On 11 March 2020 the World Health Organization (WHO) declared the outbreak of COVID-19 to be a global pandemic.1 By 10 November 2020 there were 50 266 033 confirmed cases of COVID-19 worldwide, with 1 254 567 deaths reported to the WHO.Reference World Health Organization2 The immediate medical emergency and subsequent attempts to contain the spread of the virus resulted in many countries adopting local or national lockdowns. The primary focus was on reducing infection and death rates, but the effects of lockdown, home working and social containment on mental health were soon identified.Reference Wang, Pan, Wan, Tan, Xu and McIntyre3,Reference Rajkumar4 However, much of the published data have been obtained from cross-sectional surveys of self-completed questionnaires undertaken at different times during the pandemic, and there is an absence of well-designed, repeated longitudinal surveys.Reference Moreno, Wykes, Galderisi, Nordentoft, Crossley and Jones5 Preliminary findings from these surveys are variable, but in general they have identified increased rates of anxiety,Reference Li, Yang, Qiu, Wang, Jian and Ji6,Reference Cao, Fang, Hou, Han, Xu and Dong7 depressionReference Lei, Huang, Zhang, Yang, Yang and Xu8 and post-traumatic symptoms.Reference Liu, Zhang, Wei, Jia, Shang and Sun9,Reference Tang, Hu, Hu, Jin, Wang and Xie10
In terms of children and young people, the medical consequences of COVID-19 infection are less severe, with hospitalisation and mortality rates tending to be low.Reference Crawley, Loades, Feder, Logan, Redwood and Macleod11 However, the psychological effects of the pandemic and the public health response have created significant pressures which may place children and young people at particular risk.Reference Moreno, Wykes, Galderisi, Nordentoft, Crossley and Jones5,Reference Crawley, Loades, Feder, Logan, Redwood and Macleod11 Educationally, children have had their education disrupted through school closures, online education and uncertainty about examination arrangements.Reference Crawley, Loades, Feder, Logan, Redwood and Macleod11 An unintended consequence of quarantine and enforced isolation is loneliness, a factor that is particularly problematic for children and young people, who tend to be heavily dependent on their peers.Reference Loades, Chatburn, Higson-Sweeney, Reynolds, Shafran and Brigden12 In addition, children may be at increased risk of witnessing domestic violence or directly experiencing abuse as their carers struggle to cope with the cumulative pressures of the pandemic.13
Carers have a key role in protecting and buffering their children from the effects of COVID-19 and lockdown. In addition to their own stresses, arising from uncertainty, disrupted work, reduced personal finances, less social support and health concerns, they also assume additional responsibilities for maintaining family life and for educating their children.Reference Russell, Hutchison, Tambling, Tomkunas and Horton14 It is therefore not surprising that cross-sectional studies have detailed the adverse effects of COVID-19 on the mental health of carers.Reference Russell, Hutchison, Tambling, Tomkunas and Horton14–Reference Spinelli, Lionetti, Pastore and Fasolo16
Although the negative sequelae of COVID-19 on mental health have been detailed, little is known about the potential positive psychological effects of the pandemic and lockdown and whether this might trigger post-traumatic growth.Reference Tamiolaki and Kalaitzaki17,Reference Tedeschi and Calhoun18 Post-traumatic growth is a positive, adaptative process where traumatic experiences are re-evaluated, and a new and positive life narrative developed.Reference Tedeschi and Calhoun18 Typically, post-traumatic growth follows a disruptive physical or psychological trauma that challenges an individual's perspectives, values and roles. Growth arises from the way the event is processed, not from the event itself, and leads individuals to recognise their vulnerability and what they can and cannot control, and to reassess their personal priorities. This leads to the revision and development of new psychological and philosophical beliefs and stimulates growth across three domains: self-perception, interpersonal relationships and life philosophy.Reference Tedeschi and Calhoun19 This can result in changes in five main areas: improvements in relating to others, greater personal strength, positive spiritual change, a greater appreciation of life, and discovering and embracing new possibilities.Reference Tedeschi and Calhoun19
There is evidence that people of all ages who have experienced various types of trauma can identify positive ways in which their lives have changed and that these are related to improved mental health and well-being.Reference Helgeson, Reynolds and Tomich20 Indeed, reviews have identified that up to 50% of those who have experienced a trauma experience some degree of post-traumatic growth.Reference Wu, Kaminga, Dai, Deng, Wang and Pan21 Given the reach of the COVID-19 pandemic and the current focus on negative mental health sequelae, exploration of potential post-traumatic growth and whether this might maintain and promote well-being might be an alternative paradigm to investigate.Reference Tamiolaki and Kalaitzaki17
Our study aimed to investigate the positive psychological effects of the COVID-19 pandemic and lockdown and post-traumatic growth in a particularly vulnerable group, carers of children, in Portugal and the UK.
