In the UK, revision to the Mental Health Act applying to children and young people admitted to hospital for the treatment of mental illness requires that hospital managers ensure that ‘the patient's environment in the hospital is suitable having regard to his age (subject to his needs)’. 1 Chapter 36 of the Code of Practice to the Mental Health Act specifies that children and adolescents receiving in-patient care for mental illness should have: appropriate physical facilities; staff with the right training, skills and knowledge to understand and address their needs as children and young people; a hospital routine that will allow their personal, social and educational development to continue as normally as possible; and equal access to educational opportunities as their peers, in so far as that is consistent with their ability to make use of them, considering their mental state. 1 There is an expectation that under 18-year-olds will be managed by Child and Adolescent Mental Health Services (CAMHS) specialists, or at least that their treating team will have access to CAMHS expertise. Admission of a person under 16 years of age to an adult unit with persons aged 18 years and older is now considered a reportable ‘serious untoward incident’. Psychiatrists surveyed in the UK reported adverse experiences of young people admitted to adult mental health units such as witnessing a completed suicide and being assaulted by older patients. 2 Admission of young people with mental health problems to paediatric wards raised concern about safety to the patient owing to the limited capacity to restrict access to the means for self-harm, and risks posed by the patient to others owing to the limited capacity to manage dysregulated behaviour. 2 Strategies to improve access to specialist CAMHS care include the development of intensive community treatment services (ICTS), Reference Duffy3–Reference Shepperd, Doll, Gowers, James, Fazel and Fitzpatrick5 more efficient use of specialist CAMHS in-patient resources through greater bed occupancy and shorter lengths of stay, and the establishment of new CAMHS in-patient units. 6 In New South Wales (NSW), the hospitalisation of children and adolescents for mental health reasons is governed by NSW Health Policy PD2011_016, ‘Children and Adolescents with Mental Health Problems Requiring Inpatient Care’. The policy states that children under 12 years requiring acute mental health in-patient care should be admitted to a paediatric ward or to a combined child and adolescent mental health facility within a children's hospital, whereas the preferred option for children aged 12–17 years is admission to a specialist CAMHS unit. Children aged 12–15 years for whom a specialist CAMHS bed is not available may also be admitted to paediatric wards. Other patients under 18 years for whom a specialist CAMHS bed is not available may be admitted to adult acute mental health wards. No lower age limit is specified for such admissions, but the expectation is that the admission should be brief. Since 2002, nine acute CAMHS specialist in-patient units have been opened in NSW. The purpose of this paper is to report trends in the mental health hospitalisation of under 18-year-olds in local health districts (LHDs) which have or have not opened a CAMHS unit, with specific attention to the pattern of separations from non-specialist CAMHS facilities.
Method
We extracted from the NSW state-wide mental health database separation data for under 18-year-olds from specialist CAMHS in-patient units, acute adult mental health in-patient units and paediatric medical units for the period January 2002 to December 2013. Data were extracted in June 2014. There were a total of 22 724 separations from 17 different LHDs in the overall data-set. One LHD was part of an interstate network and these data (n=109) were excluded. Data from the paediatric unit of one LHD were missing; however, the number of missing cases is assumed to be negligible based on number of separations from other units within the same LHD. In total, separation data from 17 NSW LHDs (n=22 615) were available for analysis.
Separations from each type of unit (CAMHS, adult, paediatric) were plotted by LHD in 12 monthly blocks by calendar year to determine the pattern over time. LHDs were classified according to whether they had ever contained a CAMHS unit or not: LHDs 1–7 inclusive contained a CAMHS, adult and paediatric unit, whereas LHDs 9–17 inclusive did not have CAMHS units (supplemental Table DS1). There were some exceptions to this pattern of classification, including LHD 10 which was analysed as though it contained a CAMHS unit because of its close geographical proximity to a CAMHS unit within a neighbouring LHD. Additionally, two CAMHS units were established in children's hospitals which together constitute an LHD in its own right (LHD 8). Adult and paediatric units in LHDs 3, 9 and 10 host overflow from these two CAMHS units. Hence, LHDs 1 through 10 inclusive were classified as Ever-CAMHS, whereas LHDs 11 through 17 inclusive were classified as Never-CAMHS. Sensitivity analyses were run excluding data from LHDs 3, 9 and 10 to ensure that their inclusion as Ever-CAMHS had not biased the results.
