Introduction
Ever since the first cluster of cases in Wuhan, China was announced on 31 December 2019, SAR-CoV-2, the virus responsible for COVID-19, has spread rapidly around the world affecting more than 6 million cases and resulted in more than 300 000 deaths [1]. Many countries have sought to control the outbreak with different policy measures, including city or country ‘lock-downs’ of varying degree.
In Singapore, the first COVID-19 case was detected on 23 January 2020. The initial cases were mainly imported from China and subsequently from regional countries, Europe and America. Some were travellers and some were Singaporeans returning from work or studies overseas. Subsequently, there was limited community transmission and several clusters of infections at workplaces and households. Ministry of Health, Singapore, and other governmental agencies scaled up contact tracing operations and set up quarantine facilities nationwide. By 2 April 2020, Singapore reported a total of 1049 cases, among which 51% were imported.
Researchers have sought to understand the science of this novel COVID-19 disease so as to guide public health measures to detect, control and prevent the spread of this infection internationally. Incubation period of an infectious disease is the time from exposure to the causative agent to when symptoms first appear. It can provide important information during an outbreak including when infected individuals will become symptomatic and most likely to spread the disease to another naïve person. Understanding the incubation period of a novel infectious disease provides clues about the cause and source of a disease. Incubation period is a key component to be established early because this has important implications for public health measures such as disease surveillance, contact tracing, active case finding, quarantine operations and modelling of burden of disease in the country, for planning healthcare resources and evaluating the effectiveness of measures implemented by the public health agencies. The incubation period and factors that influence it affect the length of public health measures such as quarantine and isolation. Many countries use incubation period to decide the period of lockdown and control measures.
Some data of incubation period have been published internationally. An analysis in January 2020 based on 88 confirmed COVID-19 cases in Chinese provinces outside Wuhan showed a mean incubation period of 6.4 days (95% CI 5.6–7.7 days), with a range of 2.1–11.1 days [Reference Backer, Klinkenberg and Wallinga2]. Linton et al. in their analysis based on 158 confirmed cases outside Wuhan found the median incubation period was 5.0 days (95% CI 4.4–5.6 days), with a range of 2–14 days [Reference Linton3]. These data are however variable. In a report from Germany, the median incubation period was 4.0 days, with a range of 1–7 days [Reference Böhmer4], while in Vietnam, it was 5.6 days [Reference Bui5].
Similar human coronaviruses such as SARS (mean 6.4 days, range 1.0–11.0 days) [Reference Chan-Yeung and Xu6], MERS (mean 6.0 days, range 2–14 days) [Reference Virlogeux7] and other human coronavirus (mean 3.0 days, range 2.0–5.0 days) [Reference Lessler8] have largely equivalent incubation periods as well. To our knowledge, no study has demonstrated an association between age and incubation period among COVID-19 patients.
Singapore is geographically small compared to other countries. Surveillance systems including case reporting and activity mapping of all incident cases of COVID-19 infection, tracing of all close contact and placing them on quarantine, have been set up early on in the pandemic. Singapore has identified locally linked cases involving families, colleagues and social groups, and is thus well-positioned to study the incubation period of this new virus. This paper aims to estimate the incubation period of COVID-19 among locally transmitted cases, and to study its association with age so as to better inform public health measures.
Methods
From 23 January 2020 to 2 April 2020, epidemiological data of all confirmed cases of COVID-19 admitted to restructured hospitals in Singapore was collected. A confirmed case of COVID-19 is defined as an individual with a respiratory sample testing positive for SARS-CoV-2 using a laboratory-based PCR test (sensitivity of 1st swab is 89%, 2nd swab is 95% and specificity is 100% [Reference Lee9]). For every positive case, a detailed epidemiological investigation is conducted through a phone interview by trained personnel using a common template to record information of activities. Activity mapping is conducted by capturing all activities 14 days prior to symptom onset (backward mapping) until the day of admission to hospital (forward mapping). The earliest date of any symptom suggestive of community-acquired pneumonia, community-acquired respiratory infection such as breathlessness, cough, sore throat, rhinorrhoea, anosmia and symptoms of community-acquired pneumonia is denoted as the date of onset (DOO) for this individual. The activity map of the individual is examined for all possible close contacts who tested positive. The earliest date of interaction between the close contact who tested positive is denoted as the exposure date of this individual. Positive cases with no clear exposure to another positive case were excluded from the analysis as we were unable to ascertain their incubation period. Incubation period (days) was the duration calculated from the date of exposure (DOE) to the DOO plus 1. Patients selected were those with a known exposure period as captured by the activity mapping. Other data that were collected included demographic data such as age at date of COVID-19 diagnosis, gender, date of hospitalisation and discharge after full clinical recovery.
