Introduction
Cognitive behavioural therapy (CBT) is probably an efficacious treatment for anxiety disorders and depression, taking into account publication bias, the quality of trials, and the influence of control conditions (Cuijpers et al., Reference Cuijpers, Cristea, Karyotaki, Reijnders and Huibers2016). However, only half of patients with an anxiety disorder achieve remission status post-treatment (Springer et al., Reference Springer, Levy and Tolin2018) and every fifth patient with anxiety, and every third patient with depression, drops out of treatment (Fernandez et al., Reference Fernandez, Salem, Swift and Ramtahal2015).
Motivational interviewing (MI) is a collaborative conversation style for strengthening an individual’s motivation and commitment for behaviour change (Miller and Rollnick, Reference Miller and Rollnick2013). MI may be useful for enhancing CBT because insufficient motivation, often expressed as ambivalence about or resistance to change, is a patient factor that may influence non-response and drop-out (Miller and Rollnick, Reference Miller and Rollnick2013; Westra, Reference Westra2012). MI has been employed as an adjunct to CBT in several studies, and a recent meta-analysis including 12 studies of adult patients with anxiety disorders showed that the combination had a moderate effect on symptom reduction compared with CBT alone (Marker and Norton, Reference Marker and Norton2018). Of the published studies included in the meta-analysis, all used MI as a prelude to CBT, whereas only two studies incorporated additional MI principles throughout treatment, that is, integrated MI and CBT (MI-CBT). Simpson and colleagues (Simpson et al., Reference Simpson, Zuckoff, Maher, Page, Franklin, Foa and Wang2010) found no differences in symptom improvement or adherence to CBT procedures in a small sample of participants with obsessive-compulsive disorder (OCD) who were recruited in a research clinic setting and randomly allocated to CBT alone or MI-CBT. One explanation offered by the authors was that the dose or delivery of MI was sub-optimal, because an MI module was available for use if participants showed signs of decreased motivation only if standard CBT procedures for making participants adhere to treatment were ineffective (Simpson et al., Reference Simpson, Zuckoff, Maher, Page, Franklin, Foa and Wang2010). The authors suggested that a more integrated protocol might have yielded different results. In a well-controlled and adequately powered randomised trial, Westra and colleagues (Westra et al., Reference Westra, Constantino and Antony2016) found that at post-assessment there were no differences in outcomes in participants with generalised anxiety disorder (GAD) who were recruited from the general population and received CBT alone or MI-CBT. However, over follow-up assessments at 6 and 12 months, participants in the MI-CBT condition had benefited more in terms of reduction in worry and general distress. Thus, there are only two studies of MI-CBT for anxiety disorders in adults and none was conducted in routine psychiatric care using regular therapists. There is a paucity of studies of combinations of MI and CBT for depression as the principal diagnosis. This is unfortunate considering that decreased motivation is a significant problem in depression.
Unhealthy lifestyle behaviours related to diet, alcohol use, physical activity or tobacco use are more prevalent in individuals with anxiety disorders and depression than in the general population (e.g. Fluharty et al., Reference Fluharty, Taylor, Grabski and Munafo2017; Zschucke et al., Reference Zschucke, Gaudlitz and Strohle2013). Unhealthy lifestyle behaviours not only contribute to additional suffering, but also increase the risk of chronic medical conditions and premature mortality (e.g. Batelaan et al., Reference Batelaan, Seldenrijk, Bot, van Balkom and Penninx2016). Both MI and CBT are effective in improving lifestyle behaviours and preventing disease (e.g. National Board of Health and Welfare, 2018) and the integration of the treatments may provide additional benefits. Considering the high co-morbidity of unhealthy lifestyle behaviours with psychiatric disorders, a potentially useful approach is to focus on both of these conditions in the same treatment using MI-CBT.
Pilot studies are appropriate if there is uncertainty about future randomised controlled trial (RCT) feasibility (Eldridge et al., Reference Eldridge, Lancaster, Campbell, Thabane, Hopewell, Coleman and Bond2016). The primary aim of the present study was to investigate the feasibility of MI-CBT in preparation for a future RCT designed to assess the effectiveness of MI-CBT in routine psychiatric care. Because there are only two previous studies on MI-CBT for anxiety disorders, there are several uncertainties concerning future RCT feasibility, including recruitment and retention of participants in routine psychiatric care. In addition, feasibility was investigated in terms of therapist competence in MI following a brief training, and participant perceptions of treatment credibility, expectancy for improvement, and working alliance between participants and therapists. Support for progression to an RCT was deemed sufficient if it was able to recruit a reasonable number of participants, they remained in the study, and therapists acquired competence in MI. A secondary aim of the present study was to conduct separate preliminary evaluations exploring the effects of CBT alone for anxiety disorders and depression and of MI-CBT for anxiety disorders, depression, and co-morbid unhealthy lifestyle behaviours. For both treatments, psychiatric symptoms, unhealthy lifestyle behaviours, functional impairment, and quality of life were used as outcome measures. It was expected that MI-CBT would be as feasible as CBT in the above respects and that both conditions would show clinically relevant improvements in outcome measures.