Data were analysed using IBM SPSS Statistics Version 22.0. Analyses conducted included descriptive statistics, and two-way repeated measures analysis of variance with sphericity assumed. For descriptive analyses, we noted the date of opening for each new CAMHS specialist in-patient unit (n=9) and examined the flow of under 18-year-olds to adult acute mental health units and paediatric units in the respective LHD in the years prior to and following the opening of each unit.
For inferential statistics, admissions per calendar year for individual LHDs formed the units of analysis. For admissions to adult units and paediatric units, we computed linear, quadratic and cubic trend to determine the difference in slope between Never-CAMHS and Ever-CAMHS LHDs.
NSW Health did not require ethics approval for the project as it comprised an audit of de-identified data released to a unit of the NSW Ministry of Health for the purpose of health service management and evaluation.
Results
Total separations for under 18-year-olds from mental health facilities increased by 258% from 759 in 2002 to 2723 in 2013. For comparison, from 2002 to 2013 the population in NSW aged 0–19 years increased by 4.5% from 1.78 million to 1.86 million. Reference HealthStats7 The proportion of those admitted to adult acute mental health units declined in that period from 71% to 43% but there was a net increase in the number of under 18-year-olds admitted to adult acute mental health units (Fig. 1). The proportion of those admitted to paediatric medical units for mental health reasons declined slightly in that period from 22% to 20% but there was a net increase in the number of patients admitted to paediatric medical units for mental health reasons (Fig. 1). In the Ever-CAMHS LHDs, the proportion of those admitted to adult acute mental health units declined in the same period from 66% to 35%, whereas the proportion of those admitted to paediatric units declined from 25% to 18%.
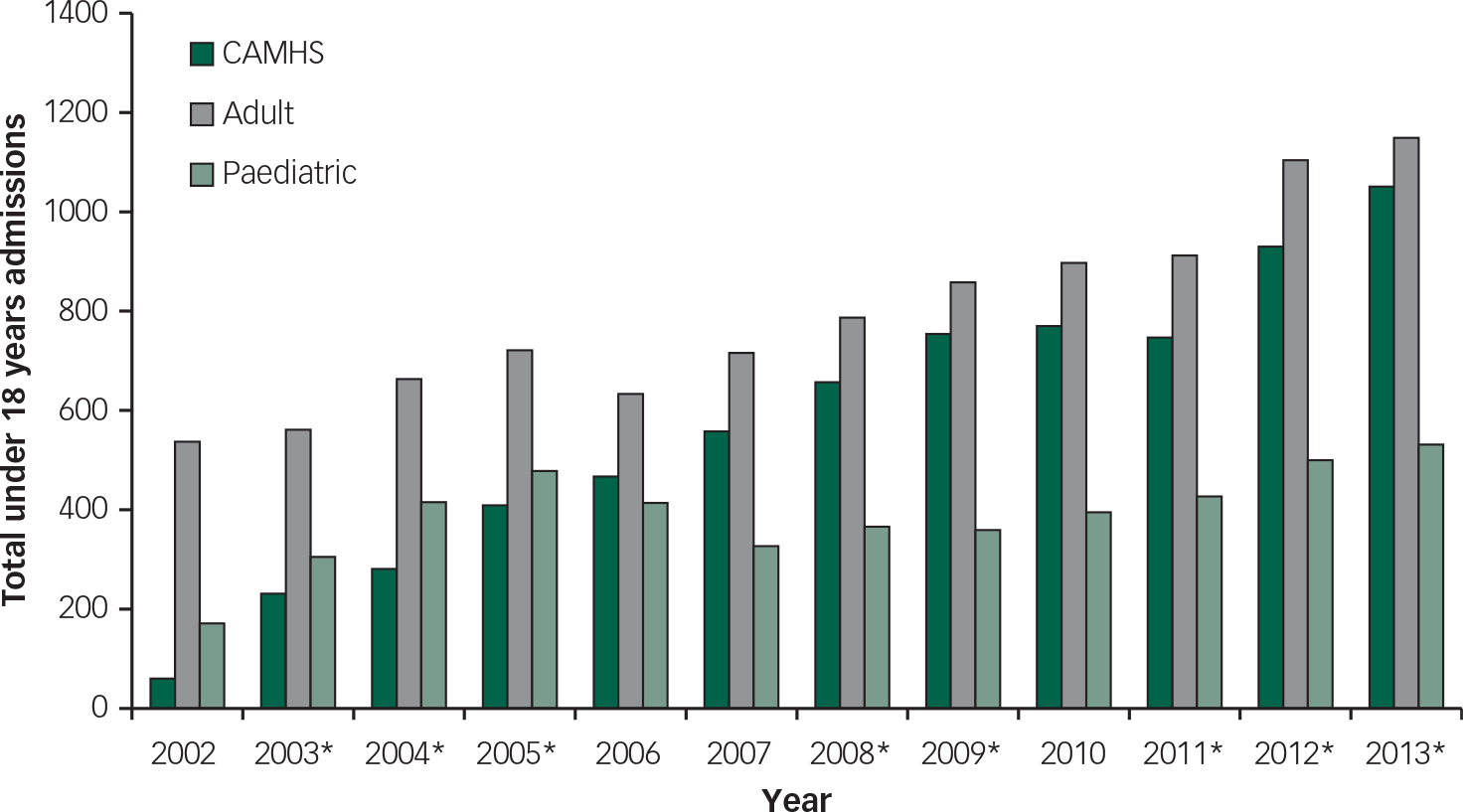
