Introduction
Foreign body airway obstruction (FBAO) is a life-threatening emergency. In the United States, approximately 5,000 patients die every year from FBAO, making it the fourth most common cause of unintentional death. Reference Miller1 Japan has a particularly high incidence of FBAO, likely due to its aging population and unique food culture, with over 8,000 deaths every year, making it the second most common cause of unintentional death. 2 Although FBAO occurs in all age groups, it is the leading cause of mortality and morbidity in infants and older adults, making it a significant public health challenge world-wide.
Foreign body removal should be performed as soon as possible before cardiac arrest occurs. Reference Olasveengen, Mancini and Perkins3,Reference Olasveengen, Mancini and Perkins4 When bystanders successfully removed the foreign body, the neurologically favorable rate was 74%, but it was 32% when removed by the Emergency Medical Services (EMS) at the scene, and only 10% when removed by doctors after arrival at the hospital. Reference Igarashi, Yokobori, Yoshino, Masuno, Miyauchi and Yokota5 Thus, the prognosis is greatly affected by the prehospital process; however, there are few large-scale studies on the characteristics of patients, interventions, and outcomes. Reference Olasveengen, Mancini and Perkins3,Reference Olasveengen, Mancini and Perkins4
Therefore, using EMS activity logs, this study aimed to evaluate whether the characteristics of patients with FBAO are associated with prehospital factors affecting outcomes in order to support policymakers in developing an intense prevention plan and provide suggestions to the fire department and medical personnel on strategies to improve outcomes in patients with FBAO.
Methods
Study Design
This was a retrospective, observational study. All EMS activities were routinely recorded. The extracted data were anonymized; hence, patient consent was waived by the ethics committee. The study protocol was approved by the appropriate ethics committee.
Setting
Patients who were transferred by the Tokyo, Japan Fire Department for FBAO from January 1, 2017 through December 31, 2019 were included in this study. Tokyo is the largest city in Japan, and the Tokyo Fire Department is a public agency that provides EMS to most cities, covering a population of approximately 15.82 million during the day and 13.52 million at night and an area of 1,761 km2. 6
Inclusion/Exclusion Criteria
Patients included in this study met the following criteria: presence of FBAO, choking, or cardiac arrest due to choking. The diagnosis was performed by a physician who initially examined the patient; multiple diagnoses were allowed. Patients with aspiration, accidental ingestion, nasal foreign bodies, and esophageal foreign bodies were excluded.
Data Collection
The following data were extracted from EMS activity records: date, time course, place of occurrence, age, sex, diagnosis, and presence of cardiac arrest. The main outcome was occurrence of out-of-hospital cardiac arrest (OHCA) before hospital arrival. If the patient experienced cardiac arrest, the following additional data were extracted: method of airway clearance and neurological outcome at 30 days. Neurological outcomes were evaluated using the cerebral performance category scale (CPC). Reference Perkins, Jacobs and Nadkarni7,Reference Jennett and Bond8
Statistical Analysis
Descriptive analysis was carried out on the characteristics of patients with FBAO who were transferred by EMS; therefore, the target number of patients was not defined. To analyze patients with FBAO who developed cardiac arrest, the OHCA and non-OHCA groups were compared using univariate analysis. Mann-Whitney U test was carried out on continuous variables presented as median and interquartile ranges, and the χ-square test was carried out on categorical variables. A P value of <.05 was considered statistically significant. All data were analyzed using R version 4.0.4 (The R Foundation for Statistical Computing; Vienna, Austria).
Results
Of the 2,429,175 patients who were transferred to the hospital, 3,807 (0.2%) patients had FBAO (Figure 1). The proportions of women and men were 2,060 (54.1%) and 1,747 (45.9%), respectively, with a median age of 82.0 (71.0–89.0) years. Bimodal age groups comprised infants and the older adults with 271 patients (7.1%) aged under four years (Figure 2). The number of patients with FBAO increased with age, with the highest proportion among those aged 86 years. The highest number of cases was 99 (2.6%), which occurred on January 1 (New Year’s Day), followed by 40 cases (1.1%) on January 2, and 28 cases (0.7%) on January 3 (Figure 3). The number of patients with FBAO on the first three days of the year was significantly higher than those on the other days (19 versus 3; P = .004). The most common times of the day were during lunch and dinner, with few cases occurring late at night (Figure 4).