Method
Design
This project is part of a European study investigating the association between cumulative risk factors and child and parent mental health during the COVID-19 pandemic. The study approval and set-up process resulted in countries starting recruitment at different times. The data presented here are from the UK and Portugal, the two countries who began recruitment during the peak of the first wave of the pandemic. Data were collected during lockdown between 1 May and 27 June 2020, following the period with the highest incidence of new cases and mortality in each country.
The study was cross-sectional and carers of children aged 6–16 years in Portugal and the UK were invited to participate in an online survey evaluating how the carers were coping with COVID-19 and lockdown. The online survey and data collection tool were developed using the Qualtrics online survey tool hosted by the Faculty of Psychology, University of Lisbon. The study was approved by the ethics committees at the Universities of Lisbon (Portugal) and Bath (UK). Recruitment was via social media, email, institutional advertising and websites, with consent provided online. Before giving consent to participate, caregivers received all the information concerning the study's objectives, the voluntary nature of their participation and the anonymity of the data collected.
Measures
Demographic information
Information was collected about carer demographics (age, gender, education and work status), family type (nuclear family), family size (number of children), effects of the COVID-19 pandemic (child home schooled, parents working remotely, reduction in income) and experience of COVID-19 (family or close friend contracted COVID-19).
Caregiver anxiety
To measure caregiver anxiety, we used the Generalised Anxiety Disorder 7-Item Scale (GAD-7).Reference Spitzer, Kroenke, Williams and Löwe22 The GAD-7 is composed of 7 items (e.g. not being able to stop or control worrying). Carers rated each item on a four-point Likert frequency scale, ranging from not at all to nearly every day over the period of the preceding 2 weeks. Higher scores indicate higher levels of anxiety, with a cut-off score of ≥10 representing moderate levels of anxiety suggesting further assessment. The alpha for the current sample was 0.90.
Caregiver well-being
The Warwick–Edinburgh Mental Wellbeing Scale (WEMWBS)Reference Taggart, Stewart-Brown and Parkinson23 was used to measure caregiver well-being. The WEMWBS consists of 14 items that assess positive affect (e.g. ‘I've been feeling confident’) satisfying interpersonal relationships (e.g. ‘I've been feeling close to other people’) and positive functioning (e.g. ‘I've been thinking clearly’). Carers rated each item on a five-point Likert scale (from none of the time to all of the time) over the time frame of the preceding 2 weeks. The total score ranges from 14 to 70, with higher scores indicating higher levels of well-being. A cut-off of ≤40 has been found to indicate a high risk of depression.Reference Taggart, Stewart-Brown and Parkinson23 The alpha for the current study was 0.92.
Post-traumatic growth
This was assessed via a single open question: ‘Do you think there are any positives to come out of this pandemic and the social distancing restrictions?’.
