Introduction
Schizophrenia spectrum and other psychotic disorders are a heterogeneous group of mental disorders that are characterised by delusions, hallucinations, disorganised thinking, as well as diminished emotional expression and avolition (World Health Organization, 2019). They can severely affect a person's functioning in multiple areas of everyday life and are associated with substantial burden for individuals, carers and the wider society (Velthorst et al., Reference Velthorst, Fett, Reichenberg, Perlman, van Os, Bromet and Kotov2017; Michalska da Rocha et al., Reference Michalska da Rocha, Rhodes, Vasilopoulou and Hutton2018). Although almost 2 million people in Southeast Asia are estimated to meet the criteria for schizophrenia according to the International Classification of Diseases (ICD-10; World Health Organization, 1992) in 2016 (age-standardised point prevalence for Thailand, 2016: 0.28%, 95% confidence interval (CI): 0.24–0.31; Charlson et al., Reference Charlson, Ferrari, Santomauro, Diminic, Stockings, Scott, McGrath and Whiteford2018), reliable epidemiological data remain scarce.
Psychotic experiences – i.e. delusional or hallucinatory experiences – are key symptoms of disorders within the schizophrenia spectrum and other psychotic disorders, although such experiences may also occur in individuals without a diagnosis of mental disorder (van Os et al., Reference Van Os, Linscott, Myin-Germeys, Delespaul and Krabbendam2009; McGrath et al., Reference McGrath, Saha, Al-Hamzawi, Alonso, Bromet, Bruffaerts, Caldas-de-Almeida, Chiu, de Jonge, Fayyad and Florescu2015). The aetiology of psychotic experiences is complex and thought to imply an interplay of genetic vulnerability, neurobiological factors (prominently the activity of the hypothalamic–pituitary–adrenal axis and the dopamine system) and socio-environmental adversities (Morgan et al., Reference Morgan, Charalambides, Hutchinson and Murray2010; Howes and Murray, Reference Howes and Murray2014). Within this framework, stressful or traumatic life events seem to be an important component risk factor for psychotic experiences (Beards et al., Reference Beards, Gayer-Anderson, Borges, Dewey, Fisher and Morgan2013; Gibson et al., Reference Gibson, Alloy and Ellman2016; Mayo et al., Reference Mayo, Corey, Kelly, Yohannes, Youngquist, Stuart, Niendam and Loewy2017). Traumatic events in both childhood and adulthood have been found to be linked to the onset of psychotic experiences across multiple countries (Beards et al., Reference Beards, Gayer-Anderson, Borges, Dewey, Fisher and Morgan2013; Gibson et al., Reference Gibson, Alloy and Ellman2016; McGrath et al., Reference McGrath, Saha, Lim, Aguilar-Gaxiola, Alonso, Andrade, Bromet, Bruffaerts, De Almeida, Cardoso and De Girolamo2017). In a recent multi-country study of cohort data (World Mental Health Survey), the occurrence of any traumatic event was associated with a three-fold higher risk of subsequent first onset of a psychotic experience compared with individuals who did not report traumatic events (McGrath et al., Reference McGrath, Saha, Lim, Aguilar-Gaxiola, Alonso, Andrade, Bromet, Bruffaerts, De Almeida, Cardoso and De Girolamo2017). Furthermore, the risk of psychotic experiences increased in line with the number of traumatic events, suggesting a dose–response relationship. Such a dose–response relationship between the number of traumatic events and the likelihood of psychotic experiences has been already proposed in earlier studies (Scott et al., Reference Scott, Chant, Andrews, Martin and McGrath2007; Shevlin et al., Reference Shevlin, Houston, Dorahy and Adamson2007; Beards et al., Reference Beards, Gayer-Anderson, Borges, Dewey, Fisher and Morgan2013). Furthermore, the few studies that examined different categories of traumatic events suggest that intrusive or interpersonal traumatic events are of particular importance for the development of psychoses compared with unintentional, non-interpersonal traumatic events (Raune et al., Reference Raune, Kuipers and Bebbington2009; Beards et al., Reference Beards, Gayer-Anderson, Borges, Dewey, Fisher and Morgan2013; Solesvik et al., Reference Solesvik, Joa, Larsen, Langeveld, Johannessen, Bjørnestad, Anda, Gisselgård, Hegelstad and Brønnick2016; McGrath et al., Reference McGrath, Saha, Lim, Aguilar-Gaxiola, Alonso, Andrade, Bromet, Bruffaerts, De Almeida, Cardoso and De Girolamo2017). Such interpersonal traumatic events are defined as events that are intentionally caused by other people (e.g. emotional abuse, neglect, abandonment, interpersonal violence and sexual assault), including collective violence (e.g. war and terror).
