Over the past few decades, type 2 diabetes mellitus (T2DM) has become one of the highly prevalent and growing chronic diseases, severely threatening the Chinese population(Reference Wang, Gao and Zhang1). A series of epidemiological studies showed a positive and robust relationship between the risk of stroke and T2DM(Reference Almobarak, Badi and Elmadhoun2,Reference Munoz-Rivas, Mendez-Bailon and Hernandez-Barrera3) . It is well known that diabetic patients with stroke have an extended hospital stay, poor prognosis and high mortality rate. The heavy burden of T2DM and stroke bringing to individuals and society worldwide is expected to increase in the next few years(Reference Al-Rubeaan, Al-Hussain and Youssef4). Common complications including hypertension, hypercoagulability, abnormal haemorheology, dyslipidaemia and other factors that occurred in T2DM patients may lead to arteriosclerosis. These factors interact with each other, resulting in a significantly increased risk of CVD(Reference MacDonald, Madika and Gomes5). Briefly, people with diabetes have a higher risk of stroke compared with non-diabetic patients(Reference Guo, Yu and Zhong6–Reference Low Wang, Hess and Hiatt8).
Stroke, as one of the most prominent complications of T2DM, is the frequent cause of death and long-term disability worldwide(Reference Lopez, Mathers and Ezzati9). The age-standardised stroke mortality has declined globally over the past 20 years. However, the absolute number of stroke events, deaths and stroke burden increases substantially, especially in developing countries(Reference Huang, Li and Zhu10,Reference Avan, Digaleh and Di Napoli11) . The number of stroke deaths in China accounts for about one-third of the global deaths of stroke, and the number of stroke patients has reached 13 million. China has become the country with the highest lifetime risk of stroke, with a massive burden of 39·3 %(Reference Wang, Li and Gu12). It is a remarkable fact that stroke is considered as a long-term and comprehensive disease caused by modifiable factors such as diet, physical activity, smoking and consumption of alcohol(Reference MacDonald, Madika and Gomes5,Reference Xia, Yue and Chao13,Reference Pan, Jin and Jun14) .
Emerging evidence has revealed that dietary patterns also play an essential role in preventing stroke in the general population(Reference Frederiksen, Themsen and Overvad15–Reference Wang, Huang and Xiang17). Substantial researches have been carried out over the past few decades to advance understanding of the impact of dietary patterns on stroke mechanisms(Reference Frederiksen, Themsen and Overvad15,Reference Shi and Ganji16,Reference Talaei, Koh and Yuan18) . Adherence to Dietary Approaches to Stop Hypertension (DASH) and prudent dietary pattern demonstrated a protective effect on stroke, whereas inverse associations were observed in the Western dietary pattern(Reference Talaei, Koh and Yuan18–Reference Feng, Fan and Wu20). The Mediterranean diet was associated with increased CVD stroke(Reference Chen, Neelakantan and Martin-Calvo21–Reference Spence23). The dietary patterns were not consistent across global regions, such as Europe and Asia, due to the complexity and diversity of food(Reference Frederiksen, Themsen and Overvad15,Reference Li, He and Lai24) . A prospective cohort study of 13 055 adults in China suggested a negative association between traditional dietary pattern, which emphasises a high intake of rice, pork, fish, poultry and fresh vegetable but low intake of wheat and CVD. On the contrary, modern dietary pattern characterised by a high intake of fruit, soya milk and fast food was associated with an increased risk of CVD(Reference Shi and Ganji16).
Although multiple epidemiological studies have extensively focused on dietary patterns and their effect on stroke in a general population(Reference Shi and Ganji16,Reference Kontogianni and Panagiotakos25,Reference Li, Hou and Chen26) , little was known regarding the relationship between dietary patterns and stroke in patients with T2DM. For this purpose, our study was thus far the first study aimed to explore the impact of different dietary patterns on stroke outcomes in T2DM patients in China.
