Compulsory community treatment orders (CTOs) enable psychiatric treatment to occur in the community without the requirement for the patient's consent. A key goal of CTOs is to prevent readmission to psychiatric hospitals for people with severe mental illness and associated risks.Reference Callaghan and Newton-Howes1 CTOs are controversial because treatment is enforced during times when patients may be stable and free of symptoms. Three randomised controlled trials (RCTs) that evaluated CTOsReference Swartz, Swanson, Wagner, Burns, Hiday and Borum2,Reference Steadman, Gounis, Dennis, Hopper, Roche and Swartz3,Reference Burns, Rugkåsa, Molodynski, Dawson, Yeeles and Vazquez-Montes4 were identified by a Cochrane review.Reference Kisely, Campbell and O'Reilly5 Swartz et al concluded that individuals treated under a CTO of longer than 6 months duration had reduced hospital admissions and total hospital days when combined with intensive treatment.Reference Swartz, Wilder, Swanson, Van Dorn, Robbins and Steadman6 Steadman et al evaluated court-ordered treatment including enhanced services compared with an enhanced service package alone and reported that there were no differences between the two groups on all major outcome measures.Reference Steadman, Gounis, Dennis, Hopper, Roche and Swartz3 The OCTET study randomised patients with psychosis to limited or extended compulsory community treatment and reported that the imposition of extended compulsory supervision did not reduce the rate of subsequent readmission.Reference Burns, Rugkåsa, Molodynski, Dawson, Yeeles and Vazquez-Montes4 However, the Cochrane review concluded that the quality of RCT evidence evaluating CTOs was low to moderate and that CTOs did not result in clear differences for the majority of outcomes considered.Reference Kisely, Campbell and O'Reilly5 Each of the RCTs has limitations that prevent their findings being translated into clinical practice. The limitations that are highlighted include the exclusion from study entry of patients with significant concerns relating to violence, study sample attrition and the confounding effects of providing enhanced care as part of the study design.Reference Kisely, Campbell and O'Reilly5,Reference Rugkåsa, Dawson and Burns7 Cohort studies provide an alternative means of assessing the outcomes of CTOs. In cohort studies, patients can act as their own controls and outcome measures are compared on and off CTOs. In general, studies of this type report that CTOs are associated with increased community care and medication and reduced hospital admissions, although these are not universal findings.Reference Rugkåsa, Dawson and Burns7,Reference Kisely, Xiao and Preston8
Evidence to date does not help clinicians in deciding which patient groups most benefit from CTOs. Although the typical patient treated under a CTO has a diagnosis of schizophrenia or mood disorder,Reference Barkhuizen, Cullen, Shetty, Pritchard, Stewart and McGuire9,Reference Dey, Mellsop, Obertova and Jenkins10 the full breadth of psychiatric diagnoses are eligible in most jurisdictions. It is possible that CTOs are associated with different clinical outcomes depending on patient diagnosis. In New Zealand, compulsory treatment of mental illness is administered under the Mental Health (Compulsory Assessment and Treatment) Act 1992.11 Compulsory in-patient and community treatment occurs if patients are ‘mentally disordered’, defined as an abnormal state of mind of such a degree that it poses serious dangers to self or others, or seriously diminishes the capacity for self-care.11 Patients are required to accept treatment in the community when on CTOs. However, active refusal of medication in the community may result in a psychiatric admission as opposed to being enforced in the community. We previously reported the effectiveness of CTOs in New Zealand using routinely collected data from large databases.Reference Beaglehole, Newton-Howes and Frampton12 CTOs were associated with increased community care and increased dispensing of psychiatric medication. CTOs were also associated with clinically significant reductions in admission frequency and admission length for patients with psychotic disorders. Diagnosis was categorised according to psychotic disorder status, as we were focused on evaluating the impact of a range of moderators (age, gender, ethnicity, sociodemographic deprivation and diagnosis) on outcome. The association between CTO status and admissions for psychotic disorders was a novel finding. However, our previous analyses did not examine the impact of diagnosis beyond that of a psychotic disorder. It is possible that other diagnostic groupings have different response signatures to CTOs. For this reason, we chose to expand our previous research and complete this analysis evaluating the impact of diagnosis on clinical outcomes during compulsory community treatment.