Method
Design
The present pilot trial had a randomised controlled parallel design and was conducted between 2013 and 2015 at a psychiatric clinic specialised in CBT for anxiety disorders and depression in Stockholm, Sweden. Participants were consecutively included in the study and provided treatment. Randomisation was conducted on a 1:1 basis using an online service (www.random.org).
Participants
Inclusion criteria were: (a) 18 years of age or older, (b) a principal diagnosis according to the Diagnostic and Statistical Manual of Mental Disorders (4th edition, text revision: DSM-IV-TR; American Psychiatric Association, 2000) of panic disorder, social anxiety disorder (SAD), OCD, GAD, post-traumatic stress disorder (PTSD), or major depressive disorder, and (c) at least one of the following unhealthy lifestyle behaviours: unhealthy eating habits, hazardous use of alcohol, insufficient physical activity, or tobacco use, according to criteria suggested by the National Board of Health and Welfare (2011). Exclusion criteria were: (a) DSM-IV-TR criteria for psychotic symptoms, (b) DSM-IV-TR criteria for substance abuse other than alcohol, (c) DSM-IV-TR criteria for substance dependence including alcohol, (d) moderate to severe suicide risk according to the Mini-International Neuropsychiatric Interview (MINI; Sheehan et al., Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs, Weiller and Dunbar1998) or a score of 2 or above on item 9 on the Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., Reference Kroenke, Spitzer and Williams2001), and (e) another simultaneous psychological treatment. Participants were recruited by the therapist who conducted diagnostic assessment. The last author assigned participants to treatment.
Treatments
Cognitive behavioural therapy
Disorder-specific CBT protocols were used in both the CBT and MI-CBT conditions, including panic control treatment (Craske and Barlow, Reference Craske, Barlow and Barlow2008) for panic disorder, CBT (Turk et al., Reference Turk, Heimberg, Magee and Barlow2008) for SAD, exposure with response prevention (Franklin and Foa, Reference Franklin, Foa and Barlow2008) for OCD, intolerance of uncertainty therapy (Dugas and Robichaud, Reference Dugas and Robichaud2007) for GAD, prolonged exposure (Foa et al., Reference Foa, Hembree and Rothbaum2007) for PTSD, and behavioural activation (Martell et al., Reference Martell, Dimidjian and Herman-Dunn2010) for depression. To be consistent with routine practice, CBT did not involve a particular focus on unhealthy lifestyle behaviours; rather, therapists were instructed to target such behaviours only to the extent they typically do when practising CBT for psychiatric disorders. Sessions in the CBT condition were conducted on a weekly basis and were typically 45 minutes in length. During the treatment period, therapists in both conditions received supervision in CBT by independent supervisors every third week as part of routine practice.
Integrated motivational interviewing and cognitive behavioural therapy
An integrated model of MI and CBT was developed as part of the present study, based on Miller and Rollnick (Reference Miller and Rollnick2013), Westra (Reference Westra2012), and personal experience of MI training and practice. The model was developed in discussions between the authors only. Participants were treated within an MI framework in accordance with the four processes characterising MI (Miller and Rollnick, Reference Miller and Rollnick2013): (1) engaging patients in a mutually trusting and respectful working relationship, (2) focusing on goals for treatment, (3) evoking and strengthening motivation for behaviour change, and (4) planning and implementing treatment. These processes are overlapping and both sequential and recursive: earlier processes lay the foundation for later processes and continue to run beneath them, and treatment may momentarily return to an earlier process that requires renewed attention (Miller and Rollnick, Reference Miller and Rollnick2013).