Materials and methods
Participants and procedure
This was a cross-sectional study conducted among T2DM patients aged ≥ 18 years in China from December 2013 to January 2014. A representative sample including forty-four towns/streets selected from sixty-five towns/streets of two regions in the south and north of Jiangsu Province randomly was obtained using a stratified cluster random sampling method. Resident health records of 20 053 T2DM patients were enrolled in the essential public health service management system. Three groups of participants were excluded: (1) participants diagnosed with stroke before T2DM, (2) patients with a duration of T2DM < 1 year and (3) participants with missing values of questionnaires. Finally, 13 731 participants diagnosed with T2DM patients between 1982 and 2012 were successfully involved in the analysis.
Data collection
Information regarding demographic characteristics (age, gender, region, residence, level of education, marital status, household income, employment, duration of diabetes), health-related behaviours (smoking, drinking and physical activity) and related diseases (hypertension, dyslipidaemia, overweight and obesity) was collected through standard paper questionnaires by well-trained staff members.
Definition of variables
Fasting plasma glucose (FPG) ≥ 7·0 mmol/l on at least two separate occasions by previous diagnosis of professionals or use of medication was defined as T2DM(27). Stroke was defined as sudden onset of non-convulsive and focal neurological deficit lasting more than 24 h. It was classified as ischaemic stroke, subarachnoid haemorrhage, brain haemorrhage and other types of stroke by previous physician diagnosis. Self-reported stroke patients were defined as those who answered ‘NO’ to this question ‘Have you ever been diagnosed with stroke by a neurologist?’ People who have smoked at least 100 cigarettes in one’s lifetime was defined as a smoker. Drinking more than once a month was considered drinking. Physical activity information was obtained through the global physical questionnaire(Reference Cleland, Hunter and Kee28). The level of physical activity was calculated using the metabolic equivalent value of various physical activities and the duration and frequency of multiple activities. For each physical activity group, participants reporting no physical activity were first classified as zero physical activity, with the remainder divided into tertiles of the level of physical activity: low level (first tertile), moderate level (second tertile) and high level (third tertile). BMI was calculated by weight in kilograms divided by the square of height in metres. It was divided into four levels: underweight (BMI < 18·5), normal weight (18·5 ≤ BMI < 24·0), overweight (24·0 ≤ BMI < 28·0) and obesity (BMI ≥ 28·0)(Reference Chen and Lu29). Previous studies have confirmed that these covariates selected in this study are related to dietary patterns and stroke in propensity score matching (PSM)(Reference Avan, Digaleh and Di Napoli11,Reference Zhang, Mu and Yan30–Reference Chen, Zhao and Ruan33) .
Dietary intake assessment
Dietary intake was evaluated through a validated seventeen FFQ by well-trained investigators from December 2013 to January 2014. Data on intake and frequency of various foods consumed in the last year were collected using the paper questionnaire. Information on average daily intake of each kind of food which included rice and noodles, whole grains, poultry meat, livestock meat, aquatic products, fresh vegetables, fresh fruits, soyabean products, eggs, dairy products, nuts, fried foods, cakes, salted products, juice, beverages and carbonated drinks was calculated (g/d).
Propensity score matching
Patients were matched based on their propensity scores to dietary patterns. The propensity scores of each participant were calculated by propensity model (multivariate logistic regression model) founded on fifteen confounding factors including demographic characteristics (age, duration of diabetes, gender, residence, household income, level of education, marital status and occupation), health-related behaviours (smoke, drink and effective exercise), related diseases (hypertension, dyslipidaemia, overweight or obesity) and HbA1c levels.
