Introduction
Schizoaffective disorder and schizophrenia are common presentations to psychiatry services and exert great personal, societal and health care costs. These disorders are often studied as a single group, so little is known about variations in admission patterns between them. Greater understanding of how these patients interact with inpatient mental health services would help tailor care offered to these patients. Schizoaffective disorder, in particular, is a very understudied condition in this regard.
In terms of morbidity, it is known that schizophrenia and related disorders can lead to a significant decline in functioning, with 1.7% the of total global years of life lived with disability attributable to schizophrenia (Charlson et al. Reference Charlson2018). Schizophrenia is ranked the 12th most disabling disorder globally (Vos et al. Reference Vos2017), with this burden falling most heavily on low and middle-income countries (Charlson et al. Reference Charlson2018). Schizophrenia is estimated to have a lifetime prevalence of 0.87% (Perälä et al. Reference Perälä2007), with no apparent difference in prevalence between men and women (Saha et al. Reference Saha2005; Perälä et al. Reference Perälä2007; Charlson et al. Reference Charlson2018). The incidence, however, is estimated at 15.2 per 100 000 per annum, with a male-to-female incident rate ratio of 1.40 (McGrath et al. Reference McGrath2004). Higher rates are seen in urban and migrant populations.
By contrast, the lifetime prevalence of schizoaffective disorder is estimated at 0.32%, with prevalence being higher amongst women than men (0.47% v. 0.14%) (Perälä et al. Reference Perälä2007). Identifying a reliable estimate of the incidence of schizoaffective disorder is complicated by frequent changes in its classification in diagnostic manuals over time.
The concept of a disorder with features typical of both schizophrenia and a mood disorder was first described by Kasanin in Reference Kasanin1933. He described these patients as having brief periods of psychotic symptoms, good recovery and better pre-morbid functioning compared to patients with schizophrenia (Kasanin Reference Kasanin1933). Schizoaffective disorder has been classified with psychotic illnesses rather than affective disorders in both the International Classification of Diseases (World Health Organization 1992) and the Diagnostic and Statistical Manual (American Psychiatric Association 2000).
Increasingly, however, there are concerns about the reliability of clinical diagnoses of schizoaffective disorder and its possible overuse in clinical practice. Significant differences are seen between research and clinical diagnoses (Wilson et al. Reference Wilson, Nian and Heckers2014) and inter-rater reliability for the diagnosis of schizoaffective disorder is poor compared to other psychiatric disorders (Maj et al. Reference Maj2000). There is also continued debate about whether schizoaffective disorder, schizophrenia, psychotic mood disorders and bipolar illness represent separate disorders or a continuum (Taylor & Amir Reference Taylor and Amir1994; Möller Reference Möller2003; Lake & Hurwitz Reference Lake and Hurwitz2006; Abrams et al. Reference Abrams, Rojas and Arciniegas2008), with some concluding that all these diagnoses should be viewed as a psychotic mood disorder, with a spectrum of severity of symptoms (Lake & Hurwitz Reference Lake and Hurwitz2006).
Genetic studies suggest a shared genetic risk between schizoaffective disorder, schizophrenia and mania (Cardno & Owen Reference Cardno and Owen2014). Genetic overlap is also seen between schizophrenia and bipolar disorder, although genetic loci differentiating these disorders are similarly identified (Ruderfer et al. Reference Ruderfer2018). Some research suggests a genetic distinction between a more severe psychosis subgroup, with lower levels of functioning, and a higher functioning subgroup with mixed bipolar and schizophrenia diagnoses (Dwyer et al. Reference Dwyer2020). Measuring neurocognitive and perceptual function might better classify patients with schizoaffective disorder, schizophrenia and bipolar disorder into distinct groups, compared to the current diagnostic classification systems (Clementz et al. Reference Clementz2016). Brain imaging does not appear to help differentiate these diagnostic groups either. Grey matter volume across brain regions differ when comparing patients with schizoaffective disorder and schizophrenia to healthy controls, but the two disorders are statistically indistinguishable when compared to each other (Clementz et al. Reference Clementz2016).