The MI-CBT model was compiled in the form of a treatment guide, designed to be used flexibly depending on the individual participant’s motivational state and whether therapist and participant agreed on first to focus on the psychiatric disorder and then to focus on the unhealthy lifestyle behaviour, or vice versa. A third option was to focus on the psychiatric disorder and the lifestyle behaviour simultaneously, as the problems for some patients are functionally related (e.g. alcohol use as a safety behaviour in SAD). In the treatment guide, the first three processes are covered in the first one to three sessions (depending on the patient’s motivational state) and consist of pure MI, whereas the fourth process consists of CBT integrated with MI. Psychiatric disorders were treated according to the CBT protocols and unhealthy lifestyle behaviours were targeted using generic CBT principles and strategies (e.g. functional analysis or case conceptualisation, thought records, stimulus control). Thus, in the treatment guide, the planning and implementation process is the most comprehensive. Planning and implementation are conducted within an MI framework; for example, sessions are client-centred and conducted in an ‘MI sprit’, and patient autonomy is emphasised. Although CBT is at the core of this process, MI principles and strategies are employed whenever patient motivation decreases; on such occasions, treatment may momentarily return to an earlier process. Examples include sub-optimal engagement in exposure (return to evoking) and ruptures in the working alliance (return to engaging). Thus, in contrast to CBT protocols, the MI-CBT guide puts an emphasis on resolving ambivalence and strengthening motivation whenever ambivalence appears, to facilitate behaviour change in anxiety or depression as well as lifestyle behaviours, and to increase adherence to CBT procedures. As in the CBT condition, sessions in the MI-CBT condition were conducted on a weekly basis and were typically 45 minutes in length. During the treatment period, therapists in the MI-CBT condition had access to regular supervision in MI-CBT by the last author.
Therapists
Six clinical psychologists specialising in CBT were randomly allocated to practice CBT (n = 3) or MI-CBT (n = 3). In the CBT condition, one therapist was female, mean age was 31.0 years (range 30–32), mean number of years of clinical experience was 1.3 (range 0–3), two therapists had previous training in MI, and the mean score of competence in CBT on the Cognitive Therapy Scale (CTS; www.beckinstitute.org) was 43.3 (range 30–52). In the MI-CBT condition, two therapists were females, mean age was 39.0 years (range 37–40), mean number of years of clinical experience was 4.7 (range 0–8), one therapist had previous training in MI, and the mean score of competence in CBT was 47.0 (range 37–57).
Training
Therapists in the MI-CBT condition received training in MI. Training was conducted according to research findings of what is required for acquisition of competence in MI; that is, a combination of learning methods, including systematic feedback on performance and supervision (Madson et al., Reference Madson, Loignon and Lane2009; Miller et al., Reference Miller, Yahne, Moyers, Martinez and Pirritano2004). The MI training included five occasions of didactic presentation, a 1-day skills training, systematic feedback on MI performance based on one session coded according to the Motivational Interviewing Treatment Integrity (MITI; Moyers et al., Reference Moyers, Martin, Manuel, Miller and Ernst2010), and four supervision occasions with an independent supervisor who was a member of the Motivational Interviewing Network of Trainers. In addition, therapists in the MI-CBT condition were provided with instructions on how to implement MI-CBT in their practice.
Assessment
Measures used in the present study are well-established and have good psychometric properties. Unless otherwise specified, assessments in participants were administered before and after treatment and 6 months following treatment completion, and higher scores indicate more severe symptoms or unhealthy lifestyle behaviours. All assessments in participants were web-based, except for diagnosis, therapist competence in CBT and MI, and observer-assessed participant motivation for behaviour change. The web-based assessment system included several reminders administered automatically via email and short message service. Upon non-response following reminders, participants were contacted by telephone. Authors were not blind to treatment allocation, while independent raters of competence in CBT and observer-assessed participant motivation were blind. Unless otherwise stated, internal consistency of measures using Cronbach’s α was calculated for the entire sample at pre-assessment.
Therapist competence in cognitive behavioural therapy
Competence in CBT was assessed in therapists in both conditions at the beginning of the treatment period using the CTS. The CTS consists of 11 items, which are rated between 0 and 6. Competence was examined in audio-recorded sessions with patients not participating in the present study. Therapists were instructed to select one patient with whom they judged they could perform as good CBT as possible (assumed to reflect ‘best practice’). A commonly referred to, although not validated, threshold for competence on the CTS is 39 points (Muse and McManus, Reference Muse and McManus2013). One therapist in each condition did not reach this threshold.
Principal diagnosis
The MINI was used to determine a principal diagnosis of an anxiety disorder or depression. Typically, diagnostic assessment was conducted by a therapist other than the one who conducted treatment.