Data analysis
Quantitative data were summarised with descriptive statistics. Student's t-tests explored differences between scores on standardised questionnaires, with non-parametric χ2-tests examining categorical data. Qualitative data were subject to thematic analysis.Reference Braun and Clarke24 Responses were transcribed verbatim as the researchers familiarised themselves with the data. The responses were then divided into short segments, which were coded according to complementary deductive and inductive processes. There was no a priori coding framework, and the researchers were masked to the specific domains of post-traumatic growth during coding. An initial reading of all codes allowed a first definition of emerging themes. Themes were reviewed by two of the authors (A.I.P. and L.B.) and were refined through multiple iterations until final agreement and data saturation were reached. A Portuguese researcher (A.I.P.) checked the classification for codes produced by Portuguese participants and the English researcher (P.S.) verified those for British participants. Whenever there was a disagreement, a third researcher would resolve it. After codes were finalised, descriptive statistics were calculated to evaluate the absolute and relative frequency of each theme using each participant as a unit of count. A χ2-test of independence was performed to examine the relation between the country (Portugal and UK) and each theme.
Finally, Spearman correlations evaluated the relationship between the perception of positives and carers’ mental health.
Results
Demographics
The participants (Portuguese, n = 185; UK, n = 200) were predominantly mothers (n = 341, 88.6%), aged 40–49 years (n = 226, 58.7%), living in an intact nuclear family (n = 307, 79.7%), with one or two children (n = 333, 86.5%) (Table 1).
Table 1 Demographics and COVID-19 experience of carers of children in Portugal (n = 185) and the UK (n = 200)
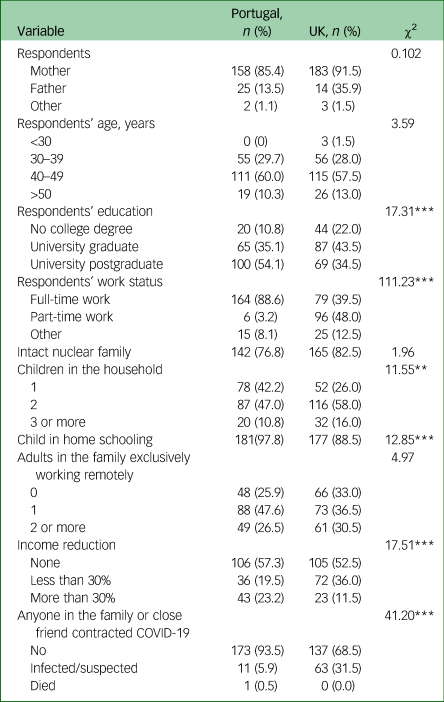
*P < 0.05; **P < 0.01; ***P < 0.001.
The majority were working exclusively from home (n = 271, 70.4%). Almost half reported a reduction in income (n = 174, 45.2%), with most children receiving remote schooling (n = 358, 93%). In total, 75 (19.5%) carers reported a family member with suspected or confirmed COVID-19 infection, with this being more likely in the UK sample. Portuguese carers were more likely to have one child residing in their household, to be in full-time employment, to have a postgraduate degree and to suffer a reduction of income of more than 30%.
Anxiety and well-being
Well-being scores (on the WEMWBS) were higher for Portuguese (mean 47.94, s.d. = 7.75) than for UK (mean 45.51, s.d. = 9.05) carers (t 383 = 2.81, P = .005), with 99 carers (25.7%) scoring ≤40, suggesting a risk of depression. There was a between-country difference on the WEMWBS (χ2(1) = 8.61, P = 0.003), with more carers in the UK (n = 64) falling below the threshold than in Portugal (n = 35).