To date, the bulk of evidence on the association between traumatic events and psychotic experiences comes from countries such as Australia, Europe and North America, with a very limited number of countries from Southeast Asia such as Thailand. The objective of the current study was to address this research gap using data from the 2013 Thai National Mental Health Survey (TNMHS). According to the existing literature, we investigated the following hypotheses:
(1) Thai adults who have experienced at least one traumatic event are at higher risk of reporting psychotic experiences (i.e. hallucinations and delusional experiences).
(2) Interpersonal traumatic events are associated with higher risk of reporting psychotic experiences compared with unintentional, non-interpersonal traumatic events.
(3) There is a dose–response relationship between traumatic events and psychotic experiences, with higher risk for psychotic experiences with an increasing number of traumatic events.
Methods
Data from the TNMHS in 2013 were used, a sub-nationally representative cross-sectional survey that adopted the methodology of the World Mental Health Survey Initiative (Kessler and Üstün, Reference Kessler and Üstün2004). Stratified four-stage probability sampling was applied, including Thai residents (i.e. having a registered address in Thailand for at least past 3 months) aged 18 years or older. Survey weights were provided by the National Statistical Office of Thailand, accounting for the sample weight, non-responses, oversampling of women and elderly and a post-stratification calibration adjustment. Details of the methodology applied in the TNMHS have been published elsewhere (Kittirattanapaiboon et al., Reference Kittirattanapaiboon, Tantirangsee, Chutha, Assanangkornchai and Supanya2016).
The instrument used in the TNMHS was the Composite International Diagnostic Interview (CIDI), a fully standardised interview on mental disorders in accordance with the ICD-10 (Kessler and Üstün, Reference Kessler and Üstün2004). The CIDI records symptoms of a broad range of mental disorders within varying reference periods. In order to apply the CIDI in Thailand, the survey was first translated by a research team of psychiatrists and linguists, and then piloted in clinical and general population samples. Interviews were conducted by trained interviewers who completed a 3-day workshop by instructors certified by the CIDI Training and Reference Centre, Institute of Social Research, University of Michigan.
In the current study, psychotic experiences were defined as reporting at least one experience of visual (‘Have you ever seen something that wasn't there that other people could not see?’) or auditory hallucinations (‘Have you ever heard any voices that other people said did not exist?’), or delusions such as thought insertion and/or withdrawal, mind control and/or passivity, ideas of references, plot to harm and/or being followed during lifetime, after excluding the possibility of dreaming or the influence of substances (‘not dreaming, not half-asleep, or not under the influence of alcohol or drugs’). Furthermore, respondents were asked whether they had ever experienced one or more traumatic events (for all traumatic events considered in this study, see Table 1). We distinguished between interpersonal (e.g. being kidnapped and sexual abuse) and unintentional, non-interpersonal traumatic events (e.g. traffic accidents and sever child illness) (Maercker, Reference Maercker2013). Traumatic events that were not specified or disclosed or that could not be clearly assigned to either category were not considered in analyses where the types of traumatic events were included (see Table 1). Lifetime post-traumatic stress disorder (PTSD), any past-year depression and any past-year anxiety disorder according to ICD-10 (World Health Organization, 1992) were considered as confounders (Isvoranu et al., Reference Isvoranu, van Borkulo, Boyette, Wigman, Vinkers, Borsboom and Investigators2017; Mayo et al., Reference Mayo, Corey, Kelly, Yohannes, Youngquist, Stuart, Niendam and Loewy2017), in addition to the following demographics and socioeconomic indicators (e.g. Fusar-Poli et al., Reference Fusar-Poli, Tantardini, De Simone, Ramella-Cravaro, Oliver, Kingdon, Kotlicka-Antczak, Valmaggia, Lee, Millan and Galderisi2017; Koenen et al., Reference Koenen, Ratanatharathorn, Ng, McLaughlin, Bromet, Stein, Karam, Ruscio, Benjet, Scott and Atwoli2017): gender (women, men), age (continuous), educational attainment (primary or less, junior high, senior high, higher education) and employment status (employed, self-employed, unemployed).