Unhealthy lifestyle behaviours – screening
Definitions of unhealthy lifestyle behaviours suggested by the National Board of Health and Welfare (2011) were used and the Board’s screening items were administered to all potential participants to determine study eligibility. Unhealthy eating habits were assessed using four items measuring the frequency of consumption of some healthy and unhealthy foods. Hazardous use of alcohol was assessed using two items measuring the frequency and amount of consumption, corresponding to items 2 and 3 of the Alcohol Use Disorders Identification Test (AUDIT; Saunders et al., Reference Saunders, Aasland, Babor, de la Fuente and Grant1993). Insufficient physical activity was defined as less than 150 minutes of moderate physical activity or less than 75 minutes of intensive physical activity or less than 150 minutes per week of both in combination. Tobacco use was defined as daily smoking or use of snuff.
Feasibility
To assess competence in MI in therapists providing MI-CBT, the MITI version 3.1.1 (Moyers et al., Reference Moyers, Martin, Manuel, Miller and Ernst2010) was used. The MITI consists of 12 items, which yield six indicators of competence: MI spirit, empathy, per cent complex reflections, per cent open questions, reflection-to-question ratio, and per cent MI-adherent behaviours, each with specified thresholds for beginning proficiency proposed by Moyers and colleagues (Moyers et al., Reference Moyers, Martin, Manuel, Miller and Ernst2010). Competence in MI was examined in one audio-recorded session with a participant per therapist. Sessions were coded by an independent rater demonstrating ‘excellent’ inter-rater reliability [intra-class coefficient (ICC) = 0.75–1.00] on five items, ‘good’ (ICC = 0.60–0.74) on four items, and ‘fair’ (ICC = 0.40–0.59) on three items compared with a ‘gold standard’ rater, according to a classification system proposed by Cicchetti (Reference Cicchetti1994).
The Credibility/Expectancy Questionnaire (CEQ; Devilly and Borkovec, Reference Devilly and Borkovec2000) was used to assess treatment credibility and expectancy for improvement. The CEQ consists of six items on two separate subscales and was administered following the third session, with higher scores indicating higher credibility (α = 0.86) or expectancy (α = 0.87). As responses are made on different scales (1–9 and 0–100%), a composite score is derived for each subscale by first standardising individual items and then summing those items for each subscale.
The Working Alliance Inventory – Short Revised (WAI-SR; Hatcher and Gillaspy, Reference Hatcher and Gillaspy2006) consists of 12 items and was used to assess participant-reported treatment alliance. The WAI-SR was administered following the sixth session, with higher scores indicating stronger working alliance (α = 0.95).
Treatment effects
Psychiatric disorder-specific symptoms
The Panic Disorder Severity Scale – Self-Rated (Houck et al., Reference Houck, Spiegel, Shear and Rucci2002) was used to assess panic symptoms, the Liebowitz Social Anxiety Scale, Self-Report (Fresco et al., Reference Fresco, Coles, Heimberg, Liebowitz, Hami, Stein and Goetz2001) for social anxiety symptoms, the Yale-Brown Obsessive Compulsive Scale Self-Report (Baer et al., Reference Baer, Brown-Beasley, Sorce and Henriques1993) for obsessive-compulsive symptoms, the Penn State Worry Questionnaire (PSWQ; Meyer et al., Reference Meyer, Miller, Metzger and Borkovec1990) for worry symptoms, and the Posttraumatic Diagnostic Scale (Foa et al., Reference Foa, Cashman, Jaycox and Perry1997) to assess post-traumatic stress symptoms. These measures were administered to participants depending on the principal diagnosis; for example, the PSWQ was administered to participants with GAD.
Unhealthy lifestyle behaviours
Unhealthy eating habits were measured using six items proposed by the National Food Agency (Sepp et al., Reference Sepp, Ekelund and Becker2004) to assess the frequency of consumption of certain unhealthy foods indicative of diet quality. The AUDIT consists of 10 items and was used to assess alcohol use. The International Physical Activity Questionnaire (IPAQ; Craig et al., Reference Craig, Marshall, Sjostrom, Bauman, Booth, Ainsworth and Oja2003) was used to assess physical activity. The IPAQ assesses physical activity in terms of metabolic equivalent of task (MET), a measure of energy expenditure. The IPAQ provides a measure in MET minutes of how much time per week is spent on three activity levels: moderate walks, moderately vigorous physical activity, and very vigorous physical activity. Higher scores indicate more physical activity. Tobacco use was assessed by items concerning number of cigarettes per day or boxes of snuff per week as proposed by the National Board of Health and Welfare (2011). These measures were administered to participants depending on which unhealthy lifestyle behaviours they showed; for example, the IPAQ was administered to participants with insufficient physical activity.