Much of the research in this area has focussed on identifying biological differences between patients with schizoaffective disorder and schizophrenia, and the diagnostic reliability of the two disorders. However, variations in admission trends and consequent resource implications are relatively under-researched. Our study seeks to compare the demographic and clinical features of patients admitted voluntarily and involuntarily with diagnoses of schizoaffective disorder or schizophrenia in three psychiatry admission units in Ireland over an 11-year period. In particular, we seek to examine whether the use of involuntary psychiatry admission differs between these two groups.
Materials and methods
Setting
We studied admissions to three acute psychiatry units in Dublin, Ireland (Tallaght University Hospital, Beaumont Hospital and the Mater Misericordiae University Hospital) for periods between 1 January 2008 and 31 December 2018, as part of the Dublin Involuntary Admission Study (DIAS). ‘Admissions’ were analysed as the unit of study and re-admissions of the same patients were not differentiated, that is a patient admitted three times over the study period was examined as three admissions. The acute psychiatry unit at the Tallaght University Hospital serves a catchment area of 273 419 people and has 52 inpatient beds (i.e., 19.0 beds per 100 000 population). The corresponding unit at the Beaumont Hospital serves 247 500 people and has 44 beds (17.8 beds per 100 000 population). The unit at the Mater Misericordiae University Hospital serves 32 869 people and has 10 beds (30.4 beds per 100 000 population). These bed numbers did not change over the study. Admissions to the Mater Misericordiae University Hospital spanned the full 11 years of data collection (1 January 2008–31 December 2018), while the other units were added after the study commenced. Data from the Tallaght University Hospital were collected from 1 January 2014 to 31 December 2018 (5 years) and data from the Beaumont Hospital were collected from 1 July 2014 to 30 June 2015 (1 year).
These units provide general adult and old age psychiatry inpatient services to urban and suburban populations. All three units are part of general hospitals and treat voluntary and involuntary patients, under the Ireland’s Mental Health Act 2001. Ireland’s public mental health service is arranged on a strict catchment area basis, such that all public (i.e., non-fee-paying) psychiatry admissions of individuals’ resident within the geographical catchment area of this service must occur in this admission unit.
In Ireland, involuntary admission and treatment of people with a mental disorder are governed by the Mental Health Act (Mental Health Act 2001), which has been fully operational since 2006. For a patient to be involuntarily admitted under this Act, they must have a ‘mental disorder’, as outlined in Section 3(1) of the legislation; that is, they must have a ‘mental illness’, ‘severe dementia’ or ‘significant intellectual disability’ where (a) ‘because of the illness, disability or dementia, there is a serious likelihood of the person concerned causing immediate and serious harm to himself or herself or to other persons’ (the ‘risk criterion’) or (b) ‘because of the severity of the illness, disability or dementia, the judgment of the person concerned is so impaired that failure to admit the person to an approved centre would be likely to lead to a serious deterioration in his or her condition or would prevent the administration of appropriate treatment that could be given only by such admission’, and ‘the reception, detention and treatment of the person concerned in an approved centre would be likely to benefit or alleviate the condition of that person to a material extent’ (the ‘treatment criterion’) or (c) both (a) and (b).
The involuntary admission process can be instigated by a (a) spouse, civil partner or relative; (b) authorised (designated) officer of the health service; (c) member of the police force; or (d) member of the public (subject to certain conditions). An ‘application’ is made to a general practitioner or other doctors who can then make a ‘recommendation’ that a patient be admitted to the hospital for assessment by a consultant psychiatrist. Within 24 hours of such an admission, the consultant psychiatrist must make a decision as to whether that person will be involuntarily admitted or not. The admission decision is subject to review by a mental health tribunal within 21 days.