Anxiety scores (on the GAD-7) were also slightly higher in Portuguese (mean 6.90, s.d. = 4.54) than UK (mean 5.98, s.d. = 4.82) carers but this difference was marginal (t 383 = 1.93, P = 0.054). A total of 83 carers (21.6%) scored ≥10 on the GAD-7, suggesting moderate anxiety, but there was no difference between countries (Portugal, n = 43; UK, n = 40; χ2(1) = 0.59, P = 0.44). These results are in line with previous surveys, in which 23% of primary care patients scored ≥10.Reference Spitzer, Kroenke, Williams and Löwe22
Post-traumatic growth
In total, 341 respondents (88.6%) felt that there were positives to emerge from COVID-19 and lockdown, with 309 (80.3%) providing examples. More positives were identified in the UK than in Portugal (χ2(1) = 5.78, P = 0.16). Thematic analysis identified ten categories (Table 2), which were related to four of the five domains of post-traumatic growth. The most commonly cited category related to the development of closer and more meaningful relationships. This was reflected by growth in family relationships (n = 162, 47.5%), described by one participant as ‘closer relationships and a better understanding of each other’. Comments coded under this theme highlighted how carers reported spending more time together as a family, had more involvement in their children's lives, and felt closer and more connected to other family members. A second domain of post-traumatic growth, a greater appreciation of life, was reflected through the reassessment of personal values and priorities (n = 76, 22.3%) and the opportunity to ‘reconsider what's really important in life’. This involved increased appreciation and gratitude for a simpler life, with opportunities for ‘reconnection with small pleasures’ with less consumerism and reliance on material things. Another category reflecting this domain was the adoption of a healthier lifestyle (n = 75, 22.0%) in which ‘life has slowed down’, resulting in less stress and ‘an opportunity to enjoy the garden and the quiet of the day’. The post-traumatic growth domain of spiritual growth involves a greater engagement with fundamental existential issues. Examples were provided in the category of social growth (n = 53, 15.5%), such as ‘people were helping each other more’ and the development of a ‘stronger sense of community’. There was a ‘greater appreciation of others’ (e.g. healthcare workers) and an ‘acknowledgement of inequalities’. Others identified wider environmental benefits (n = 52, 15.2%) through ‘less car use’ creating less air pollution, which was ‘better for the environment’. The fourth domain of post-traumatic growth, discovering and embracing new possibilities, was reflected in comments about changes in working practice (n = 38, 11.1%), involving positive ‘changes in attitudes to home working’ and the adoption of a ‘better work–family balance’. It was also reflected through opportunities to learn or develop new skills (n = 22, 6.5%), particularly ‘acquiring new technology-related competencies’. Respondents highlighted these as particularly important as they increasingly relied on technology for work, educating their children and socialising. Others described the positive opportunity to home educate their children (n = 10, 2.9%), with one carer reporting that ‘I have always wanted to home school but cannot afford to […] this has been a wonderful experience’. Finally, there were a few examples that were more descriptive rather than indicative of post-traumatic growth. A few mentioned disease control (n = 17, 5.0%) and the ‘benefits of the quarantine and social distancing to avoid or control the spread of the coronavirus infection’. Finally, a few commented on financial benefits (n = 6, 1.8%) where ‘staying home helped to save money’.
Table 2 Post-traumatic growth themes identified by carers of children in Portugal (n = 157) and the UK (n = 184)
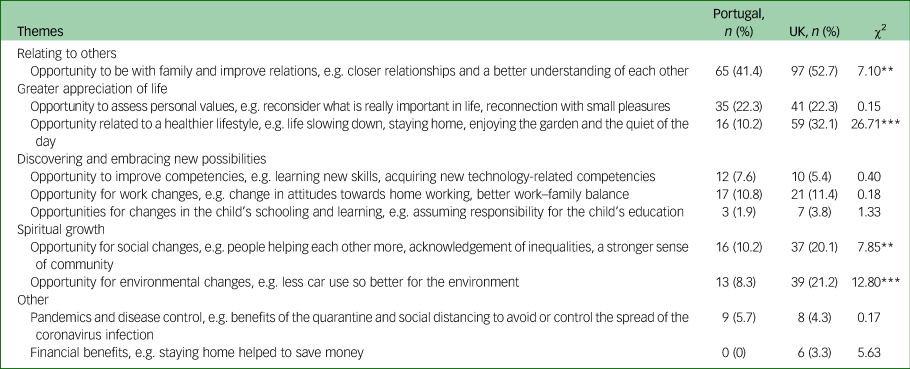
*P < 0.05; **P < 0.01; ***P < 0.001.