Method
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human participants/patients were approved by the Human Research Ethics Committee of the University of Otago (reference number HD19/076). This study analysed large databases. The data were received in anonymised form using unique identifiers. As a consequence, informed consent was not required. Full details of the source data-sets and rationale for outcome measures are provided in our parent paper.Reference Beaglehole, Newton-Howes and Frampton12 Key components are summarised below, along with details relating to diagnosis.
Data-sets
The Programme for the Integration of Mental Health Data (PRIMHD) is the national mental health information collection service for the Ministry of Health (MoH), New Zealand. The PRIMHD data-set records service activity and outcomes for all individuals who receive treatment from public sector secondary healthcare and non-governmental organisation mental health and addiction services.13 PRIMHD data were requested from the MoH for all patients started on a CTO between 1 January 2009 and 31 December 2018. Data were requested in an anonymised form using a unique identifier and included the following:
(a) date and duration of the first CTO (section 29, Mental Health Act 1992) and subsequent CTOs
(b) demographic information
(c) DSM-IV principal diagnostic codes
(d) service use information, including admissions to psychiatric institutions, duration of admissions and out-patient contacts.
The Pharmaceutical Collection is a data warehouse containing the vast majority of dispensing data for New Zealand.14 Psychiatric medication dispensing was requested for patients identified by the unique identifiers provided in the PRIMHD sample. Medications were categorised using the online Pharmaceutical Schedule – November 2019 (a New Zealand database of medications subsidised by the government).
Diagnosis
The PRIMHD database provided the DSM-IV primary diagnoses for patients placed under CTOs during the 10-year study period. Patients could receive multiple diagnoses owing to the potential for repeated contact with specialist mental health services (SMHS) over the study period. For this reason, organising principles were applied to categorise the diagnostic data. We did this using a hierarchical approach to create the following diagnostic groupings: dementia disorders; psychotic disorders; bipolar I disorder; other bipolar disorders; major depressive disorder; personality disorders; other diagnosis; no diagnosis. The DSM-IV codes and diagnoses included in each category are shown in the supplementary material available at https://doi.org/10.1192/bjo.2022.547.
Primary outcome measure
As recommended by Rugkåsa et al,Reference Rugkåsa, Dawson and Burns7 we chose the number of psychiatric in-patient admissions per year on a CTO compared with the number of psychiatric in-patient admissions/year off CTOs to be the primary outcome measure. Admissions are a proxy measure for the effectiveness of community treatment. Admissions were required to be of greater than 48 h to exclude brief admissions for administering depot antipsychotic medication because of refusal to accept treatment in the community. Patients cannot be restrained for medication in the community, so brief admissions may be required to administer medication despite unwellness not being present.
Secondary outcomes
(a) The number of psychiatric admission days/year during a CTO compared with psychiatric admission days/year off CTOs.
(b) Number of community contacts during a CTO compared with contacts off CTOs. Community contacts included input from specialist mental health services and non-governmental organisations. Phone contacts, ‘did not attend’ appointments and care coordination phone calls were excluded.
(c) Rates of psychiatric medication dispensing during a CTO compared with rates of medication dispensing off CTOs.
Statistical analysis
The study population according to diagnostic grouping is described using standard descriptive statistics. Multiple pairwise comparisons were used to examine between-diagnostic group differences.
The incidence of the key outcome measures for each of the diagnostic groups was calculated for the periods on and off CTOs. Individual data were aggregated according to CTO status. The grouped period for patients on CTOs was compared with the grouped period for patients off CTOs. This involved calculating the person-years represented for each individual on and off CTOs over the total study period. The total number of relevant outcome events both on and off CTOs for each individual were then summed to calculate the rates on and off CTOs. A rate ratio (RR) was calculated using these incidences by dividing the incidence of the outcome measure on CTOs with the corresponding figure off CTOs. An RR < 1 means that the outcome is less likely on CTOs and an RR > 1 means the outcome measure is more likely on CTOs. The 95% confidence intervals for the incidence and ratio estimates were calculated using the standard Poisson approximation.Reference Sahai and Khurshid15 Significance was set at P < 0.05. SPSS version 27 for Windows was used for analysis.
Results
In total, 14 726 patients were placed on a CTO at any time during the 10-year period between 1 January 2009 and 31 December 2018. The breakdown of the study population according to diagnosis was as follows: dementia disorders, 2.4% (n = 350); psychotic disorders, 56.6% (n = 8338); bipolar I disorder, 9.5% (n = 1393); other bipolar disorders, 1.4% (n = 212); major depressive disorder, 2.8% (n = 417); personality disorders, 0.7% (n = 106); ‘other diagnosis’, 5.1% (n = 757); and ‘no diagnosis’, 21.4% (n = 3153).