Alternatively, a person who already is a voluntary inpatient in an inpatient psychiatry unit and expresses a desire to leave can be retained by a nurse or doctor for up to 24 hours if they think the patient meets the criteria for involuntary care. Within this period, the patient is assessed by two consultant psychiatrists and a decision made about whether their status should change to involuntary; that is, whether or not the voluntary patient undergoes a change of status from voluntary to involuntary (rather than being involuntary from the outset).
Data collection
For all admissions, we recorded gender, date of birth, occupation, marital status, date of admission, date of discharge, legal status and clinical discharge diagnosis. We recorded diagnosis using the International Classification of Diseases (World Health Organization 1992) and created groups of related diagnoses. For patients whose status was involuntary for part or all of their admission, we recorded whether their status was involuntary from the outset or they underwent a change of status from voluntary to involuntary during their admission. We also recorded the dates that involuntary status was commenced and terminated, the legal criteria on which the involuntary order was made and the method by which it was terminated, categorised as follows: (a) involuntary admission order revoked by responsible consultant psychiatrist; (b) involuntary admission order revoked by mental health tribunal; (c) involuntary admission order expired and not renewed; or (d) patient transferred to another hospital while still an involuntary patient.
Statistical analysis
We stored and analysed data using IBM SPSS Statistics (version 26). Data were normally distributed except where specified otherwise. For bi-variable analysis, we used the Student’s t-test and Pearson’s Chi-square test as appropriate. For multi-variable analysis, we performed two binary logistic regression analyses with diagnosis (schizoaffective disorder or schizophrenia) at the dependent variable. Independent variables were the variables that differed significantly between the two diagnostic groups on bi-variable testing. One regression model was for all patients (voluntary and involuntary) with schizoaffective disorder or schizophrenia and one regression model was for involuntary patients only.
Ethical approval
This study was approved by the research ethics committees of the Tallaght University Hospital, Beaumont Hospital and the Mater Misericordiae University Hospital, and was performed in accordance with the Declaration of Helsinki. This was a study of usual practice using existing routine data to evaluate the current mental health service. Data protection legislation was adhered to and the patient confidentiality was protected at all times. Data were stored on a password-protected research computer in a locked research office. Data were irrevocably anonymised and encrypted.
Results
During the study periods, there were 5581 admissions, of which 4723 (84.7%) were voluntary and 856 (15.3%) involuntary. Data collected in Tallaght University Hospital over 5 years spanned 1 367 095 person-years and there were 218.8 admissions per 100 000 person-years. Data collected in Beaumont Hospital over 1 year spanned 247 500 person-years, with 145.5 admissions per 100 000 person-years. Finally, data collected in the Mater Misericordiae University Hospital over 11 years spanned 361 559 person-years, with 411.2 admissions per 100 000 person-years.
Affective disorders were the most common diagnoses amongst all admissions (n = 1671, 30.0%), followed by psychotic disorders (n = 1464, 26.3%), personality disorders (n = 673, 12.1%), drug use disorders (n = 511, 9.2%), neurotic disorders (n = 506, 9.1%), other disorders (n = 433, 7.8%), alcohol disorders (n = 270, 4.8%) and organic disorders (n = 51, 0.9%). Schizoaffective disorder accounted for 4.7% (n = 260) of all admissions, schizophrenia 17.0% (n = 949) and other psychotic disorders 4.6% (n = 255) (Table 1). The proportions of admissions with schizophrenia and schizoaffective disorder to the Tallaght University Hospital, Beaumont Hospital and Mater Misericordiae University Hospital were broadly similar (schizophrenia 17.7%, 22.5% and 15.2%; schizoaffective disorder 5.0%, 5.8% and 4.0%, respectively). The proportions of schizophrenia versus schizoaffective disorder did not differ significantly between the three hospitals (Pearson’s Chi-square =0.237, p = 0.888).