Post-traumatic growth, well-being and anxiety
The number of positives identified was correlated with less carer-reported anxiety (r = –0.15, P = 0.003) and improved well-being (r = 0.17, P = 0.001). A comparison of those who did (n = 341) and did not (n = 34) report any positives found a significant difference in well-being scores (t 373 = 2.24, P = 0.025) but not in anxiety scores (t 373 = 0.75, P = 0.45). Those who failed to identify any positives had lower well-being scores (mean 43.56, s.d. = 8.61) than those who identified positives (mean 47.00, s.d. = 8.51).
Discussion
Our survey was undertaken during lockdown as the death rate from COVID-19 was peaking. Carers reported severe disruption to work and their children's education; almost half reported a reduced income, and one in five reported suspected or actual family COVID-19 infection. Despite this adversity, the majority identified positives arising from the pandemic and lockdown, with most examples suggesting evidence of post-traumatic growth reflected in changes in behaviour or cognition. These related to the post-traumatic growth domains of relating to others, a greater appreciation of life, discovering and embracing new possibilities and positive spiritual change. We found no clear evidence of the fifth domain, relating to increased personal strength.
The rates of post-traumatic growth reported here are higher (88.6%) than those reported in reviews looking at growth following a range of traumas (52.6%)Reference Wu, Kaminga, Dai, Deng, Wang and Pan21 or recent studies of nurses during the COVID-19 pandemic (39.3%).Reference Chen, Sun, Chen, Jen, Kang and Kao25 Possible explanations for this difference could be threefold. First, this may reflect our reliance on a single open-ended question to assess post-traumatic growth rather than an established multi-question inventory such as the Post-Traumatic Growth Inventory.Reference Tedeschi and Calhoun19 Second, our criteria for identifying post-traumatic growth only required the identification of a single event. The criteria for determining possible post-traumatic growth using standardised questionnaires are typically based on cumulative scores where a number of items must be identified. Finally, our open-ended question may have facilitated post-traumatic growth by prompting a positive mindset that encouraged respondents to actively seek and acknowledge positive developments. Our question may therefore have encouraged respondents to identify and cognitively process events in a more positive way, thereby explaining why rates of post-traumatic growth were so high. Nonetheless, the examples provided in our survey were not abstract or idealistic post hoc reconstructions of change but reflected actual changes in behaviour typically as a response to the physical limitations imposed by the lockdown. Further studies involving follow-ups are required to substantiate these findings and to determine whether these changes become established and persist once lockdown is eased.
Strengths and limitations
Our study is one of the first to explore benefit finding and potential post-traumatic growth arising from the COVID-19 pandemic and lockdowns. The prospective nature of our study is a strength, with data collected in real time during the peak of the pandemic. However, our study does have a number of limitations that need to be acknowledged. First, we report on a small, convenience sample of volunteers and our cohort is therefore not representative of the general population. Indeed, our sample primarily comprised highly educated mothers living within an intact nuclear family. Second, the cross-sectional nature of our design limits the conclusions that can be drawn. Although we can describe our data at a single point in time, we are unable to draw any conclusions about the nature of relationships or how these might change over time. Third, benefits and potential post-traumatic growth were assessed by a single item, not by a validated questionnaire of post-traumatic growth. Although this limitation is acknowledged, our qualitative approach did allow respondents to disclose their experiences and thoughts without constraint. Similarly, given the online delivery of the survey, respondents could easily have skipped this question if they felt it was not relevant or applicable. Given that our qualitative analysis identified core categories commonly reflected in the post-traumatic growth literature adds to the strength and validity of our findings.Reference Tedeschi and Calhoun19
Implications
The positives that participants identified as arising from the COVID-19 pandemic were associated with less anxiety and improved well-being, raising the possibility that post-traumatic growth might mitigate some of the adverse psychological effects of the pandemic. However, our findings need to be interpreted with caution, since our study has a number of methodological limitations. Further research exploring possible post-traumatic growth following the pandemic and the potential positive effects on mental health is warranted.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available because they contain information that could compromise the privacy of research participants.
Author contributions
All authors contributed to the conception and design of the study, analysed the data, and drafted, revised and approved the final manuscript.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
None.








eLetters
No eLetters have been published for this article.