There were 1049 cases with confirmed SARS-CoV-2 infection diagnosed in Singapore from 23 January 2020 to 2 April 2020. Only 177 cases (16.9%) could provide a definite exposure date. In the remaining 872 cases (83.1%), the contact tracing teams were unsure of the identity of the probable infector and thus were unable to assess if these cases were epidemiologically linked. Of the 177 cases with definite exposure, only 164 cases (92.7%) had a definite symptom onset date (DOO) and met the inclusion criteria for the computation of incubation period in this study.
Descriptive statistics were analysed for the selected cases, including the number and proportions for categorical variables as well as mean and median for continuous variables. Univariate analyses such as χ 2 test and independent sample t-test were performed to identify differences between categorical groups and sample means, respectively, whilst median test was used to assess differences in medians between categorical groups. Association between continuous variables was examined using Spearman correlation coefficient. The findings were considered statistically significant at the 5% level (P < 0.05). Statistical analyses were done using the Statistical Packages for Social Sciences (SPSS) v22.0.
Results
Of the 164 cases analysed, their mean age was 44.2 years (s.d. 15.8); 77 (47.0%) were male and 121 (73.8%) were Singapore residents (Table 1). In comparison with excluded cases, the excluded cases were younger (mean ages 40.5 vs. 44.2 years, P = 0.010), more males (59.4% vs. 47.0%, P = 0.003) and more imported cases (57.4% vs. 18.9%, P < 0.001).
Table 1. Demographic characteristics of COVID-19 patients

* Included Spain (5), Switzerland (4), the Netherlands (3), Japan (3), Brazil (3), Sri Lanka (2), Sweden (2) and others.
† Incubation period = Date of symptom onsets – Date of exposure + 1 day.
‡ Day of illness at admission = Date of admission – Date of symptom onsets + 1 day.
Noted:
(i) Missing values of included cases: Day of illness at admission (6);
(ii) Missing values of excluded cases: Nationality (3), Residence status (2), Day of illness at admission (115).