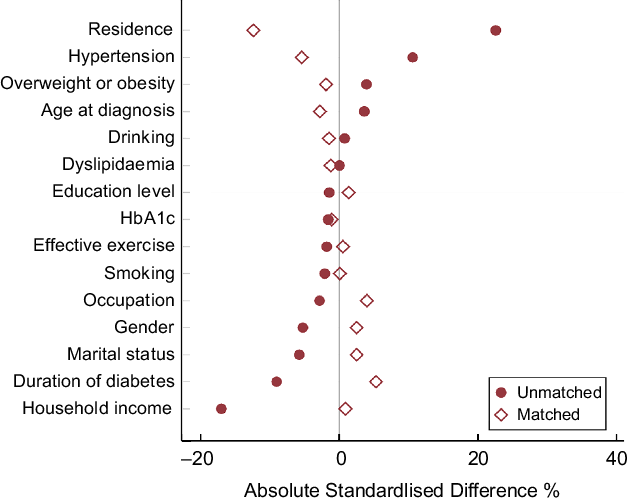
Each participant in the high-fat pattern group was matched to an object in the balanced pattern group through nearest neighbour matching in a 1:1 ratio with a caliper width of 0·02. The participants after matching were used for subsequent analyses. To evaluate matching effect of the sample, we acquired the absolute standardised differences based on fifteen confounding factors before and after PSM.
Statistical analysis
Statistical analyses were performed on software Mplus version 7.0 and R version 4.0.2. The descriptive statistics including percentage and median were used to describe the demographic characteristics. The chi-squared test and the Mann–Whitney U test were used to assess the demographic characteristics differences between dietary patterns before and after PSM. Foods were first aggregated into seventeen mutually exclusive foods to determine dietary patterns using latent class analysis. For each kind of food, participants were first classified as those reporting zero intake, with the remainder divided into tertiles of intake and then categorised into three categories: low intake (first tertile), moderate intake (second tertile) and high intake (third tertile). The best-fitting model was determined on the basis of information criteria-based metrics, including the Akaike information criterion (AIC); Bayesian information criterion (BIC); sample-size-adjusted Bayesian information criterion (aBIC); Lo–Mendell–Rubin likelihood ratio test (LMR); Bootstrap likelihood ratio test (BLRT); entropy and substantive interpretation. Different dietary patterns were described based on the conditional probabilities of the corresponding foods.
Binary logistic regression was used for the entire population, and conditional logistic regression was used for propensity score-matched population in subgroup analysis to assess the risk of stroke and OR, and related 95 % CI were calculated. P < 0·05 (bilateral) was considered statistically significant.
Results
Demographic characteristics of type 2 diabetes mellitus patients
A total of 867 (6·3 %) patients had a stroke. The respondents’ ages ranged from 21 to 94 years with a mean age of 63 years. Close to two-thirds of participants (61·0 %) were 60 years and above. Of them, a more significant proportion (60·7 %) of them were females. The highest proportion of participants was residing in urban–rural areas (53·9 %). Further, nearly three-fourth (55·0 %) received junior school or below. With regard to health-related behaviours, there were 27·3 % current smokers and 16·8 % drinkers. In terms of the related diseases, the largest proportion of patients (63·2 %) was overweight or obesity, followed by hypertension (56·3 %), and the least proportion was dyslipidaemia (16·8 %).
Latent class analysis
Model fitting statistics for one to six latent classes were performed in the latent class analysis models among patients with T2DM. Along with the number of estimated classes increased, the Akaike information criterion, Bayesian information criterion and sample-size-adjusted Bayesian information criterion indicated monotonically improving fit. On the other hand, entropy remained consistently above 0·60 and increased with the number of categories. NYLUND et al. found that the Lo–Mendell–Rubin test was the most sensitive index to the classification of potential categories in the Monte Carlo simulation study. When non-significant (P > 0·05), the Lo–Mendell–Rubin and the Bootstrap likelihood ratio test demonstrated that the two-class model fits the data better than the three-class model significantly(Reference Carragher, Adamson and Bunting34). Founded on model fit tests and the aim of parsimony, the two-class model was considered as the best solution of latent dietary patterns (Table 1).
Table 1 LCA fit indices of dietary patterns among patients

LCA, latent class analysis; AIC, Akaike information criterion; BIC, Bayesian information criterion; LMR, Lo–Mendell–Rubin; BLRT, Bootstrap likelihood ratio test.