Table 1. Diagnosis and legal admission status of psychiatry admissions in three Dublin psychiatry units over the study periods

On bi-variable testing, compared to admissions with schizophrenia, admissions with a schizoaffective disorder were more commonly female (63.8% v. 29.6%), older (mean age 44.16 years v. 39.13 years) and married (14.7% v. 7.7%), and less likely to be unemployed (69.5% v. 79.3%) (p < 0.001 in all cases; Table 2) or have an involuntary status for all or part of their admission (23.8% v. 37.6%; Pearson’s Chi-square = 17.094, p < 0.001). On multi-variable testing of all admissions (voluntary and involuntary), a diagnosis of the schizoaffective disorder rather than schizophrenia was significantly associated with female gender, voluntary status and older age (Table 3).
Table 2. Comparison of admissions (voluntary and involuntary) with schizoaffective disorder and schizophrenia in three Dublin psychiatry units over the study periods
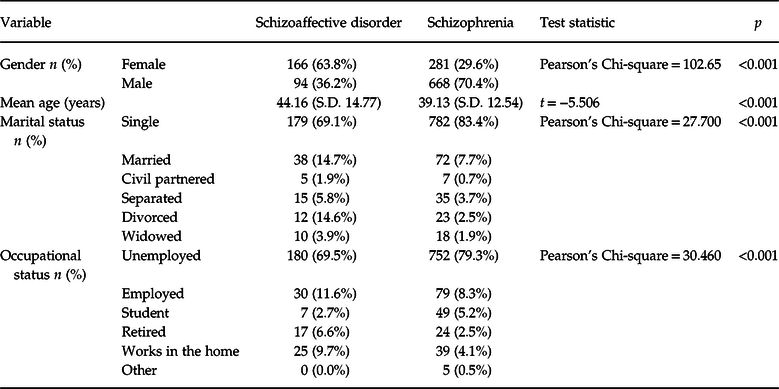
S.D., Standard deviation.
Table 3. Binary logistic regression analysis of correlates of diagnosis amongst admissions (voluntary and involuntary) with schizoaffective disorder and schizophrenia in three Dublin psychiatry units over the study periods
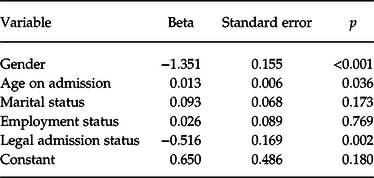
In this binary logistic regression model, the dependent variable was diagnosis (schizoaffective disorder or schizophrenia); the independent variables were variables that differed significantly between the two diagnostic groups on bi-variable testing.
On bi-variable testing of involuntary admissions with schizoaffective disorder or schizophrenia, those with schizoaffective disorder (n = 62) were more likely to be female (53.2% v. 26.1%; p < 0.001) and older (mean age 46.84 v. 37.37 years; p < 0.001), and less likely to be unemployed (72.1% v. 81.7%; p = 0.010) compared to those with schizophrenia (n = 357) (Table 4). Involuntary admissions with schizoaffective disorder did not differ significantly from those with schizophrenia in relation to the legal criteria upon which involuntary admission was based, duration of overall admission, duration of time spent with involuntary status or method by which involuntary admission ended. On multi-variable testing of involuntary admissions, a diagnosis of the schizoaffective disorder rather than schizophrenia was significantly associated with older age and female gender (Table 5).
Table 4. Comparison of involuntary admissions with schizoaffective disorder and schizophrenia in three Dublin psychiatry units over the study periods

S.D., Standard deviation.
Table 5. Binary logistic regression analysis of correlates of diagnosis amongst involuntary admissions with schizoaffective disorder and schizophrenia in three Dublin psychiatry units over the study periods

In this binary logistic regression model, the dependent variable was diagnosis (schizoaffective disorder or schizophrenia); the independent variables were the variables that differed significantly between the two diagnostic groups on bi-variable testing.