Table 1 reports the characteristics of the study population according to diagnosis. The dementia disorders group (mean age 46.7 years, s.d. = 22.7) was significantly older than the other diagnostic groups (P < 0.01 for all pairwise comparisons). The personality disorders group (mean age 28.9 years, s.d. = 13.9) was significantly younger than the other diagnostic groups (P < 0.01 for all pairwise comparisons) except for the ‘other diagnosis’ group (mean age 29.5 years, s.d. = 15.6, P = 0.70). The mean age for the overall sample was 35.2 years (s.d. = 16.0). Gender breakdown is shown in Table 1. Notably, for personality disorders, 84% were female. The psychotic disorders group was 38.4% Māori ethnicity, which was a higher proportion than in all other diagnostic groups (P < 0.01). In contrast, the major depressive disorder group was 17.0% Māori, a lower proportion than for the other diagnostic groups (P < 0.01). The mean number of CTOs for the diagnostic groups over the study period ranged from 1.9 (major depressive disorder) to 3.0 (psychotic disorders). The psychotic disorders group spent longer on compulsory treatment over the study period (median 631.5 days, IQR = 1546.0 days) than the other diagnostic groups (P < 0.01 for all pairwise comparisons). The major depressive disorder group spent less time on compulsory treatment (median 170.0 days, IQR = 220.0 days) over the study period than other diagnostic groups (P < 0.01 for all pairwise comparisons) except personality disorders (median 182.5 days IQR = 426 days, P = 0.15).
Table 1 Characteristics of the study population according to diagnosis
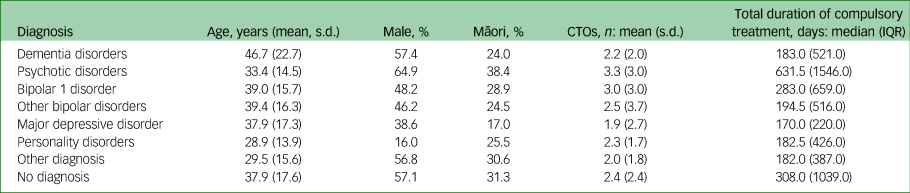
CTO, community treatment order.
Table 2 reports admission frequency/year, psychiatric admission days/year and community psychiatric contacts/year for each of the diagnostic groups according to CTO status and the RRs for these variables.
Table 2 Rate ratios of key outcomes according to diagnostic group

Admission frequency
The psychotic disorders group was the only diagnostic group with less frequent admissions on CTOs (1.00 admissions/year on CTOs compared with 1.22 admissions/year off CTOs; RR = 0.82, 95% CI 0.81–0.83, P < 0.01). All other diagnostic groups had more admissions/year on CTOs (Table 2). The largest RR was for the major depressive disorder group (2.21 admissions/year on CTOs compared with 1.09 admissions/year off CTOs; RR = 2.02, 95% CI 1.87–2.19, P < 0.01). The personality disorders group were admitted more frequently than other diagnostic groups on and off CTOs, with a significantly higher rate on CTOs compared with off CTOs (3.50 admissions/year on CTOs compared with 2.40 admissions/year off CTOs; RR = 1.46, 95% CI 1.31–1.61, P < 0.01). Fig. 1 reports the RR for admission frequency according to diagnostic group in ascending order to demonstrate the variation between diagnostic groups for this outcome measure.

Fig. 1 Rate ratio of admission frequency according to diagnostic group. Error bars represent 95% CIs; the horizontal line highlights RR = 1.
Admission days/year
The psychotic disorders group was the only diagnostic group with fewer admission days/year on CTOs (12.32 days/year on CTOs compared with 15.17 days/year off CTOs; RR = 0.81, 95% CI 0.81–0.82, P < 0.01) (Table 1). All other diagnostic groups had more admission days/year on CTOs (Table 2). The major depressive disorder group had many more admission days/year on CTOs (26.23 days/year compared with 11.87 days/year off CTOs, RR = 2.21, 95% CI 2.16–2.26, P < 0.01). The personality disorders group had the greatest number of admission days/year of any diagnostic group (32.88 days/year on CTOs compared with 24.02 days/year off CTOs, RR = 1.37, 95% CI 1.32–1.41, P < 0.01).