Of the 13 731 subjects aged 18 years or over in China, 61·2 % were classified as consuming the high-fat pattern, while 38·8 % were described as the balanced pattern. Class 1 labelled the high-fat pattern and showed a higher probability of moderate to high consumption of whole grains, poultry meat, livestock meat, aquatic products, soyabean products, eggs and fresh vegetables, and low consumption of rice and noodles. There is no consumption of fresh fruits, dairy products, fried foods, nuts, cakes, juice, beverages, carbonated drinks and salted products in the high-fat pattern. Subjects in class 2, the balanced pattern, reported a higher probability to consume moderate consumption of rice and noodles, livestock meat, aquatic products, eggs, fresh vegetables, soyabean products and low consumption of whole grains, poultry meat, fresh fruits and salted products. There is no consumption of dairy products, fried foods, nuts, cakes, juice, beverages and carbonated drinks in the balanced pattern (Fig. 1).

Fig. 1 Probabilities of consumption for selected food items by dietary patterns derived from latent class analysis. The green line: low intake of food; the blue line: moderate intake of food; the red line: high intake of food
Characteristics of dietary patterns before and after propensity score matching
Based on the different dietary patterns before matching, participants were divided into high-fat (n 8401(61·2 %)) and balanced (n 5330 (38·8 %)) patterns. There were statistically significant differences between two patterns in all covariates except for age, blood glucose control, smoking and drinking status (Table 2). Overall, 867 (6·3 %) patients had a stroke. Notably, balanced pattern patients were the best possibility to be women and overweight or obese.
Table 2 The comparisons of characteristics by LCA for patients with T2DM before and after matching

LCA, latent class analysis; PSM, propensity score matching; T2DM, type 2 diabetes mellitus.
A total of 4985 balanced pattern patients could be propensity-matched to high-fat pattern patients, creating a new sample of 9970 patients (4985 balanced pattern patients, 4985 high-fat pattern patients). After matching, the balance between two dietary patterns remarkably improved, as none of the confounding factors was significantly different except for occupation, physical activity level, hypertension and residence (Table 2). The groups after PSM were also well balanced in other variables not included in the model. The absolute standardised differences were < 10 % for all covariates between different dietary patterns except for residence (Fig. 2).

Fig. 2 Absolute standardised differences in fifteen covariates between high-fat pattern and balanced pattern patients before and after matching. The maroon solid circle represents absolute standardised differences before matching, and the maroon hollow diamond represents absolute standardised differences after matching
Association between different dietary patterns and stroke in type 2 diabetes mellitus patients
As illustrated in Table 3, there were 583 (5·8%) events of stroke after PSM. Conditional logistic regression models exhibited that the balanced pattern was correlated with a statistically significant decrease in the risk of stroke (OR = 0·61; 95 %CI 0·51, 0·72; P < 0·001). To ensure that these results were not confused by the covariates with unsatisfactory matching, we evaluated the risk of adverse outcomes after adjusting for unbalanced factors after PSM, including occupation, physical activity level, hypertension and residence. After adjustment, the balanced pattern was also to be correlated with decreased risk of stroke (adjusted OR = 0·63; 95 % CI 0·52, 0·76; P < 0·001). The results of the propensity-matched analysis were authenticated in the whole population (OR = 0·61; 95% CI 0·52, 0·71; P < 0·001) (Table 3).
Table 3 Prevalence of stroke and impact of different dietary patterns on stroke outcome in the entire and PS-matched population

(Balanced pattern v. high-fat pattern); PS, propensity score; PSM, propensity score matching.
Data are expressed as n (%) where appropriate. OR and CI were derived from logistic regression models.
Binary logistic As per journal style, unlinked footnotes are not allowed. Hence, please link them with symbols in the sequential order.regression was used for the entire population, and conditional logistic regression was used for PS-matched population.
* In the entire population analyses, adjustment was for the PS; in the propensity-matched population analysis, adjustment was for unbalanced factors after PSM.
Subgroup analysis
To confirm the association between two different dietary patterns and stroke in various subgroups, we carried out subgroup analyses using conditional logistic regression models. The OR for balanced pattern were constantly < 1·0 in all subgroups, demonstrating the decreased risk of stroke. However, the protective effect of the balanced model did not differ significantly (interaction P > 0·05) (Fig. 3).