Table 1. Classification of traumatic events into interpersonal and unintentional, non-interpersonal traumatic events

Statistical analysis
Poisson regression models with robust standard error estimation (Rojanaworarit and Wong, Reference Rojanaworarit and Wong2019) were used to examine the association between traumatic events and psychotic experiences. The outcome of interest was the occurrence of at least one psychotic experience during one's lifetime (dichotomous). As independent variable, the experience of at least one traumatic event was considered (dichotomous, hypothesis 1). In order to test hypothesis 2, the same modelling approach was applied considering a categorical independent variable distinguishing between persons who did not experience a traumatic event, experienced at least one unintentional traumatic event, at least one interpersonal traumatic event or experienced both an unintentional and interpersonal traumatic event (four levels). Individuals who did not report interpersonal or unintentional traumatic events, but another, unspecified traumatic event, were excluded in this analysis (4.4% missing). Finally, in order to examine a dose–response relationship (hypothesis 3), the number of traumatic events was taken into account as categorical independent variable with five levels (0, 1, 2, 3, 4 and 5 or more traumatic events).
In order to adjust the regression models, the following control variables were included consecutively: demographic variables (gender, age; model 1), socioeconomic indicators (educational attainment, employment status; model 2) and finally psychiatric disorders (fulfilling diagnostic criteria for PTSD at any time during lifetime, past-year depressive and past-year anxiety disorder; model 3). Additionally, an unadjusted model was used (model 0). Respondents with missing information on either the dependent, independent or control variables were excluded from analyses (N = 12). Survey weights were applied in all regression analyses. All analyses were carried out using Stata 15.1 (StataCorp, 2017).
Ethical approval
The TNMHS was approved by the Ministry of Public Health's Committee for Mental Health and Psychiatric Research in Humans on 21 October 2013 with registration number 77/2556.
Results
Sample characteristics
A total of 4727 adults completed the interview (response rate: 74.3%), of which 4715 aged 44.1 years on average (standard deviation [s.d.]: 23.4 years) constituted the analytic sample (<1% missing). An overview of sociodemographic characteristics of the sample, the prevalence of psychotic experiences, the prevalence of reporting at least one traumatic event and the weighted percentage of persons fulfilling diagnostic criteria for mental disorders (i.e. PTSD diagnosis at any time during lifetime, past-year depressive disorder, past-year anxiety disorder) is displayed in Table 2.
Table 2. Overview of sample characteristics and prevalence of psychotic experiences, traumatic events and mental disorders within the study population (total N = 4715)
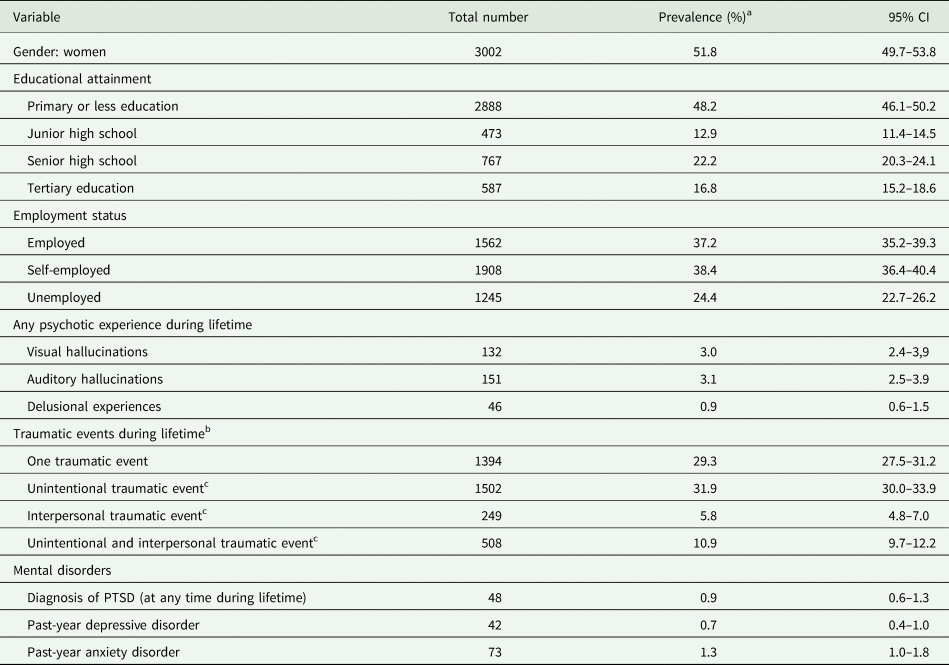
a Survey weights applied to account for the population distribution.