Figure 1. Inclusion Criteria.
Abbreviation: OHCA, out-of-hospital cardiac arrest.
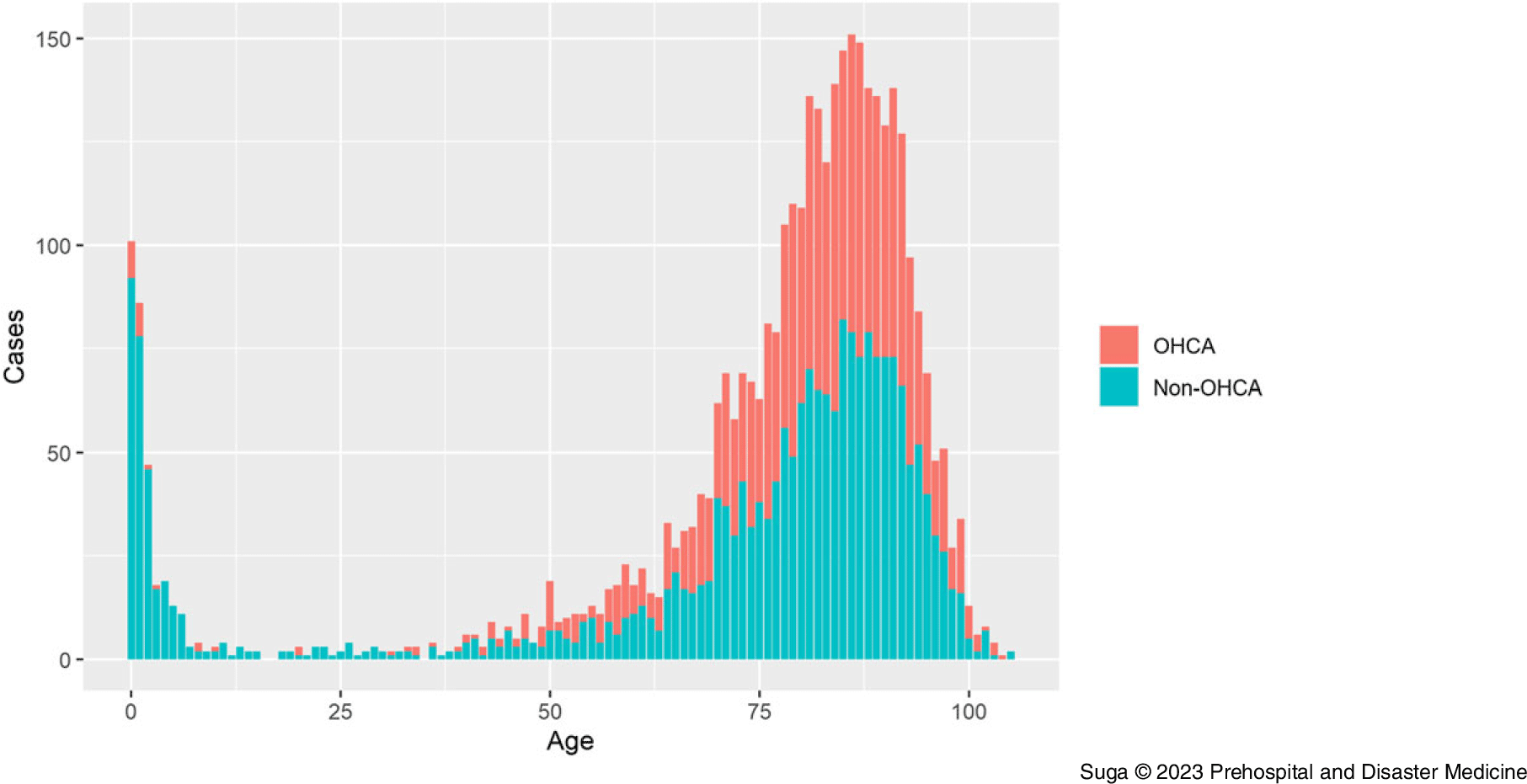
Figure 2. Age Distribution of Patients with Foreign Body Airway Obstruction.
Note: The age distribution was bimodal: infants and the older adults. Green represents non-OHCA and red represents OHCA. The proportion of non-OHCA patients was significantly higher in the infant group than in the older adult group.