Contacts with community psychiatric services
The number of contacts with community psychiatric services was increased for all diagnostic groups on CTOs (Table 2). The lowest RR was for personality disorders (113.16 contacts/year on CTOs compared with 52.96 contacts/year off CTOs (RR = 2.14, 95% CI 2.10–2.18, P < 0.01). The highest RR was for the ‘other diagnosis’ group (86.09 contacts/year on CTOs compared with 21.17 contacts/year off CTOs (RR = 4.07, 95% CI 4.03–4.10, P < 0.01).
Dispensing of psychiatric medication
Table 3 reports the dispensing of psychiatric medications according to CTO status and diagnostic group. Dispensing of all psychiatric medications was increased on CTOs. This association was most prominent for depot antipsychotic medications. The RR for depot antipsychotic dispensing ranged from 2.85 for the psychotic disorders group to 8.34 for the major depressive disorders group.
Table 3 Rate ratio of psychiatric medication dispensing according to diagnostic grouping

Discussion
We analysed data for all New Zealanders placed on a CTO over a 10-year period and report that there are differing outcomes according to diagnosis. We therefore believe that a more nuanced understanding of outcomes associated with CTOs is required. Our findings direct attention to the likely outcomes for people with a range of diagnoses on CTOs and whether appropriate clinical goals are being achieved with CTO use.
This study repeated our previous finding relating to CTO outcomes for people with psychotic disorders.Reference Beaglehole, Newton-Howes and Frampton12 A psychotic disorder diagnosis was associated with 22% fewer admissions on CTOs and shorter admission days by 2.85 days/year on CTOs. We regard the extent of these reductions in admissions to be clinically significant for patients and services. We suspect that the reduction in admissions results from greater use and adherence to antipsychotic medications. CTOs can therefore be regarded as meeting one of their goals of reducing ‘revolving door’ admissions for this patient group. This finding can be incorporated into evidence-informed discussions between clinicians, patients and family.
No other patient diagnostic group was associated with reduced admission frequency or admission days/year. Despite more contact with community out-patient services and higher rates of psychiatric medication, including depot antipsychotic medications, admission frequency and admission days/year for the other diagnostic groups were increased on CTOs. This finding requires close attention, as a key goal of reducing admissions is not being met.
The bipolar disorder groups had 12% more admissions on CTOs and more than 2 extra days in hospital/year on CTOs. They were also four to five times more likely to be dispensed depot antipsychotic medications. Atypical antipsychotic medications, including risperidone in depot form, are indicated for bipolar disorder and the prevention of mania (although clinical trials have not included non-consenting patients).Reference Boyce, Irwin, Morris, Hamilton, Mulder and Malhi16,Reference Pacchiarotti, Tiihonen, Kotzalidis, Verdolini, Murru and Goikolea17,Reference Malhi, Bell, Singh, Bassett, Berk and Boyce18 Despite this evidence base, their increased use while patients were on CTOs was not associated with less frequent admissions compared with voluntary periods. It appears that increased care and higher dispensing rates for psychiatric medications (including depot antipsychotic medications) were ineffective in sufficiently modifying the course of illness to reduce admissions.
Patients with major depressive disorder were twice as likely to be admitted and had many more admission days/year on CTOs. In addition, the major depressive disorder group was eight times more likely to be dispensed depot antipsychotic medications on CTOs. Although augmentation with second-generation antipsychotics is an option for treatment-resistant depression,Reference Mulder, Hamilton, Irwin, Boyce, Morris and Porter19 depot antipsychotic medications are not usually recommended for the treatment of major depressive disorder.Reference Malhi, Bell, Singh, Bassett, Berk and Boyce18 The extent of the increase in depot antipsychotic dispensing is therefore striking. We assume the major depressive disorder group included patients with treatment-resistant depression and psychotic features. However, the increase in psychiatric medication on CTOs did not modify the course of illness sufficiently to reduce admissions compared with voluntary periods.