b Numbers do not add up as 21.8% of the participants have experienced more than one traumatic event.
c N = 4506.
About 6% (95% CI: 4.9–7.0) of the respondents reported a psychotic experience during their lifetime, with hallucinatory experiences being more prevalent than delusional experiences. One in two respondents reported at least one traumatic event during their lifetime, with 12.8% (95% CI: 11.5–14.2) reporting two, 5.3% (95% CI: 4.5–6.4) three, 1.9% (95% CI: 1.5–2.5) four and 1.7% (95% CI: 1.3–2.3) five traumatic events. Unintentional, non-interpersonal traumatic event were reported more often than interpersonal traumatic events. On average, the first traumatic event was reported at the age of 26.1 years (s.d.: 19.5 years), with almost two-fifths reporting having been under the age of 18 (38.0%, 95% CI: 35.1–40.9; N = 2444, 1.2% missing). Almost 1% (0.9%, 95% CI: 0.6–1.3) of the respondents met the criteria for PTSD at any time during their lifetime.
Traumatic events and psychotic experiences
Results of the Poisson regression models conducted for hypotheses testing are displayed in Table 3. Respondents reporting at least one traumatic event during their lifetime were around 2.3 times more likely to report a psychotic experience. Taking into account the type of traumatic events, the likelihood of reporting psychotic experiences was similar among respondents experiencing an unintentional traumatic event only and those individuals without any traumatic event. By contrast, respondents experiencing at least one interpersonal traumatic event were around 2.3 times more likely to report psychotic experiences during their lifetime (compared to those without traumatic events). Among those who reported both at least one unintentional and one interpersonal traumatic event, the risk of psychotic experiences was about 4.0 times higher than among those without traumatic event.
Table 3. Results of the Poisson regression models for the association of traumatic events and psychotic experiences for (1) any traumatic event during lifetime and (2) by type of traumatic event
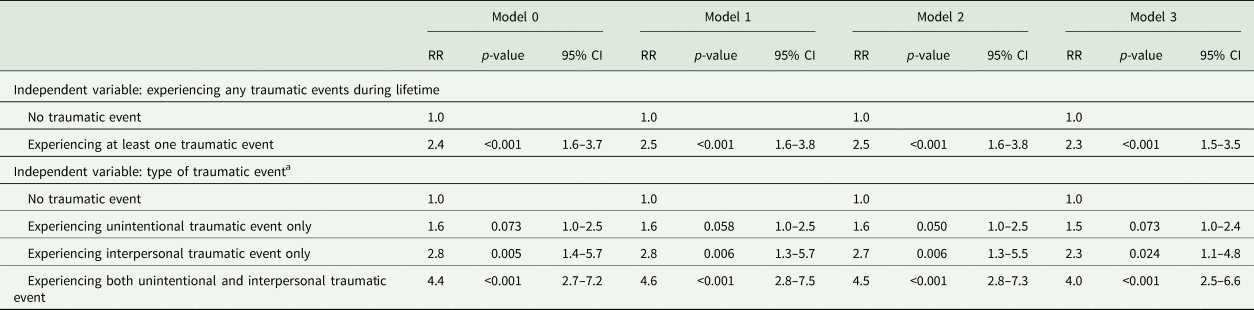
RR, risk ratios; CI, confidence interval.
Model 0: unadjusted model.
Model 1: adjusted for sex and age.
Model 2: adjusted for sex, age, educational attainment and employment status.
Model 3: adjusted for sex, age, educational attainment, employment status, PTSD diagnosis at any time during lifetime, past-year depressive disorder and past-year anxiety disorder.
a N = 4506; 4.4% missing values due to respondents reported an unspecified traumatic event.