Abbreviation: OHCA, out-of-hospital cardiac arrest.

Figure 3. Number of Occurrences of Foreign Body Airway Obstruction by Month.
Note: There is a peak from January 1 through January 3.

Figure 4. Heat Map of Day and Time when FBAO is Most Likely to Occur.
Note: FBAO most commonly occurs at lunch and dinner times, with few occurrences between 9:00pm and 6:00am.
Abbreviation: FBAO, foreign body airway obstruction.
The number of patients who experienced OHCA caused by FBAO was 1,644 (43.2%). Comparing the OHCA and non-OHCA groups, there were significant differences in age, sex, time spent at the site, distance between the site and hospital, place of occurrence, and time of occurrence (Table 1). There were no significant differences in the rate of OHCA occurring in residences and nursing homes following Bonferroni correction (P = .17). The prevalence of OHCA was 7.0% for patients under four years old and 46.0% for the rest, and infants had a significantly lower proportion of those with cardiac arrest after FBAO (P < .001). Of the patients with OHCA, 446 (27.1%) patients received advanced airway management at the emergency scene, 201 (12.2%) were intubated, 245 (14.9%) had laryngeal tube suction, and 371 (22.6%) had prehospital return of spontaneous circulation (ROSC). Neurological outcomes at 30 days were as follows: CPC1 = 23 (1.4%); CPC2 = 20 (1.2%); CPC3 = 47 (2.9%); CPC4 = 60 (3.6%); and CPC5 = 1,494 (90.9%); Figure 5. In total, 98.2% (1,250/1,273) of patients who did not have ROSC before hospital arrival died within 30 days, a significantly higher mortality rate than that in patients who had ROSC (98.2% versus 65.8%; P < .001).
Table 1. Patient Demographic Characteristics

Abbreviation: OHCA, out-of-hospital cardiac arrest.

Figure 5. Outcomes at 30 Days After Admission.
Note: Among 371 patients who had ROSC at hospital arrival, neurological outcomes were as follows: CPC1 = 19 (5.1%); CPC2 = 20 (5.4%); CPC3 = 43 (11.6%); CPC4 = 45 (12.1%); and CPC5 = 244 (65.8%). Among 1,273 patients who did not have ROSC at hospital arrival, neurological outcomes were as follows: CPC1 = 4 (0.3%); CPC2 = 0 (0%); CPC3 = 4 (0.3%); CPC4 = 15 (1.2%); and CPC5 = 1,250 (98.2%).
Abbreviations: CPC, cerebral performance category; ROSC, return of spontaneous circulation.
Discussion
This study included all emergency transfers due to FBAO recorded in the database of the fire department and revealed that FBAO was more likely to occur among infants and the older adults from January 1 through January 3, and during lunch and dinner hours, as noted in the EMS records. Infants had significantly lower proportion of those with cardiac arrest after FBAO. Among patients who did not have ROSC before hospital arrival, 98.2% died within 30 days.
The occurrence of FBAO is seasonal in Japan. Reference Igarashi, Norii, Sung-Ho, Nagata and Yokota9 A Japanese study that analyzed deaths caused by FBAO over a 10-year period found that January 1 recorded the highest number of deaths, followed by January 2 and January 3 (average of 71, 55, and 45 deaths, respectively), which was much higher than the average number of daily occurrences (13 deaths). Reference Taniguchi, Iwagami, Sakata, Watanabe, Abe and Tamiya10 Analysis of the number of emergency transfers showed similar results in that they were related to the Japanese custom of eating rice cakes during the New Year’s holiday. In total, 24.5% of OHCA cases caused by rice cakes occurred on the third day of the New Year. Reference Kiyohara, Sakai and Nishiyama11 Rice cakes have traditionally been eaten for more than 1,000 years in the hope of a long life, in reference to their ability to stretch. Because the risk of FBAO is widely known, it is considered a personal responsibility, and there are hardly any preventive regulations. In contrast to that in Tokyo, a fire service in London, United Kingdom found that the number of occurrences remained almost constant throughout the year. Reference Pavitt, Nevett and Swanton12
Nearly one-half of the patients with FBAO experience cardiac arrest before the EMS arrives. A strong correlation between time to foreign body removal and neurological outcome has been reported: removal of the foreign body within five minutes resulted in an incident rate of death or persistent vegetative state of six percent; however, the prevalence was 47% for 6–10 minutes, 68% for 11–25 minutes, and 70% for ≥26 minutes. Reference Igarashi, Norii and Sung-Ho13 Nevertheless, because it took 8.7 minutes from the emergency call to EMS arrival in this study, it is unlikely that the foreign body could have been removed by the EMS within five minutes, indicating the importance of first aid by bystanders.