Other measures
The Generalized Anxiety Disorder Assessment 7 (GAD-7; Spitzer et al., Reference Spitzer, Kroenke, Williams and Lowe2006) consists of seven items and was used to assess general anxiety symptoms (α = 0.89) and the PHQ-9 (Kroenke et al., Reference Kroenke, Spitzer and Williams2001), which consists of nine items, was used to assess depressive symptoms (α = 0.78). The Sheehan Disability Scale (SDS; Sheehan, Reference Sheehan1983) consists of three items and was used to assesses functional impairment, with higher scores indicating more functional impairment (α = 0.64). The Quality of Life Inventory (QOLI; Frisch et al., Reference Frisch, Cornell, Villanueva and Retzlaff1992) consists of 32 items and was used to assess quality of life, with higher scores indicating higher quality (α = 0.79).
Several measures were used to assess potential mediators of effects to investigate in a future RCT. The Change Questionnaire (CQ; Miller and Johnson, Reference Miller and Johnson2008) consists of three items and was used to assess participant-reported motivation for behaviour change. Two versions of the CQ were developed: one for the psychiatric disorder (α = 0.33) and one for the lifestyle behaviour (α = 0.46). A self-efficacy (SE) measure was developed for use in the present study based on guidelines for SE scale construction (Bandura, Reference Bandura, Pajares and Urdan2006) and previous personal experience of SE scale development (e.g. Bohman, Rasmussen, & Ghaderi, Reference Bohman, Rasmussen and Ghaderi2016). Two versions were developed: one for the psychiatric disorder (six items; α = 0.77) and one for the lifestyle behaviour (five items; α = 0.72). Items concerned efficacy beliefs in performing activities or being in situations despite psychiatric symptoms or lifestyle behaviours and were rated between 0 and 10. To test multiple administration in preparation for a future RCT, the CQ and the SE measure were administered following the third and sixth session; the SE scale was also administered at pre-assessment. The Client Language Assessment in Motivational Interviewing (Miller et al., Reference Miller, Moyers, Manuel, Christopher and Amrhein2007) was used to measure observer-assessed participant motivation for behaviour change in terms of change talk; that is, utterances that are in favour of change, as opposed to sustain talk; utterances that are in favour of the status quo. Per cent change talk [change talk/(change talk + sustain talk)] was assessed based on three self-selected audio-recordings of the first or second session per therapist.
Data analysis
Data were analysed using the SPSS (version 26, SPSS Inc., Chicago, IL, USA) and an online effect size calculator (https://effect-size-calculator.herokuapp.com). Differences in the number of sessions between the CBT and MI-CBT conditions were examined using an independent samples t-test and in the proportion of drop-out between the conditions using relative risk with 95% confidence intervals (CI). Because participants had one of several psychiatric disorders as the principal diagnosis and there were few participants per diagnosis, a psychiatric symptoms index measure was created using the standardised scores of the symptoms measure of the principal diagnosis for each participant. The same procedure was used to create an unhealthy lifestyle behaviours index measure based on measures of unhealthy diet, alcohol use, physical activity (with scores reversed), and tobacco use. Within-condition effect sizes were calculated for feasibility measures and for treatment outcome measures from pre- to post-assessment and from pre- to 6-month follow-up assessment. Equations for within-condition Cohen’s d effect sizes suggested by Lakens (Reference Lakens2013) and employed in the online effect size calculator with Hedges’ correction g were used.
Results
Feasibility
Seventy-three patients were assessed for eligibility during an 8-month period; of these, 24 were excluded. Thus, 49 participants were randomly allocated to CBT alone (n = 21) or MI-CBT (n = 28). For participant flow through the study, including reasons for exclusion, see Fig. 1. In the CBT condition, 14 (66.7%) participants were females, mean age was 40.3 years (SD = 13.2), and 18 (85.7%) were born in Sweden. In the MI-CBT condition, 16 (57.1%) participants were females, mean age was 41.7 years (SD = 13.4), and 27 (96.4%) were born in Sweden. For principal psychiatric diagnosis and unhealthy lifestyle behaviours in participants, see Table 1.

Figure 1. Participant flow through the study. CBT, cognitive behavioural therapy; MI, motivational interviewing.
Table 1. Principal psychiatric diagnosis and unhealthy lifestyle behaviours

CBT, cognitive behavioural therapy; MI, motivational interviewing.