Fig. 1 Total admissions (n=22 615) for under 18-year-olds to in-patient CAMHS, adult acute mental health and paediatric medical units for mental health reasons in NSW from 2002 to 2013. Data are comprised of 16 local health districts (LHDs). Asterisks indicate the year in which a new CAMHS unit opened.
For the period 2002–2013, the mean age of patients admitted to CAMHS units was lower than that for children and adolescents admitted to adult acute mental health units (14.60 years (range 4–17) v. 15.82 years (range 11–17)) and higher than those admitted to paediatric medical units for mental health reasons (13.01 years (range 0–17)). Males made up 30% of paediatric admissions, 33% of CAMHS admissions, and 41% of admissions to adult acute mental health units. Average length of stay was 6.99 days for adult units, 7.38 days for paediatric medical units and 19.03 days for CAMHS units. Frequencies of diagnoses for the overall sample are presented in supplemental Table DS2.
Nine specialist acute CAMHS in-patient units opened during the period January 2002 to December 2013, ranging in capacity from 6 to 12 beds. To investigate trends in child and adolescent admissions to adult mental health units in NSW, we conducted a two-way repeated measures analysis of variance with year and LHD type as independent variables. Mauchly's test indicated that the assumption of sphericity had been violated. However, we elected to report results with sphericity assumed, as the Mauchly's test can be oversensitive. There was a significant effect of time on admissions to adult units, F(11,154)=2.20, P=0.02. There was no significant time by LHD-type interaction, F(11,154)=0.55, P=0.87. Figure 2 depicts the admissions to adult units for Ever-CAMHS (n=9) and Never-CAMHS (n=7) LHDs. The difference in slope for LHD type was not found to be statistically significant for linear, F(1,14)=0, P=0.99, quadratic, F(1,14)=2.40, P=0.14, or cubic trends, F(1,14)=4.53, P=0.05. Analyses were rerun suppressing data from LHDs 3, 9 and 10 as they were classified as Ever-CAMHS on the assumption they accepted overflow admissions from a neighbouring LHD. Re-analysis did not alter the findings.