Infants had a significantly lower proportion of those with cardiac arrest after FBAO compared with the rest. Infants are in the process of developing swallowing functions, and they bring anything to their mouths. Toys, household items, and food can cause FBAO. Reference Rimell, Thome and Stool14 There are several possible reasons for OHCA being less common in infants than in adults. Infants eat under adult supervision and are not given food that is likely to cause FBAO, making it easier to remove foreign bodies. In addition, there may be differences in the effectiveness of first aid due to body size and strength of the cough reflex.
Patients with FBAO who experienced cardiac arrest had extremely poor outcomes and their proportion of favorable neurological outcome was 1.4%–2.6%. Reference Igarashi, Yokobori, Yoshino, Masuno, Miyauchi and Yokota5,Reference Kiyohara, Sakai and Nishiyama11,Reference Igarashi, Norii and Sung-Ho13,Reference Otomune, Hifumi and Jinno15,Reference Kitamura, Kiyohara and Sakai16 Analysis of the risk factors leading to OHCA in this study revealed that the OHCA group comprised significantly older patients and had a higher proportion of men compared with the non-OHCA group. Considering dental problems and dysphagia, FBAO occurs more frequently among the older adults. Reference Holen and Dickler17,Reference Mittleman and Wetli18 There was no significant difference in the incident of OHCA between residences and nursing homes; nursing homes had the same rate of OHCA as residences, despite the presence of nurses and caregivers. In the OHCA group, time spent at the scene was shorter and distance from scene to hospital was longer than those in the non-OHCA group. Tokyo has 26 tertiary emergency medical facilities and more than 300 secondary emergency medical facilities; in principle, patients with OHCA were transferred to tertiary emergency medical facilities, which are fewer in number; thus, the transfer distance was longer. Both the OHCA and non-OHCA groups require foreign body removal and ventilation at the site, although the on-site stay of the OHCA group may be prolonged if other procedures (eg, adrenaline administration) are performed according to Advanced Life Support guidelines; the OHCA group tended to have a shorter on-site time.
This study found that 98.2% of patients with OHCA who did not have ROSC upon arrival at the hospital died within 30 days. As hypoxia is the cause of cardiac arrest, it is necessary to remove foreign bodies as soon as possible and improve the hypoxic state through adequate ventilation. Because a longer airway obstruction time was associated with vegetative state or death in patients with FBAO, Reference Igarashi, Norii and Sung-Ho13 it is preferable to perform procedures for removing foreign bodies (stay and play) rather than to immediately transfer the patient to the hospital (scoop and run). However, advanced airway management was performed in only 27.1% of patients, and this may reflect the fact that patients in the OHCA group had a significantly shorter time spent at the scene and “scoop and run” was chosen. Furthermore, although laryngeal tube suction is not recommended—because the tube is indiscriminately inserted and may push foreign objects further inside—it was found that laryngeal tube suction is used more often than tracheal intubation in cases of FBAO.
Limitations
This study had several limitations. First, patients with OHCA had outcomes recorded at 30 days, while those with non-OHCA did not. Second, the database does not include information on bystander first aid or types of foreign bodies. As this information is not mandatory, it was not collected in this study. A prospective cohort study, the Multi-Center Observational Choking Investigation/MOCHI registry, is currently in progress to address these issues. Reference Norii, Igarashi and Sung-Ho19
Conclusion
This study revealed that FBAO occurred among infants and the older adults more frequently from January 1 through January 3 and during lunch and dinner times. Further precautions should be taken against FBAO at the beginning of the year. Among patients who did not have ROSC upon arrival at the hospital, 98.2% died within 30 days. It is important to remove foreign bodies and provide sufficient ventilation to the patient at the scene to increase the potential for ROSC.
Conflicts of interest/funding
The authors declare none.