The core deficit in dementia disorders is a decline in cognitive function.Reference American Psychiatric Association20 Individuals with a dementia disorder diagnosis treated under a CTO are more likely to be impaired in their decision-making capacity than those with other disorders. In the present study, antipsychotics and sodium valproate were prescribed significantly more while these patients were on CTOs. They were presumably used to treat the behavioural and psychological symptoms of dementia, although evidence for their effectiveness is limited and there are concerns about their side-effect profile.Reference Tible, Riese, Savaskan and von Gunten21,Reference Lee, Gill, Freedman, Bronskill, Hillmer and Rochon22 Again, the higher rates of medication did not modify the course of illness sufficiently to reduce admissions compared with voluntary periods.
The personality disorders group had more frequent admissions on CTOs. Their admission days/year were greater than those for the other diagnostic groups and lengthened further in association with CTOs. Participants with personality disorders were dispensed medications, including depot antipsychotic medication, at much higher rates on CTOs. Treatment guidelines for personality disorders suggest only a limited role for medications.Reference Ripoll, Triebwasser and Siever23,24 In addition, it is generally accepted that longer admissions for patients with personality disorders may be harmful and treatment should largely occur in the community.Reference Paris25 Although clinicians may argue that the complexity of presentation of patients with personality disorders should not preclude treatment under a CTO, our findings suggest that CTOs for personality disorders are associated with more frequent admissions and high rates of compulsory medication. The personality disorders group also received higher rates of community contacts on and off CTOs compared with the other diagnostic groups, suggesting that more intensive management is required for this group than for the other diagnostic categories.
Diagnoses in the ‘other diagnosis’ group included post-traumatic stress disorder, alcohol dependence, opioid dependence, cannabis dependence, and substance induced mood and psychotic disorders (despite the New Zealand Mental Health Act excluding substance use as a basis for providing compulsory psychiatric treatment). This group experienced more frequent admissions, more admission days/year, more community care and greater dispensing of psychiatric medication, including depot antipsychotic medications, on CTOs. Similarly to the other non-psychotic disorder groups, higher rates of treatment on CTOs did not reduce admissions compared with voluntary periods.
We chose admission frequency (excluding brief ‘recall admissions’) to be the primary outcome measure as recommended by Rugkåsa et al.Reference Rugkåsa, Dawson and Burns7 This does not mean we regard admissions in a negative light. We believe them to be an essential part of psychiatric management and often the only solution if community care is progressing poorly. However, we used admissions as a crude proxy for relapse and categorical measure of CTO ‘success’. On this basis, should increased admissions and more admission days/year for the non-psychotic disorder groups be regarded as a failure of CTOs? At first glance, it could be argued that CTOs should not be used for non-psychotic disorder groups because compulsory treatment (including high rates of depot antipsychotic medications) does not result in reduced admissions compared with periods off CTOs.
However, this was not an RCT. Greater degrees of unwellness are likely to be clustered around the times CTOs are used. Increased admissions may therefore simply mark periods of worse mental health which clinicians attempt to contain by using CTOs for individuals who are reluctant to take medication. In this situation, unless the medication is rapidly and reliably effective, it is perhaps not surprising that admissions are more frequent.
For psychotic disorders, compulsory treatment appears effective and reduces admissions, although higher rates of medication use and more community care will not be viewed favourably by all and some will argue that involuntary medication use and care in the community remains unjustified despite apparent clinical benefits. For the non-psychotic disorder groups, compulsory treatments are either less effective or less quickly effective, so that admissions are not reduced on CTOs. The psychotic disorder group in our study spent longer on CTOs than the other groups. Our data do not inform us whether longer periods of compulsory treatment would eventually result in reduced admissions compared with voluntary periods for non-psychotic disorder groups. However, the association between high admission frequency accompanied by high rates of depot antipsychotic medications and community care is a concern in situations where there is not an obvious indication for their use (or if their use does not achieve demonstrable clinical success). We believe that coercive treatments should not be used lightly and their use should be justifiable to others. For patients, compulsory community treatment is accompanied by feelings of coercion and control.Reference Corring, O'Reilly and Sommerdyk26 It is possible that disruption to therapeutic relationships contributes to the lack of treatment efficacy. We therefore recommend that the associations we report for non-psychotic disorders be considered by clinicians and compulsory treatment be reviewed in light of our findings.
The psychotic disorders group had a higher percentage of Māori patients (38.4%) and the depressive disorders group had a lower percentage of Māori patients (17.0%) than the other diagnostic groups. Several factors are likely to affect these findings, including high burden of mental illness among Māori and differential access to treatment.Reference Baxter, Kokaua, Wells, McGee and Oakley Browne27,Reference Metcalfe, Beyene, Urlich, Jones, Proffitt and Harrison28 Our study could not inform us whether systemic biases also contributed to the ethnic variation observed between diagnoses. We anticipate a further paper scrutinising CTOs for Māori more closely.