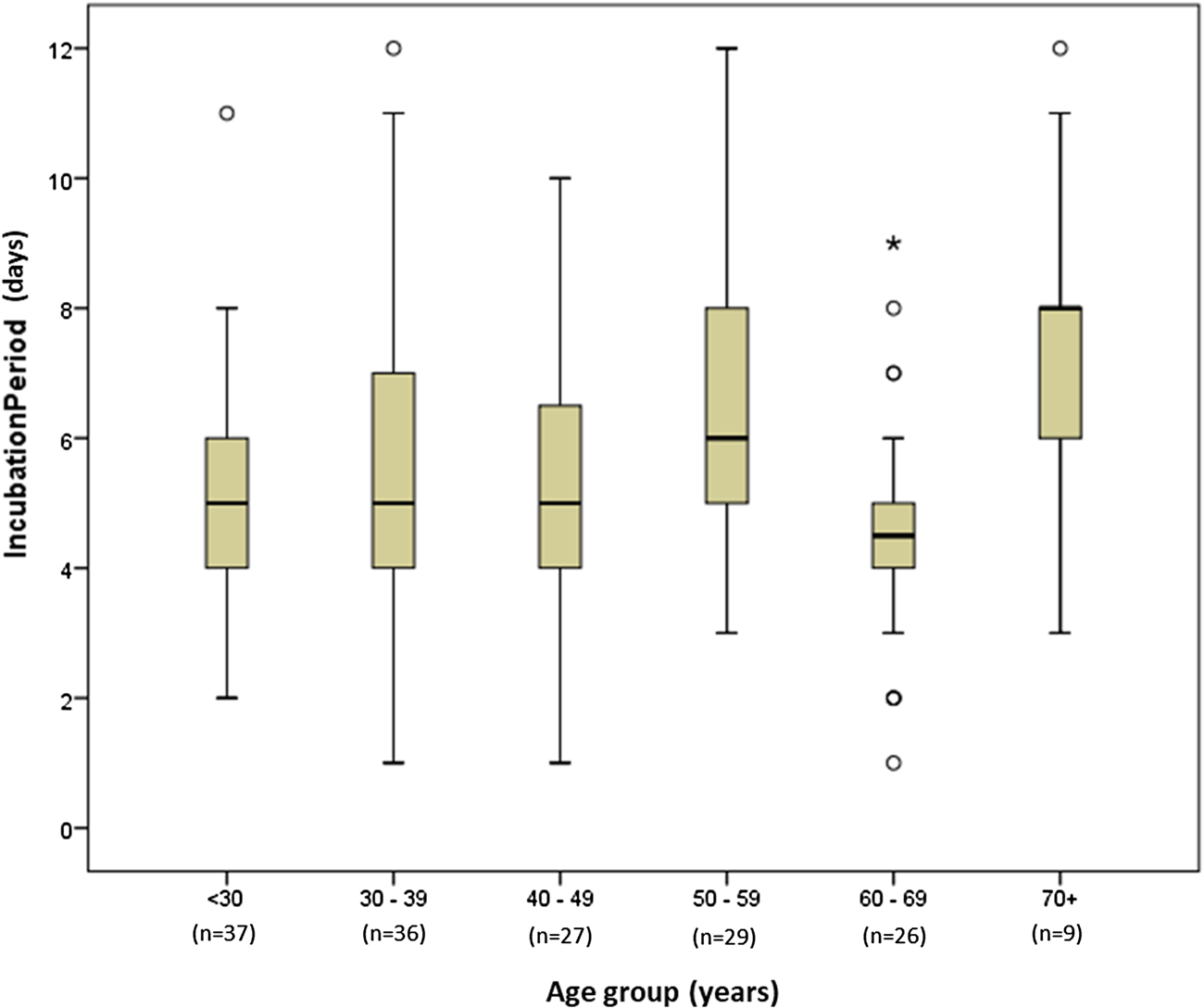
We estimated that the median incubation period of the included cases was 5 days (range 1–12 days) (Fig. 1). Except for age group of 60–69 years, the older age groups appeared to have a longer incubation period. The median incubation period among those <30, 30–39 and 40–49 years was 5.0 days; whilst that of 50–59, 60–69 and 70 years and above were 6.0, 4.5 and 8.0 days, respectively (Fig. 2). The incubation period of the included cases had similar mean and median. Overall, the mean incubation period was 5.54 days (95% CI 5.18–5.90). Age-specific mean incubation periods were statistically significantly different (P = 0.005) across different age categories. The longest was observed among those aged 70+ (7.56 days, 95% CI 5.31–9.80) whilst the shortest was among those aged 60–69 years (4.69 days, 95% CI 3.86–5.52) and <30 years (4.95 days, 95% CI 4.31–5.58). Mean incubation periods among those aged 30–39, 40–49 and 50–59 years were 5.78 days (95% CI 4.91–6.65), 5.33 days (95% CI 4.53–6.14) and 6.34 days (95% CI 5.42–7.27), respectively. Overall mean incubation period of those aged <70 years was shorter than those aged 70+ years (5.43 vs. 7.56 days, P = 0.008). There was a significant negative correlation between incubation period and day of illness at admission among those <70 years (Spearman's ρ: −0.270; P < 0.001). This suggests that cases with a longer incubation period had earlier admission to hospital. However, this relationship was not statistically significant among those 70 years and above (ρ: −0.305; P = 0.425).
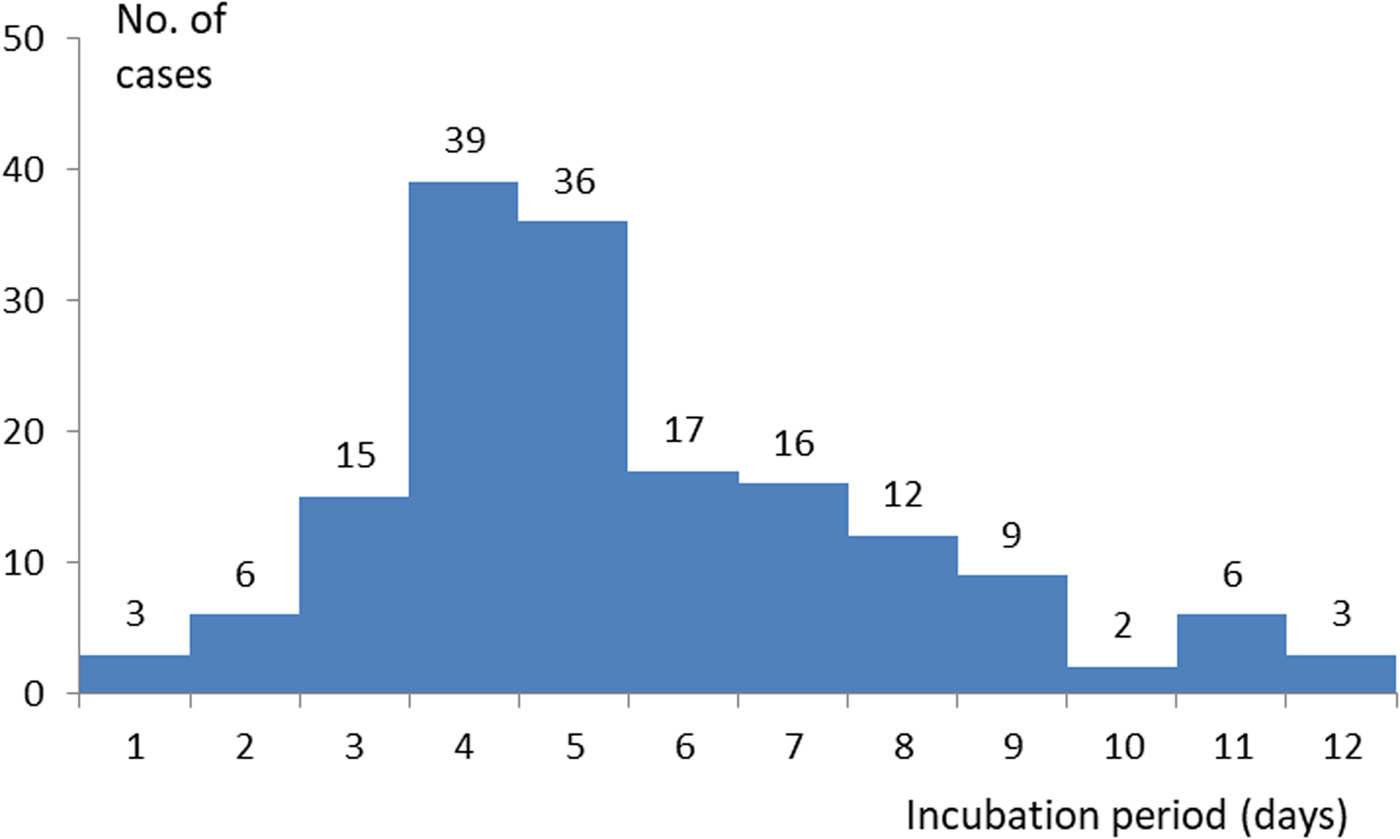
Fig. 1. Incubation period of patients with known exposure to another positive case.

Fig. 2. Box plot of incubation period byage group.
The younger age groups were found to have a shorter length of stay (LOS). Those aged 30–39 years had the shortest median LOS of 13 days, followed by those aged <30 years at 13.5 days. Although a short median LOS of 13 days was also observed among those aged 60–69 years, they had remarkably larger variability (range 6–64 days) leading to the longest average LOS of 18.7 days across all age groups. Comparatively, those aged 70+ years had long median and average LOS at 15 and 17.7 days, respectively, with a relatively smaller variability (range 9–38 days) (Table 2).