Mean number of treatment sessions was 8.2 sessions (SD = 5.2) in the CBT condition, and 10.7 sessions (SD = 7.7) in the MI-CBT condition, a difference that was not statistically significant, t 47 = –1.276, p = .208. Twenty-one (42.9%) participants dropped out of treatment, 11 (52.4%) in the CBT condition and 10 (35.7%) in the MI-CBT condition; the proportion of drop-out between conditions was not statistically different, relative risk = 1.44 [0.76, 2.75] (indicated by CI overlapping 1). Missing values across variables (i.e. feasibility and treatment outcome measures at different assessments) ranged from one to three missing values. In the MI-CBT condition, one therapist reached beginning proficiency in MI on four of the six MITI indicators of competence, and two therapists on two of the indicators. Means in participant perceptions of treatment credibility, expectancy for improvement, and working alliance were similar across the conditions; see Table 2. No adverse events were observed in the participants.
Table 2. Means in treatment credibility, expectancy for improvement, and working alliance

CBT, cognitive behavioural therapy; MI, motivational interviewing; CEQ credibility, Credibility/Expectancy Questionnaire, treatment credibility subscale (standardised); CEQ expectancy, CEQ, expectancy for improvement subscale (standardised); WAI-SR, Working Alliance Inventory – Short Revised.
Treatment effects
Means and within-condition Hedges’ g effect sizes in treatment outcome measures across assessments are presented in Table 3. Means changed in the expected direction across assessments for both the CBT and MI-CBT conditions, except for in the unhealthy lifestyle behaviours index for both conditions. Specifically, mean scores decreased in the psychiatric symptoms index, GAD-7, PHQ-9 and the SDS, and increased in the QOLI from pre- to post-assessment and from pre- to 6-month follow-up assessment. Within-condition effect sizes revealed that most of these improvements were large in magnitude in both conditions.
Table 3. Means and within-condition Hedges’ g effect sizes in treatment outcome measures
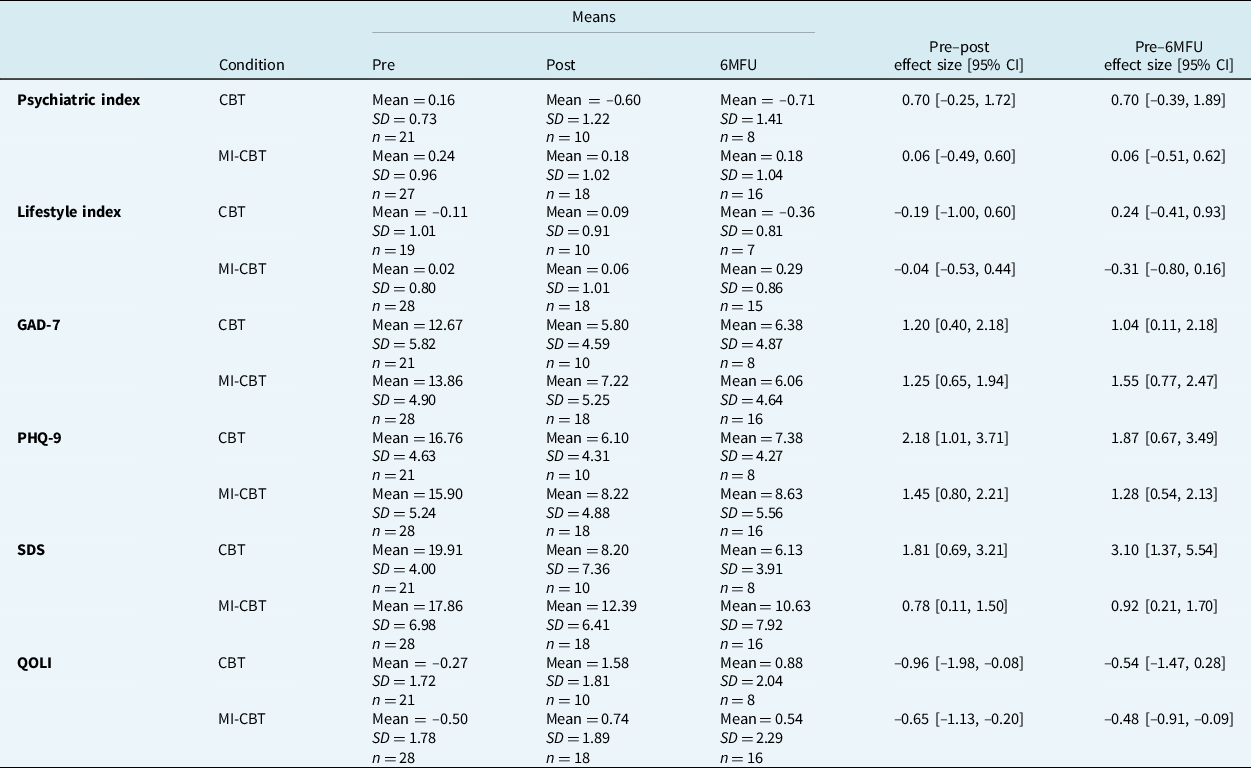
CI, confidence interval; 6MFU, 6-month follow-up; CBT, cognitive behavioural therapy; MI, motivational interviewing; Psychiatric index, psychiatric symptoms index (standardised); Lifestyle index, unhealthy lifestyle behaviors index (standardised); GAD-7, Generalized Anxiety Disorder Assessment-7; PHQ-9, Patient Health Questionnaire-9; SDS, Sheehan Disability Scale; QOLI, Quality of Life Inventory.