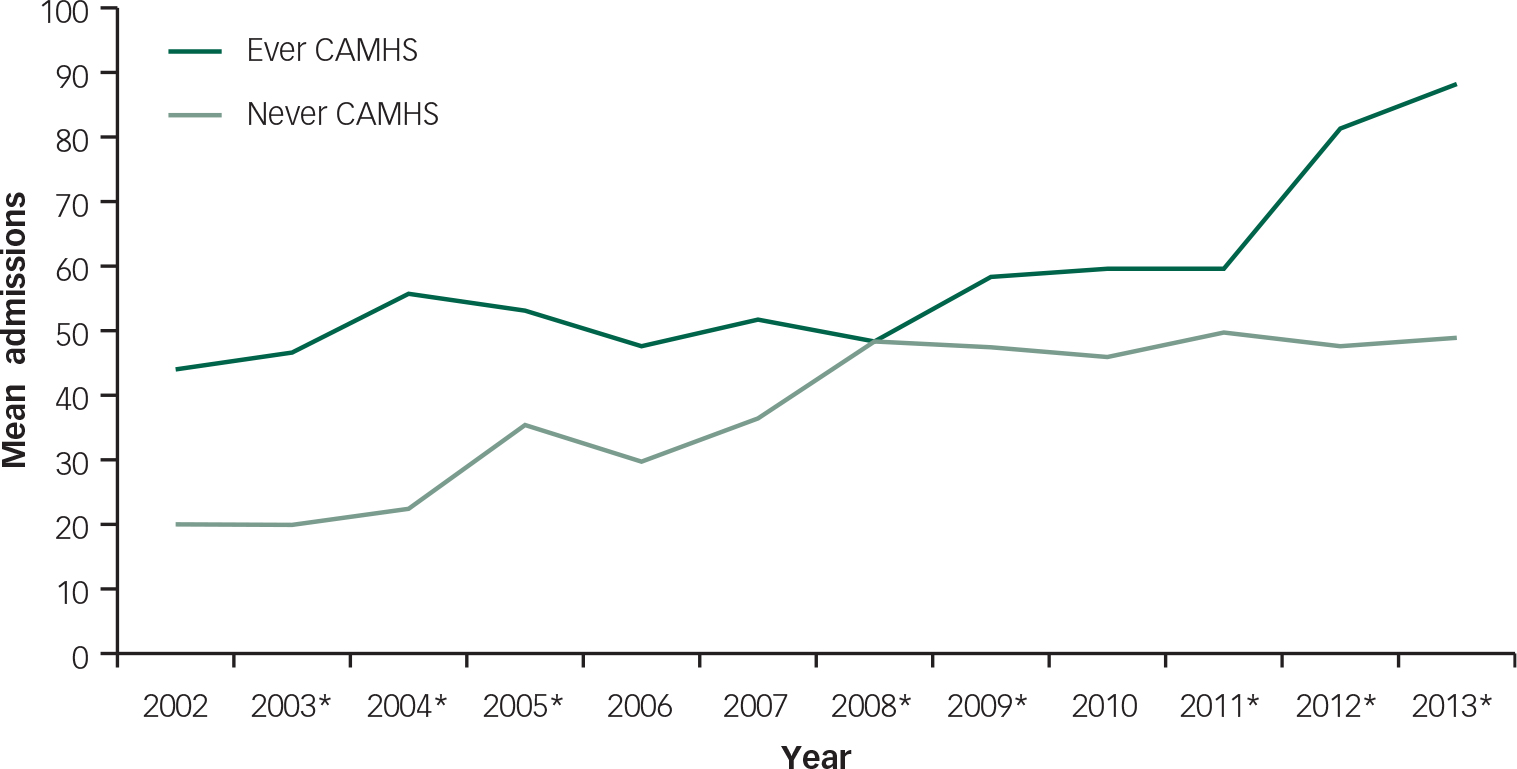
Fig. 2 Mean yearly under 18-year-olds admissions per LHD to adult acute in-patient units by LHD type. Asterisks indicate the year in which a new CAMHS unit opened.
We repeated the analyses for admissions to paediatric medical units. Again, Mauchly's test indicated that the assumption of sphericity had been violated, but we elected to report results with sphericity assumed. Whereas mean admissions appear somewhat higher overall in LHDs hosting a CAMHS unit than those without, the difference did not reach statistical significance, F(1,13)=3.85, P=0.07. The main effect of time was statistically significant, F(11,143)=2.31, P=0.01, but the time by LHD-type interaction was non-significant, F(11,143)=0.26, P=0.99 (supplemental Fig. DS1). The difference in slope for LHD type was not found to be statistically significant for linear, F(1,13)=0.05, P=83, quadratic, F(1,13)=0.01, P=0.94, or cubic trends, F(1,13)=0.33, P=0.58. Analyses were rerun suppressing data from LHDs 3, 9 and 10 as they were classified as Ever-CAMHS on the assumption they accepted overflow admissions from a neighbouring LHD. Re-analysis did not alter the findings.
In the year of opening for CAMHS units (data analysable for eight LHDs), the number of admissions to related LHD acute adult mental health in-patient units compared with the previous year increased by more than 5% for five units, remained stable for two units and decreased by more than 5% for one unit (Table 1). The increases observed exceeded the statewide trend in admissions (see supplemental Table DS3). In the year subsequent to opening, admissions to adult units (data analysable for seven LHDs) increased by more than 5% for four units and decreased for three units. The net effect on admission to adult acute mental health units in the year of opening of a CAMHS unit and 1 year either side (data analysable for seven LHDs) was an increase from 348 to 484 admissions followed by a fall to 401 admissions. It took a further year (data analysable for six LHDs) for admissions to fall back to baseline levels.