Discussion
We found that affective disorders were the most common diagnoses amongst voluntary admissions and psychotic disorders were most common amongst involuntary admissions. This is in keeping with previous studies, which have found an association between psychosis and involuntary admission status (Riecher et al. Reference Riecher1991; Salize & Dressing Reference Salize and Dressing2004) and is also consistent with prior reports from the DIAS (Ng & Kelly Reference Ng and Kelly2012; Curley et al. Reference Curley2016; Umama-Agada et al. Reference Umama-Agada2018; Feeney et al. Reference Feeney2019). In interpreting our findings of differences between admissions with schizophrenia and schizoaffective disorder, it should again be noted that first admissions were not distinguished from re-admissions in this dataset. It is possible that individuals with a high number of re-admissions could have driven statistically significant findings.
Compared to admissions with schizophrenia, admissions with a schizoaffective disorder were more likely to be female (63.8% v. 29.6%), which is consistent with previous literature (Perälä et al. Reference Perälä2007). Admissions with a schizoaffective disorder were also older than those with schizophrenia on both bi-variable and multi-variable testing (mean age 44.16 years v. 39.13 years). Bi-variable testing indicated that admissions with a schizoaffective disorder were more likely to be married (14.7% v. 7.7%), and less likely to be unemployed (69.5% v. 79.3%) compared to those with schizophrenia, suggesting a better social function in schizoaffective disorder (Dwyer et al. Reference Dwyer2020), but these associations were not apparent on multi-variable testing and are therefore not considered further.
Most significantly, we found a difference between the two diagnostic groups in terms of involuntary admission, as significantly fewer admissions with the schizoaffective disorder had involuntary status compared to those with schizophrenia (23.8% v. 37.6%). This suggests that psychotic symptoms might be a stronger driver of involuntary admission than affective symptoms. More specific features of involuntary admission did not differ between the two groups, such as legal criteria for admission, duration of admission, length of time spent as an involuntary patient or method by which involuntary status was revoked.
Our study has several strengths. We focused on a relatively understudied issue; that is, whether there are clinical differences in the ways that patients with schizoaffective disorder and schizophrenia present to, and are treated by, mental health services, especially in relation to specific parameters of psychiatry admission such legal status, duration of admission. We studied a broad range of variables, including gender, age, occupation, marital status, diagnosis, legal criteria for involuntary admission, duration of admission, duration of involuntary care and reason for termination of involuntary status. Our study spans more than a decade of admission data and examines over 5000 admissions.
Limitations include the facts that our research is based in urban and suburban centres in Ireland, which might reduce generalisability; re-admissions were not differentiated from first admissions; we recorded only one diagnosis per patient when some might have had two or more; factors relating to deprivation and social supports were not examined; type of schizoaffective episode (mood or psychotic episode) was not specified; and only data from one of the three units spanned the full study period, limiting potential comparisons. While we focused on comparing patients with schizoaffective disorder and schizophrenia, we did not examine patients with other psychotic disorders (e.g., depression, mania). Some of these other diagnoses might, in time, be revised to schizoaffective disorder or schizophrenia; a more detailed, longitudinal study would be needed to elucidate these issues. Furthermore, as described in the introduction, there are issues in reliably distinguishing schizophrenia from schizoaffective disorder and these should also be considered in interpreting our findings. We also did not examine admission diagnoses in the context of beds per capita. Future research could usefully examine the impact of variability in beds per capita between catchment areas on the diagnostic mix amongst admissions.
Overall, we found that admissions of patients with schizoaffective disorder differ in significant respects from those with schizophrenia. More specifically, admissions with schizoaffective disorder are more likely to be female and older, and less likely to have involuntary admission status, compared to those with schizophrenia. We hypothesise that psychotic symptoms might be a stronger driver of involuntary psychiatry admission than affective symptoms. However, future research examining the relationship between the type of schizoaffective episode and involuntary status is needed to further elucidate if such an association exists.
Acknowledgements
We are very grateful to everyone who assisted with this study.
Conflicts of interest
None.
Ethical standards
This study was approved by the research ethics committees of Tallaght University Hospital, Beaumont Hospital and the Mater Misericordiae University Hospital. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committee on human experimentation with the Helsinki Declaration of 1975, as revised in 2008.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.