Fig. 3 Impact of different dietary patterns on stroke outcomes by subgroups after propensity matching
Discussion
To our knowledge, our study is the first study to focus on the impact of different dietary patterns on stroke outcomes in T2DM patients. Compared with traditional methods such as factor analysis to assess dietary patterns, latent class analysis has its unique superiority. First, it has less restrictive premises and is very flexible. Second, it is suitable for clustering analysis of both hierarchical variables and categorical variables. In addition, latent class analysis uses probability to classify based on a specific probability model, which is less arbitrary and more in line with the objective reality. The results showed that there were differences in dietary patterns among patients with T2DM. The typical dietary characteristics of two dietary patterns in T2DM patients contained a variety of foods rich in quality protein such as soyabean products or whole grains and fewer intake of fruits and rice, which may be due to the transition to a low glycaemic index diet after diabetes considering their state of health, especially the reduction in the intake of foods that are likely to contribute to poor control of glycaemia(Reference Pestoni, Riedl and Breuninger35,Reference Alaradi, Ouagueni and Khatib36) .
Participants exhibiting adherence to the balanced pattern consumed moderate amounts of beneficial foods such as white meat, eggs, soyabean products and fresh vegetables tended to a Mediterranean diet, which was beneficial to stroke prevention(Reference Chen, Neelakantan and Martin-Calvo21–Reference Spence23,Reference Geisler37) . A healthy dietary pattern could also affect other modifiable risk factors, namely obesity, diabetes and dyslipidaemia, thereby influencing the risk of stroke(Reference Larsson, Akesson and Wolk38). The association between high-fat pattern and increased stroke risk might be mediated through obesity or central obesity. Patients in the high-fat pattern consumed a high intake of staple foods, including rice and whole grains rich in starch and high-fat foods. A series of researches investigated the relationship between meat consumption and the stroke risk and exhibited that consumption of red meat, which was a source of SFA, was related to an increased risk of stroke(Reference Yang, Pan and Sun39–Reference Bechthold, Boeing and Schwedhelm41), which was in agreement with our findings.
However, the results of a series of studies regarding red meat were also controversial(Reference Bechthold, Boeing and Schwedhelm41–Reference Saneei, Saadatnia and Shakeri43). Several studies found that excessive consumption of red meat was correlated with an increased stroke risk, while moderate consumption of red meat could not result in lipid structural changes or significant blood pressure increases, which supported our conclusion(Reference Bechthold, Boeing and Schwedhelm41–Reference Saneei, Saadatnia and Shakeri43). On the other hand, there is little literature on revealing that high meat intake was negatively correlated with CHD and stroke. High-fat intake, including SFA and unsaturated fatty acid, was associated with reduced stroke risk, and no adverse effects of fat intake on CVD were observed(Reference Wang, Li and Liu44,Reference Dehghan, Mente and Zhang45) . In contrast, consumption of white meat had a protective impact on stroke(Reference Kim, Hyeon and Lee40,Reference Lupoli, Vitale and Calabrese46) . Based on evidence mentioned above, further researches are needed on the association between red meat and stroke in patients with T2DM.
Participants in the balanced pattern also consumed high levels of soyabean products, which may have a protective effect on stroke(Reference Roman, Jackson and Gadhia47,Reference Lou, Li and Yan48) . Beans are rich in protein, carbohydrates, fibre and various micronutrients (such as phytochemicals)(Reference Ozawa, Yoshida and Hata49). A series of meta-analyses of prospective cohort researches on the relationship between eggs and stroke have provided conflicting findings(Reference Bechthold, Boeing and Schwedhelm41,Reference Ozawa, Yoshida and Hata49–Reference Alexander, Miller and Vargas52) . Eggs are a primary source of dietary cholesterol considering the weak correlation between dietary cholesterol and blood cholesterol, and they are also an affordable and common source of high-quality protein, unsaturated fatty acids, Fe and phospholipids(Reference Soliman53,Reference Wolfe, Baum and Starck54) . Also, eggs were demonstrated to have a protective effect on stroke, which are consistent with the results of our study(Reference Bechthold, Boeing and Schwedhelm41,Reference Ozawa, Yoshida and Hata49,Reference Alexander, Miller and Vargas52,Reference Fallah-Moshkani, Saadatnia and Shakeri55) .