Table 1 Number of under 18-year-olds admissions to adult acute mental health in-patient units pre- and post-opening of a CAMHS unit within the surrounding LHD
| LHD | 2 years prior | 1 year prior | Year of opening | 1 year post | 2 years post |
|---|---|---|---|---|---|
| 1 | – | – | 35 | 34 | 23 |
| 2 | 159 | 263 | 251 | – | – |
| 3 | 92 | 82 | 83 | 71↓ | 55 |
| 4 | 25 | 17 | 12↓ | 15↓ | 14 |
| 5 | 38 | 48 | 58↑ | 29↓ | 29 |
| 6 | 42 | 30 | 61↑ | 62↑ | – |
| 7 | 153 | 133 | 209↑ | 154↑ | 120 |
| 8a | 51 | 32 | 41↑ | 50↑ | 67 |
| 8b | 39 | 6 | 20↑ | 20↑ | 32 |
Note: Arrows depict an increase or decrease of >5% relative to the year prior to CAMHS unit opening.
Admissions of children and adolescents to related LHD paediatric medical units for mental health reasons (data analysable for seven LHDs) increased greater than 5% in three units, remained stable for one unit and decreased for three units in the year of opening (Table 2). The increases observed exceeded the statewide trend in admissions (supplemental Table DS4). In the year subsequent to opening, admissions increased for three units, remained stable for two units and decreased for two units. The net effect on admission to paediatric medical units in the year of opening of a CAMHS unit and 1 year either side (data analysable for six LHDs) was a decline from 143 to 130 to 111.
Table 2 Number of child and adolescent admissions to paediatric medical units pre- and post-opening of a CAMHS unit within the surrounding LHD
| LHD | 2 years prior | 1 year prior | Year of opening | 1 year post | 2 years post |
|---|---|---|---|---|---|
| 1 | – | – | – | 27 | 28 |
| 2 | 79 | 100 | 114↑ | – | – |
| 3 | 4 | 3 | 2↓ | 3 | 3 |
| 4 | 47 | 56 | 51↓ | 22↓ | 22 |
| 5 | 41 | 53 | 42↓ | 35↓ | 24 |
| 6 | 7 | 6 | 8↑ | 14↑ | – |
| 7 | – | – | 85 | 142 | 162 |
| 8a | – | 10 | 10 | 11↑ | 11 |
| 8b | 32 | 15 | 17↑ | 26↑ | 17 |
Note: Arrows depict an increase or decrease of >5% relative to the year prior to CAMHS unit opening.
Discussion
The net number of patients under 18 years receiving hospital care for mental health problems in NSW has risen considerably since 2002. Bed capacity in specialist CAMHS in-patients units in NSW has increased, but even in 2013 more patients under the age of 18 received hospital care for a mental health problem outside the CAMHS units than within them. The NSW rate of 43% of child and adolescent mental health admissions going to adult units in 2013 compares with 8% across the UK National Health Service in 2008–2009, 1 19% in Norway in 1993, Reference Sourander and Turunen8 and 31% in Ireland in 2011. 6 Comparable data from other countries are difficult to find, although it is clear from descriptive studies that under 18-year-olds are admitted to adult psychiatric units in, for example, Italy, Reference Pedrini, Colasurdo, Costa, Fabiani, Ferraresi and Franzoni9 New Zealand Reference Park, McDermott, Loy and Dean10 and Sweden. Reference Ostman11 Psychiatrists surveyed in the UK reported a number of factors contributing to the difficulty in accessing specialist CAMHS beds including increase in referrals, decreased capacity of social care, decreased in-patient capacity, decreased community CAMHS capacity, changes in commissioning arrangements, change in clinical need or complexity of patients and decreased capacity for intensive outreach. 2
In five of eight instances, the opening of a specialist CAMHS in-patient unit in NSW was followed by an unintended short-term increase in the number of under 18-year-olds admitted to acute adult mental health in-patient units in the district. An increase in admissions to paediatric medical units was only seen in three of seven districts, and the net effect was a decline in admissions to paediatrics. It may be expected that admission rates to CAMHS units would be low in the first calendar year of opening because generally they will not be open for a full 12 months. In addition, it takes the units months, and sometimes years, to recruit sufficient staff; hence beds may not be fully occupied for some time after opening. However, these factors per se do not explain the temporary surge in admissions to adult units. We speculate that anticipation of the opening of a specialist CAMHS in-patient unit raises the expectation that in-patient care will form part of the overall mental health care of under 18-year-olds with mental illness and that demand for such service outstrips the capacity of the CAMHS unit, leading to overflow admissions to adult units. It is possible that a similar phenomenon has occurred in the UK. Although the rates of child and adolescent admissions to adult units have been favourable compared with NSW, there was in 2013 an upswing in the number of under 18-year-olds treated on adult mental health wards. 12 The upswing occurred despite an increase in specialist CAMHS bed numbers from 1128 in 2006 to 1264 in January 2014, and an improvement in bed occupancy. 12