Table 2. Breakdown of length of stay according to age groups

s.d., standard deviation.
a Excluded two cases that were still admitted and three death cases. Missing values: 44 cases (27.7%).
Discussion
Estimates of the COVID-19 incubation period differ widely across the world; some suggest that it can be as short as 3–4 days [Reference Linton3] or as long as 6–7 days [Reference Backer, Klinkenberg and Wallinga2]. Early data from Singapore suggests that it is around 4 days [Reference Pung10]. This difference could be due to inherent variations in the biology of the strain locally vis-à-vis abroad [Reference Wang11]. This study reports a median incubation period of 5 days with a maximum of 12 days and supports current literature with regards to the incubation period of COVID-19. The result also affirms Singapore's use of 14 days for backward activity mapping and defining period of quarantine operations. Since March 2020, travellers who return from overseas to Singapore are mandated to be isolated on a Stay Home Notice (SHN) for 14 days. If exposed to SARS-CoV-2 before isolation or quarantine, a person should present with symptoms way before 14 days. Persons under quarantine who remain asymptomatic at the end of 14 days should be considered unaffected by COVID-19.
Our study showed that older patients, in particular 70 years and above, had longer incubation periods than younger ones. We postulate that this is due to a slower immune response amongst older patients. This corroborates with existing literature about SARS 2003, which also had features of an immune-modulated disease like COVID-19. Cowling et al. hypothesised about this in their report in 2007 [Reference Cowling12] on SARS 2003, where they demonstrated that older patients had longer incubation periods, suggesting that this might have resulted from a delayed immune response.