The risk of reporting psychotic experiences as a function of the number of traumatic events is shown in Fig. 1. The risk ratios of psychotic experiences in respondents who were exposed to a single traumatic event was not statistically significantly higher than for individuals who were not exposed to a traumatic event (p = 0.103). Beginning with two traumatic events, the risk of psychotic experiences increases with each additional event, with risk ratios of 2.5 (95% CI: 1.5–4.2), 3.7 (95% CI: 2.0–6.7) and 5.9 (95% CI: 3.3–10.7) for two, three and four traumatic events, respectively. Compared with respondents without traumatic event, those who reported five or more traumatic events had 7.7 (95% CI: 4.0–14.8) times higher risk of having at least one psychotic experience during their lifetime.

Fig. 1. Dose–response relationship (risk ratios and 95% CIs) between the number of traumatic events and psychotic experiences. Reference category: no traumatic event. Model adjusted for sex, age, educational attainment, employment status, PTSD diagnosis at any time during lifetime, past-year depressive disorder and past-year anxiety disorder. *p < 0.001.
Discussion
To the best of our knowledge, this is the first study investigating the link between traumatic events and psychotic experiences in the Thai population. In line with previous research, we found an increased risk for psychotic experiences in individuals who have suffered from traumatic events (Scott et al., Reference Scott, Chant, Andrews, Martin and McGrath2007; Shevlin et al., Reference Shevlin, Houston, Dorahy and Adamson2007; Raune et al., Reference Raune, Kuipers and Bebbington2009; Beards et al., Reference Beards, Gayer-Anderson, Borges, Dewey, Fisher and Morgan2013; Solesvik et al., Reference Solesvik, Joa, Larsen, Langeveld, Johannessen, Bjørnestad, Anda, Gisselgård, Hegelstad and Brønnick2016; Mayo et al., Reference Mayo, Corey, Kelly, Yohannes, Youngquist, Stuart, Niendam and Loewy2017; McGrath et al., Reference McGrath, Saha, Lim, Aguilar-Gaxiola, Alonso, Andrade, Bromet, Bruffaerts, De Almeida, Cardoso and De Girolamo2017). Moreover, among individuals who were exposed to either interpersonal or multiple traumatic events (i.e. more than one event), the risk of psychotic experiences was particularly high compared with those who reported a single unintentional or no traumatic event.
The risk of psychotic experiences increased with the number of traumatic events, pointing to a dose–response relationship which is in line with evidence from previous research (Scott et al., Reference Scott, Chant, Andrews, Martin and McGrath2007; Shevlin et al., Reference Shevlin, Houston, Dorahy and Adamson2007; Beards et al., Reference Beards, Gayer-Anderson, Borges, Dewey, Fisher and Morgan2013; Morgan and Gayer-Anderson, Reference Morgan and Gayer-Anderson2016; Croft et al., Reference Croft, Heron, Teufel, Cannon, Wolke, Thompson, Houtepen and Zammit2019). There was no strong evidence of an increased likelihood of psychotic experiences when only a single traumatic event was reported unless this was an interpersonal event. These findings lead us to conclude – without assuming any causality – that the risk of psychotic experiences is generally not increased when a person is exposed to a single unintentional traumatic event. However, when a single traumatic event involved an interpersonal situation, the likelihood of psychotic experiences is increased. According to Morgan and colleagues (Morgan et al., Reference Morgan, Charalambides, Hutchinson and Murray2010; Morgan and Gayer-Anderson, Reference Morgan and Gayer-Anderson2016), adversities in child- and adulthood are key factors in the socio-developmental pathway to psychosis. Exposure to trauma is supposed to interplay with the genetic susceptibility and the dopaminergic system of an individual and to affect its perceptions and cognitions, leading to initial manifestations of a psychosis in some people. Intrusive life events, including interpersonal traumatic events, are proposed to be specifically linked to psychosis (Morgan and Gayer-Anderson, Reference Morgan and Gayer-Anderson2016), which is supported by our findings.