Additional results
Means in participant-reported motivation and SE were similar across assessments for the conditions; see Table 4. Furthermore, means changed in the expected direction across assessments, except for motivation to change unhealthy lifestyle behaviours in the MI-CBT condition. Within-condition effect sizes in SE for performing activities despite psychiatric symptoms were of moderate to large magnitude across assessments for both conditions. However, effect sizes in motivation to change psychiatric symptoms and unhealthy lifestyle behaviours were mostly small, and mostly non-existent in SE for performing activities despite unhealthy lifestyle behaviours (Table 4). Observer-assessed motivation in terms of change talk was 8.8 and 7.5% in the CBT and MI-CBT conditions, respectively.
Table 4. Means and within-condition Hedges’ g effect sizes for participant-reported motivation for behaviour change and self-efficacy

CI, confidence interval; CBT, cognitive behavioural therapy; MI, motivational interviewing; CQ psychiatric, Change Questionnaire: motivation to change psychiatric symptoms; CQ lifestyle, Change Questionnaire: motivation to change unhealthy lifestyle behaviors; SE psychiatric, self-efficacy for performing activities despite psychiatric symptoms; SE lifestyle, self-efficacy for performing activities despite unhealthy lifestyle behaviours.
Discussion
The primary aim of the present pilot trial was to investigate the feasibility of MI-CBT in preparation for a future RCT designed to assess the effectiveness of MI-CBT in routine psychiatric care. A secondary aim was to conduct separate preliminary evaluations exploring the effects of CBT alone for anxiety disorders and depression and of MI-CBT for anxiety disorders, depression, and unhealthy lifestyle behaviours. It was expected that MI-CBT would prove as feasible as CBT and that participants in both conditions would show clinically meaningful improvements.
The participants were recruited by the therapists, and the recruitment turned out to be rather slow. As suggested by anecdotal reports, this may have been due to therapist work stress, which may have led therapists to give less priority to recruitment. There was a high total drop-out rate of 42.9%, which was much higher than in the other two studies (16.7 and 16.5%, respectively) comparing CBT alone with MI-CBT in adult patients with anxiety disorders (Simpson et al., Reference Simpson, Zuckoff, Maher, Page, Franklin, Foa and Wang2010; Westra et al., Reference Westra, Constantino and Antony2016). In neither the present study nor in the Simpson or Westra studies was the proportion of drop-out between conditions statistically different. The drop-out rate of the present study is more similar to the findings of the meta-analysis of drop-out in CBT by Fernandez and colleagues (Fernandez et al., Reference Fernandez, Salem, Swift and Ramtahal2015). In any case, the drop-out rate is a concern in terms of feasibility. There are at least two possible explanations. The first pertains to characteristics of participants; in the present study participants were recruited in routine psychiatric care, whereas in the Simpson and Westra studies, participants were recruited at a research clinic and from the general population, respectively. In fact, the psychiatric clinic where participants were treated in the present study exclusively deliver treatment to patients with ‘complex’ disorders; that is, patients with high symptom severity or co-morbidity or with previous treatment failures. A second explanation pertains to heavy participant burden in terms of extensive assessment, which involved both psychiatric symptoms and unhealthy lifestyle behaviours measures, and potential mediators of change, assessed at several time points.
