrast, the social-ecological model more frequently points policymakers toward public investments that are not easily captured by politically powerful private interests (e.g. sanitation systems, infrastructure to support surveillance and epidemiological investigation) and toward regulation of private commercial activities (e.g. pollution controls).
9.5.2.1 Tension between Individual and Collective Rights and Responsibilities
At the heart of both of these shifts – toward increased integration between public health and healthcare and toward the social-ecological model of health – is an intractable tension between individual interests and collective needs and between personal and public responsibility for health. Do individuals bear primary responsibility for avoiding exposure to mosquitoes and other disease-carrying pests or should pest control be publically financed? Should a minority of individuals who oppose the use of pesticides (e.g. because they do not trust the safety assurances of government scientists) be able to block public vector control efforts? Is it the responsibility of individuals who rely on local bodies of water for recreation and fishing to find alternatives, or is there a public responsibility to ensure that bodies of water and the animals that inhabit them are safe? Should individual property owners be barred from using their land in ways that contribute to water contamination? Why should governments stockpile influenza drugs to be distributed in case of emergency while allowing many who need HIV drugs to go without?
In theory, infectious disease threats are the paradigmatic example of why collective needs must sometimes outweigh individual rights and collective action is sometimes the only mechanism by which individuals may protect themselves. The US Supreme Court famously articulated these principles in Jacobson v. Massachusetts, in which it rejected the notion that an individual’s right to refuse vaccination trumps the community’s need to protect itself from a smallpox epidemic.Footnote 70 In practice, however, many forces still resist the notion that infectious disease threats justify infringement of individual rights (e.g. to bodily integrity, property, and autonomy) and trigger an obligation to provide mutual aid (e.g. through collective mechanisms to finance development and deployment of public health infrastructure, medical countermeasures, and healthcare services).
The vector-borne and diarrheal illnesses that are likely to be exacerbated by climate change have long been neglected by collective financing and health governance mechanisms at the international, domestic, and local levels. Governmental and nongovernmental investments in global health have tended to privilege threats such as influenza pandemics that spread rapidly across borders and affect the wealthy alongside the poor. These investments are typically justified as a form of “enlightened self-interest” in light of the notion that “disease knows no borders” and so the resources of wealthy states are well-spent containing disease threats at their point of origin, even if that means building infrastructure in far-flung places. Climate-sensitive diseases tend to serve as counter-examples to this well-worn trope. In fact, one could map cases of Dengue fever, cholera, and other illnesses that impose extraordinary burdens on human health and wellbeing and easily identify borders between governmental jurisdictions. Public spending on health infrastructure matters. Economic opportunities, which enable a higher standard of living, matter. Climate change threatens to exacerbate the unconscionable health disparities that have long plagued human society. If we rise to the challenges posed by the health impacts of climate change by investing in basic public health infrastructure and human resources, promoting intersectoral collaboration, and privileging upstream, social-ecological interventions over downstream interventions that put the onus on individuals to change their behaviors and rely on expensive and reactive clinical treatments, our world will be better for it. Failure, on the other hand, would be unsurprising in light of the history of health governance.