Some limitations have to be taken into account. First, the cross-sectional design of our study does not allow for conclusions about causality. Second, since the TNMHS was conducted in 2013, more research is needed using more recent databases, including other countries in this region, and taking into account longitudinal study designs. Third, psychotic experiences constitute only one symptom of schizophrenia spectrum and other psychotic disorders and may not in all cases lead to clinically meaningful impairment of functioning. Additionally, the TNMHS did not include questions on family history of psychotic experiences, which would have been a key variable given the large genetic component in schizophrenia and other psychotic disorders (e.g. Chou et al., Reference Chou, Kuo, Huang, Grainge, Valdes, See, Yu, Luo, Huang, Tseng and Zhang2017; Zwicker et al., Reference Zwicker, Denovan-Wright and Uher2018). Fourth, the regression of the type of traumatic event (hypothesis 2) is not completely independent of the dose–response regression (hypothesis 3), since in the former analysis we have considered one category in which both types of traumatic events are present (i.e. interpersonal and unintended events), i.e. a minimum of two events, which is equivalent to the experience of two or more traumatic events from the dose–response analysis. In this context, it must be taken into account that no information was available on whether the traumatic events were experienced on one or several independent situations. For example, it could have happened that an unexpected death of a loved one (traumatic event 1) occurred in a car accident in which the respondent was personally involved (traumatic event 2). However, we consider the impact of these restrictions on the relevance of our study results to be marginal.
Based on the strong link between traumatic events and psychotic experiences, some researchers call for a distinction to be made between trauma-related psychotic experiences and such experiences in people who were not exposed to trauma (Hardy, Reference Hardy2017; Wearne et al., Reference Wearne, Curtis, Melvill-Smith, Orr, Mackereth, Rajanthiran, Hood, Choy and Waters2020), with major implications for diagnosis and treatment (Alameda et al., Reference Alameda, Rodriguez, Carr, Aas, Trotta, Marino, Vorontsova, Herane-Vives, Gadelrab, Spinazzola and Di Forti2020). Research investigating potential causal pathways of the association between trauma and psychosis found dissociation – a symptom of post-traumatic stress – to be associated with psychotic experiences (Longden et al., Reference Longden, Branitsky, Moskowitz, Berry, Bucci and Varese2020; Wearne et al., Reference Wearne, Curtis, Melvill-Smith, Orr, Mackereth, Rajanthiran, Hood, Choy and Waters2020) and may be a putative mechanism underlying the association (Perona-Garcelán et al., Reference Perona-Garcelán, Carrascoso-López, García-Montes, Ductor-Recuerda, López Jiménez, Vallina-Fernández, Pérez-Álvarez and Gómez-Gómez2012; Varese et al., Reference Varese, Barkus and Bentall2012; Schalinski et al., Reference Schalinski, Breinlinger, Hirt, Teicher, Odenwald and Rockstroh2019; Alameda et al., Reference Alameda, Rodriguez, Carr, Aas, Trotta, Marino, Vorontsova, Herane-Vives, Gadelrab, Spinazzola and Di Forti2020). Additionally, trauma-related beliefs as well as negative cognitive schemas may serve as such putative mechanisms (Alameda et al., Reference Alameda, Rodriguez, Carr, Aas, Trotta, Marino, Vorontsova, Herane-Vives, Gadelrab, Spinazzola and Di Forti2020; Hardy et al., Reference Hardy, O'Driscoll, Steel, van der Gaag and van den Berg2020). However, the multitude of research undertaken so far is limited by its narrow focus on interpersonal traumatic events and/or childhood adversities, hence studying only specific types of traumatic events, not allowing for a systematic comparison between the risks related to different types of traumatic events. Yet, studies that considered the type (i.e. interpersonal and/or unintentional traumatic events) and the timing of traumatic events (e.g. trauma exposure in childhood, adolescence or adulthood) indicate differences in risk for psychotic experiences across these two aspects (i.e. type and timing of traumatic events; Shevlin et al., Reference Shevlin, Houston, Dorahy and Adamson2007; Schroeder et al., Reference Schroeder, Langeland, Fisher, Huber and Schäfer2016; Croft et al., Reference Croft, Heron, Teufel, Cannon, Wolke, Thompson, Houtepen and Zammit2019; Schalinski et al., Reference Schalinski, Breinlinger, Hirt, Teicher, Odenwald and Rockstroh2019). Our findings concur with previous results and provide further insights into the role of interpersonal trauma and the exposure to multiple traumatic events, which seems to be independent of the type of trauma. Given our study's limitations, we may recommend the following research opportunities for future studies: exploring different types and the timing of traumatic events; distinguishing between traumatic events, in which the person interviewed was either a victim, a perpetrator or both a victim and a perpetrator – a distinction which was not possible in our study; and investigating the trauma–psychosis relationship using a longitudinal study design.