Furthermore, it is necessary to underline moderate to high consumption of fresh fruits and vegetables. Several epidemiological studies have ascertained an inverse correlation between high consumption of fruits and vegetables and stroke risk(Reference Aune, Giovannucci and Boffetta56–Reference Luo, Jiang and Yu58). Fruits and vegetables contain a variety of nutrients and phytochemicals, including fibre, vitamin C, carotenoids, antioxidants, K and flavonoids, which might decrease the risk of stroke through a combination of biological mechanisms(Reference Roman, Jackson and Gadhia47,Reference Ozawa, Yoshida and Hata49,Reference Luo, Jiang and Yu58,Reference Akpalu, Gebregziabher and Ovbiagele59) . Also, a high intake of fruits and vegetables can indirectly decrease the risk of chronic diseases by replacing unhealthy foods high in saturated fat, blood transfusions, glycaemic load and Na. Chinese populations tended to eat vegetables that have been cooked with excessive salt resulting in an increased risk of stroke.
Notably, adherence to a long-term vegetarian dietary pattern is most probably to lead to a decline in immunity, due to the lack of digestible animal protein and fat, resulting in large fluctuations in blood glucose(Reference Poda, Hsu and Rau60,Reference Ou, Chen and Huang61) . Dietary control in patients with diabetes should not be simply considered that low intake and single intake of food were beneficial to participants. Therefore, improving the nutritional status of malnutrition should be encouraged as part of important prevention for stroke patients.
There are some limitations to the study. First, the study sample was selected from Jiangsu province and not representative of the total T2DM patients in China. Thus, this conclusion cannot be generalised to China or even the whole world. Second, this study was not a cohort design; consequently, we could only suggest correlations. We had no access to get reliable inference of causality between dietary patterns and stroke. Thus, further cohort studies are needed in the future to confirm our results. However, we had no access to reveal more robust reliable inferences of causality. Further prospective cohort studies are needed to verify our findings in the future. Third, although some potential confounding factors have been adjusted, the retrospective method of food frequency survey and self-reporting history of diseases cannot avoid the possibility of recall bias and other unknown confounding factors, which may affect the results of the analysis. Fourth, subgroup analysis may destroy the results after PSM, resulting in bias, which makes the conclusions less robust. The results of subgroup analysis can only be used as exploratory analysis to provide clues for studies, and further studies are needed for confirmation in the future.
Conclusions
This study provides sufficient evidence to support the dietary intervention strategies to prevent stroke effectively. In our study, we evaluate whether a particular dietary pattern was correlated with stroke risk in patients with T2DM, adjusting for other known risk factors. Our findings indicated that maintaining a balanced dietary pattern, especially with moderate consumption of high-quality protein food and a high intake of vegetables instead of low consumption of various foods merely, was correlated with a decreased risk of stroke in T2DM patients in China.
Acknowledgements
Acknowledgements: The authors would like to thank all the participants involved in the survey. The authors would also like to thank the Huai´an Center for Disease Control and Prevention. Financial support: This work was supported by the National Natural Science Foundation of China (grant number (82003484)) and Universities’ philosophy and social science researches in Jiangsu Province (2020SJA1053), Natural Science Foundation for Colleges Universities in Jiangsu Province (20KJB330005). Conflicts of interest: None. Authorship: Conceptualisation, W.W. and X.Z.; data curation, C.H.; methodology, W.W. and X.Z.; software, Q.C. and Z.S.; supervision, E.P., Z.S. and P.L.; validation, E.P., Z.S. and P.L.; writing – original draft, C.H.; writing – review and editing, W.W. and X.Z.. All authors approved the final manuscript as submitted and are accountable for this work. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all the research procedures were approved by the Research Ethics Committee of the Huai´an Center for Disease Control and Prevention and Xuzhou Medical University. All participants provided written informed consent.