Additionally, in patients younger than 70 years old, those with longer incubation periods were admitted earlier after the onset of illness. It is worth noting that this trend was also observed among those 70 years old and above, and the correlation appears to be stronger than the younger cases (−0.305 vs. −0.270) even though it did not reach statistical significance, possibly due to the small sample size of nine in this group of patients. Patients with short incubation periods may present later to hospital as their infector, who has taken some time to be diagnosed after being symptomatic, has to be diagnosed first before the individual is aware of his vulnerability and be on the look-out for COVID-19 symptoms. Conversely, a person who has a longer incubation period would likely to be already quarantined because of the infector has been found. Through contact tracing operations and close telephonic surveillance, upon developing the first symptoms, the person under quarantine will inform the quarantine official and be sent to hospital for testing immediately and admitted to hospital if found to be positive for COVID-19 infection.
We postulate that an elderly person could have more recall bias and be more likely to ignore early symptoms and only report later when symptoms become more severe or intolerable. This is supported by observational studies that showed age correlates with the severity of disease at onset. Guan et al. in their study of 1099 patients with laboratory-confirmed COVID-19 in mainland China showed that patients with severe disease at onset were older than those with non-severe disease by a median of 7 years. Conversely, a report on a cluster of younger patients by Huang et al. affirmed that symptoms tend to be milder than in older patients with COVID-19 [Reference Huang13].
It is noteworthy that those 60–69 years of age had a relatively large number of outliers (34.6%) in the incubation period. In this study, the incubation period of this age group had a smaller interquartile range (IQR) of 3.75–5.25 days (i.e. IQR of 1.5 days) and more cases fulfilled the definition of an outlier. Comparatively, incubation periods of other age groups had larger variability with IQRs of 3–4.5 days, particularly those aged 70+ had the largest IQR of 4.5 days (i.e. 5–9.50 days).
Little was known of COVID-19 infection initially when it was first reported in China in January 2020. It was crucial to synthesise new scientific evidence of SARS-CoV-2 virus and educate the public, especially the elderly sub-population who are at higher risk of morbidity and mortality associated with the infection. This includes the recognition of common symptoms of COVID-19, practice of safe distancing measures and modification to health-seeking behaviour to consult their family physician early, etc. Ministry of Health and national agencies have been prompt to package information and disseminate publicly to both the young and elderly.
Our analysis has some important limitations. First, there is a possibility of recall bias leading to patients over or underestimating the time of exposure to someone who was a confirmed case of COVID-19 as this was only taken retrospectively when the patient is admitted to the hospital. Similarly, patients may not recall accurately their first symptom. As many COVID-19 symptoms are mild, transmission could have already occurred before noticing symptoms. Hence, self-reported DOO is often later, resulting in a longer reported incubation period.
Second, asymptomatic or pre-symptomatic spread could have linked some of the cases. However, the magnitude of impact on our results is difficult to ascertain as asymptomatic and pre-symptomatic cases are difficult to diagnose and our study was conducted before widespread COVID-19 testing was readily available. Rigorous contact tracing allowed us to quickly identify and quarantine close contacts who could either be asymptomatic or pre-symptomatic.
Third, we only included 15.6% of all cases in Singapore in this study. The majority of patients were unable to provide information on a definite exposure or unlinked epidemiologically and were excluded from the analysis. However, the cases we analysed had complete information about their exposure and DOO of the infector. The incubation periods of these cases were directly linked to the infector through contact tracing operations and activity mapping of trained personnel. Thus, the incubation period of these cases was well-linked epidemiologically. The above limitations were also mitigated by the relatively small geographical size in Singapore aggressive contact tracing done for each case to corroborate the history of patients and to maximise the number of patients with a definite exposure to be included in this study.
Further studies can be undertaken to better understand the mechanisms behind pre-symptomatic and asymptomatic transmission of COVID-19 infection and in particular whether an older person mounts a delayed response to the SARS-CoV-2 virus.
Conclusion
We found that incubation period of locally-acquired COVID-19 cases in Singapore ranged from 1 to 12 days with a median of 5 days, supporting the existing use of 14 days to apply duration of quarantine and twice the maximum incubation period for monitoring and closure of active clusters of transmission in Singapore. We also found that people aged 70 years and older have a longer incubation period than younger individuals, suggesting that earlier and more proactive testing may be beneficial for an elderly person with known exposure to a positive case.
Acknowledgements
Our study team appreciates the clinical colleagues and personnel involved in the activity mapping at all public hospitals as well as officials involved in contact tracing operations. They record detailed clinical history and investigate epidemiologic linkages of all COVID-19 infections in Singapore.
Conflict of interest
We declare no competing interests.
Data availability statement
Data were obtained under governmental laws and cannot be released publicly.