Our analyses found no significant difference between trends over time in admissions of children and adolescents to adult mental health units between LHDs with Ever-CAMHS and Never-CAMHS. Similarly, our analyses found no significant difference between trends over time in mental health admissions to paediatric medical units between LHDs with Ever-CAMHS and Never-CAMHS. These findings argue against the opening of CAMHS units having a long-term favourable or unfavourable impact on admissions to non-CAMHS facilities. Although a smaller proportion of all juvenile mental health admissions were to non-specialist CAMHS in 2013 than in 2002, the absolute number of admissions to non-specialist CAMHS has risen steadily over the period. In response to a similar situation in the UK, the Royal College of Psychiatrists has made recommendations to reduce the burden on in-patient services of providing mental health care to children and adolescents. 2 The first is to address pressures on other government sectors such as education and social welfare that have ‘knock on’ effects on health services. Second is the strengthening of community CAMHS services. Third is the establishment of ICTS to facilitate early discharge from hospital and planned intensive home treatments. Fourth is financial incentives to encourage community and in-patient CAMHS to work more effectively in partnership. Fifth is the establishment of partnership and safeguarding boards to promote interagency cooperation to mitigate against delayed discharges and delayed admissions. Sixth is investment in crisis services for vulnerable and high-risk children and young people. It is possible that the establishment of ICTS would be a more effective strategy for reducing admissions of under 18-year-olds to acute adult mental health in-patient services than creating more specialist CAMHS beds, as it removes the expectation of admission to hospital. Between the year prior and the year following the establishment of an ICTS for adolescents in the Lothian region of Scotland, the number of under 18-year-olds admitted to adult mental health wards dropped from 20 to 7. Reference Duffy3 Median length of stay in the region's specialist adolescent mental health unit also decreased, from 40 to 30 days. However, reviews of the relative effectiveness of ICTS conclude that there are insufficient quality data to determine whether this form of treatment is a viable alternative to in-patient care. 2,Reference Lamb4,Reference Shepperd, Doll, Gowers, James, Fazel and Fitzpatrick5
Limitations
A study of this nature is dependent on the accuracy of the data that are entered into the state-wide database. During the period of interest there have been adjustments to the boundaries of health districts, meaning that possible admissions to some adult and paediatric medical units have been attributed to different LHDs at different times between 2002 and 2013. To our knowledge, this would have only affected a few small hospitals such that the overall error in a sample of this size would be minimal. We have not made adjustments for the few (n=68) patients whose episode of care involved treatment both by an acute adult mental health unit and a CAMHS unit, as the number is too small to impact on the findings and conclusions. The decision of where to locate CAMHS in-patient units in NSW was strategic. As such, factors that influenced the location of the units such as perceived unmet need may also have influenced the flow of admissions. If those factors are specific to NSW, the findings of the study may not generalise to other jurisdictions.
Implications of the study
These data indicate that in the first year or so after opening a specialist CAMHS in-patient unit it is likely that child and adolescent admissions to acute adult mental health units in the surrounding region will increase. Directors of mental health services need to be aware of this phenomenon and communicate it to service providers and consumers, otherwise newly opened specialist CAMHS in-patient units may be perceived to have failed in their purpose. In NSW at least, the opening of CAMHS units has not influenced the longer term flow of patients to non-CAMHS facilities. CAMHS units appear to fulfil an additional as opposed to replacement role in the care pathway for young people with mental illness. The reduction of admissions of under 18-year-olds to adult units requires strategies in addition to an increase in specialist CAMHS bed capacity.







eLetters
No eLetters have been published for this article.