Our findings emphasise the close link between traumatic events and psychotic experiences and extend the existing knowledge to the region of Southeast Asia. Experiencing either an interpersonal trauma or from multiple traumatic events were particularly associated with reporting psychotic experiences during lifetime. In Thailand, almost one in five individuals reported having experienced either an interpersonal trauma or multiple traumatic events in their lifetime, and two in five were minors at the time of first trauma exposure. With a total population of 69.8 million inhabitants in Thailand in 2020 (United Nations, Department of Economic and Social Affairs, Population Division, 2020), about 13 million people would be potentially at risk during their lifetimes. These numbers exemplify the need for effective secondary prevention programmes for people who have experienced interpersonal or multiple traumatic events, particularly for those with a genetic predisposition for psychosis (Fusar-Poli et al., Reference Fusar-Poli, Tantardini, De Simone, Ramella-Cravaro, Oliver, Kingdon, Kotlicka-Antczak, Valmaggia, Lee, Millan and Galderisi2017). According to the World Health Organisation's recommendations within the Mental Health Gap Action Programme to reduce the treatment gap for mental disorders in low- and middle-income countries (World Health Organization et al., 2008, 2015), psychological support should be provided in terms of psychological first aid for those with acute stress following traumatic events (Dua et al., Reference Dua, Barbui, Clark, Fleischmann, Poznyak, van Ommeren, Yasamy, Ayuso-Mateos, Birbeck, Drummond and Freeman2011: 20). Furthermore, prevention (and intervention) programmes may target trauma-related beliefs, negative cognitive schemas or dissociative symptoms, which have been previously found to be putative mechanisms for trauma-related psychosis and distinct from those in non-trauma-exposed persons with psychosis (Alameda et al., Reference Alameda, Rodriguez, Carr, Aas, Trotta, Marino, Vorontsova, Herane-Vives, Gadelrab, Spinazzola and Di Forti2020; Hardy et al., Reference Hardy, O'Driscoll, Steel, van der Gaag and van den Berg2020). Secondary prevention programmes may consider mobile apps or other remote and electronic interventions as an option, as they are easily accessible and preliminary evidence of favourable outcomes and high acceptance in the patient population exists (Vaidyam et al., Reference Vaidyam, Wisniewski, Halamka, Kashavan and Torous2019).
Conclusion
This study was the first to investigate the association between traumatic events and psychotic experiences in a Thai population. We found the experience of interpersonal or multiple traumatic events to be associated with a substantially elevated likelihood of reporting hallucinations or delusions during lifetime. Within our sample, a total of 6% reported having had psychotic experiences at least once in their lives, and one in five respondents stated having experienced interpersonal or multiple traumatic events. The high lifetime prevalence of traumatic and psychotic experiences in the Thai population highlights the need for effective and widely accessible secondary prevention programmes to reduce post-traumatic stress in affected people.
Availability of data and materials
The dataset supporting the conclusions of this paper will be made available upon request to the Bureau of Mental Health Academic Affairs, Department of Mental Health, Ministry of Public Health: dmh.bmha@gmail.com. Syntax used in the statistical analyses can be obtained upon request to the corresponding author.
Acknowledgements
Ulrich Reininghaus was supported by a DFG Heisenberg professorship (no. 389624707). Till Bärnighausen was supported by the Alexander von Humboldt Foundation through the Alexander von Humboldt Professor award, funded by the Federal Ministry of Education and Research, Germany, and the Wellcome Trust, UK.
Financial support
The survey was funded by the Department of Mental Health, Ministry of Public Health, Nonthaburi, Thailand. This study was supported by a DFG Heisenberg professorship (no. 389624707) to UR. Open Access Funding by the Publication Fund of the TU Dresden.
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees in accordance with the Declaration of Helsinki.