Ratings of treatment credibility, expectancy for improvement, and working alliance were similar across the conditions. Thus, it does not appear that the integration of MI and CBT or the dual treatment focus negatively influenced participant perceptions of treatment or the relationship to the therapist. This finding provides some preliminary support of the feasibility of MI-CBT.
In general, and consistent with expectations, the evaluation of treatment effects suggested that participants in both conditions experienced large and clinically meaningful reductions in anxiety and depressive symptoms and functional impairment, and moderate to large increases in quality of life from pre- to post-assessment and from pre- to 6-month follow-up assessment. These results provide additional preliminary support of the feasibility of MI-CBT and warrant further evaluations of this treatment. However, in the psychiatric symptoms and unhealthy lifestyle behaviours indices, effect sizes varied from non-existent to moderate across conditions and assessments. There were moderate to large improvements in SE for performing activities despite psychiatric symptoms across assessments for both conditions. However, effect sizes in motivation to change psychiatric symptoms and unhealthy lifestyle behaviours were mostly small, and largely non-existent in SE for performing activities despite unhealthy lifestyle behaviours, across assessments for both conditions.
There are at least two possible explanations of the lack of effects on unhealthy lifestyle behaviours and observer-assessed and participant-reported motivation. First, therapists may not have targeted lifestyle behaviours, despite an explicit focus to do so in the MI-CBT condition, which may be due to a perceived lack of ability. Therapists in routine psychiatric care do not typically target lifestyle behaviours. However, the extent to which therapists focused on lifestyle behaviours was not assessed. Second, MI-CBT may not have been delivered adequately as therapists, contrary to expectations, reached beginning proficiency in MI on only some indicators of competence. This result is similar to the study by Simpson and colleagues (Simpson et al., Reference Simpson, Zuckoff, Maher, Page, Franklin, Foa and Wang2010) in which therapists did not reach beginning proficiency on most indicators of competence in MI. In contrast, in the study by Westra and colleagues (Westra et al., Reference Westra, Constantino and Antony2016) only therapists demonstrating competence were allowed to enter the study and see participants. However, competence in the integration of MI and CBT was assessed neither in the present study nor the other studies, so it is not known to what extent therapists can actually provide skilful MI-CBT, rather than pure MI.
There are some limitations of the present study that should be taken into account when interpreting the results, and which may inform future studies. As already mentioned, therapists were not trained to competence in MI and CBT prior to entering the study; thus, treatment delivery may have been sub-optimal. Relatedly, fidelity was not assessed. Furthermore, the drop-out rate was high, indicating low feasibility in this respect. Finally, it cannot be ruled out that the differing assessment points after randomisation due to varying treatment length across participants to some extent could have influenced the results. Generalisability of the results may be limited to specialised psychiatric care settings.
Conclusions
In the present study, there were indications of feasibility of MI-CBT in some respects. However, because of insufficient participant recruitment and retention and therapist competence in MI, the study did not support the progression to an RCT designed to assess the effectiveness of MI-CBT in routine psychiatric care. Additional pilot studies are needed. Future pilot studies, and by extension RCTs, should ensure that these critical aspects are managed adequately, for example, by enabling an extended recruitment period and using procedures to ensure that therapists acquire competence.
The present pilot trial was only the second RCT to be conducted comparing CBT alone with MI-CBT in adult patients with anxiety disorders, and the first in a routine care setting using regular therapists. Moreover, it was the first trial to include participants with principal depression, a disorder that may be particularly apt for motivational work considering symptoms such as loss of interest and energy. In addition, it was one of few trials involving a dual treatment focus on both psychiatric disorders and unhealthy lifestyle behaviours. Given previous research of the benefits of combining MI and CBT, the paucity of studies integrating the treatments, and the potential benefit of simultaneous treatment of psychiatric disorders and unhealthy lifestyle behaviours, more research along these lines is warranted.
Acknowledgements
The authors would like to thank the participants and therapists at WeMind Psykiatri.
Financial support
This work was supported in part by the National Board of Health and Welfare (grant number 2.7-11638/2013).
Conflicts of interest
None.
Ethical statements
The authors have abided by the Ethical Principles of Psychologists and Code of Conduct as set out by the British Association for Behavioural and Cognitive Psychotherapies and the British Psychological Society. The study was approved by the Ethical Review Board in Stockholm, Sweden (2013/1566-31/3). Participants provided written informed consent.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Author contributions
AG and BB designed the study and wrote the initial draft. All authors conducted the statistical analyses, interpreted the results, and critically revised the manuscript. All authors read and approved the final manuscript.








Comments
No Comments have been published for this article.