Limitations
Our study utilised routinely collected data. Unfortunately, symptom or functional outcome scales were not included in the data-set. Although admissions and medication dispensing are readily quantifiable, community care was defined broadly and the quality as opposed to quantity of community interventions provided is unknown. The study was strengthened by the inclusion of all individuals placed on CTOs over the study period. However, individuals were not randomised to CTOs; instead, these were recommended by clinicians and endorsed by judges at CTO hearings. Non-random elements are therefore inherent in the distribution between on CTO/off CTO status. For example, CTOs are more likely to be introduced during times when there is heightened concern about illness and risk, and ceased at other times. Any reduction in admission frequency on CTOs therefore represents a clinical benefit during times when there are greater concerns (as was observed for psychotic disorders). For the diagnostic groups that did not have reduced admission frequency on CTOs, it is possible that admission rates would have been still higher in the absence of a CTO at that time. However, it is clear that the compulsory interventions did not reduce rates compared with the non-compulsory period.
Patients in the ‘no diagnosis’ group comprised 21.3% of the study population. It would be surprising if the majority of these patients were not given clinical diagnoses over the study period. We therefore expect that the absence of PRIMHD diagnoses relates to reporting problems acknowledged to be present in the PRIMHD database.29 Despite this limitation, we regard the positively identified categories to be a sensitive representation of the clinical issues for the individuals represented.
The dementia disorders group had a mean age of 46.7 years. This is younger than expected for a typical dementia cohort. However, in New Zealand, compulsory treatment for dementia is usually provided under a capacity-based legislation called the Protection of Personal and Property Rights Act 1988.30 This enables broader interventions (including financial and physical healthcare) to be applied, unlike the New Zealand Mental Health Act (which only enables compulsory treatment of mental disorder). Consequently, the dementia group in our study are likely to be a heterogeneous group mostly consisting of individuals with pre-senile dementias treated and managed in adult as opposed to older aged services.
We applied hierarchical rules to the diagnostic database to stratify large data into a form that could be analysed according to diagnostic groupings. Readers familiar with DSM-III31 will be aware that this approach is not without precedent, although more recent iterations of the DSM have largely removed the hierarchical approach to diagnosis. We believe that the application of hierarchical rules in this analysis is a sensible and informative way of managing complex information, although we recognise that comorbidity is common and that clinicians will need to translate our findings to inform their approach to complex clinical scenarios.
Our study was situated in New Zealand. The New Zealand Mental Health Act11 applies risk-based criteria to the threshold for compulsory treatment. We think it likely that the CTO signatures observed in our study will be present in countries with similar legislation and recommend other researchers review existing databases to clarify whether our findings are reproduced elsewhere.
Clinical implications
There are specific outcome signatures relating to CTOs according to diagnosis. Rather than asking whether CTOs are effective, we believe that awareness of the likely outcomes for different diagnostic groupings will assist clinicians in making informed decisions about CTOs and in communicating their thinking to patients and families. We believe our research remains supportive of CTOs for patients with psychotic disorders. However, we believe our findings should challenge clinicians to review the use of CTOs for patients without psychotic disorders. The clustering of higher dispensing of psychiatric medications, including depot antipsychotics, alongside more frequent and longer admissions on CTOs is concerning. Although more frequent admissions on CTOs may be a necessary response to difficult clinical scenarios, we believe that an explicit awareness of likely outcomes for different diagnoses has the potential to improve clinical practice in this complex area.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjo.2022.547.
Data availability
On reasonable request the corresponding author, B.B., will support access to the aggregated data-set from which this study is drawn.
Acknowledgement
We thank Fiona Wild from the Ministry of Health, New Zealand, for her support in accessing the data.
Author contributions
B.B. designed the study, reviewed the data, prepared the first draft and completed the final paper. G.N.-H. and R.P. contributed to the study design, reviewed the first draft and contributed to the final paper. C.F. contributed to study design, curated the study data, completed the data analysis and contributed to the final paper.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
R.P. has made use of computer software provided by SBT-pro at no cost for research. He has also received support for travel to educational meetings from Servier and Lundbeck.










eLetters
No eLetters have been published for this article.