A previous study reported that 28.3% of UK adults were not sure or strongly hesitant to be vaccinated against the COVID-19, and the vaccine hesitancy varies greatly by socio-demographic and clinical background (Freeman et al., Reference Freeman, Loe, Chadwick, Vaccari, Waite, Rosebrock and Lambe2020). Patients with severe mental illness are more likely to suffer from severe clinical outcomes of COVID-19 (Wang, Xu, & Volkow, Reference Wang, Xu and Volkow2021), thus it has been advocated that they should be prioritized for vaccination (De Hert, Mazereel, Detraux, & Van Assche, Reference De Hert, Mazereel, Detraux and Van Assche2021). However, vaccine hesitancy in this subpopulation is a major obstacle in the global efforts to control the COVID-19 pandemic. There is little research on this problem apart from two preliminary, single-center surveys conducted in Western countries. A study (Mazereel, Vanbrabant, Desplenter, & De Hert, Reference Mazereel, Vanbrabant, Desplenter and De Hert2021) in a Belgium psychiatric hospital (N = 1151) found that 93% of hospitalized patients with various psychiatric disorders accepted and received COVID-19 vaccines. Another study (Danenberg et al., Reference Danenberg, Shemesh, Tzur Bitan, Maoz, Saker, Dror and Bloch2021) in an Israeli public psychiatric hospital (N = 51) found that 23.5% of hospitalized patients with severe mental illness had no intention to get vaccinated. To date, there are no data on vaccine hesitancy in non-Western settings or in community-dwelling patients with psychiatric disorders or across various diagnostic groups. Therefore, we examined the prevalence of vaccine hesitancy and its associated factors among community-dwelling and hospitalized patients with major depressive disorder (MDD), bipolar disorder (BD), and schizophrenia (SCZ) in China, the largest developing country.
This study was conducted in both outpatient clinics for community-dwelling patients and inpatient departments attached to six major psychiatric hospitals in China between September 21, 2020 and October 8, 2021. Community-dwelling and hospitalized participants who were diagnosed as MDD, BD, or SCZ according to the International Classification of Diseases, Tenth Revision (ICD-10) and older than 18 years were consecutively invited to participate in this survey. Global quality of life was measured with the first two items of the World Health Organization Quality of Life Scale Brief version (WHOQOL-BREF), while severity of perceived fatigue and physical pain were assessed by a fatigue numeric rating scale and Visual Analog Scale for Pain (VAS), respectively. Depressive symptoms were measured by the Patient Health Questionnaire-2 (PHQ-2), and perceived stigma was assessed by the Social Impact Scale (SIS). A standardized question was used to measure COVID-19 vaccination hesitancy: ‘Do you intend to be vaccinated against COVID-19 in the future?’ (No/Not having vaccination temporarily/Yes). The first two options were categorized as ‘COVID-19 vaccination hesitancy’ according to the WHO recommendation. All participants signed electronic written informed consent and the study protocol was approved by the ethics committees of the participating hospitals.
The χ2 tests, independent samples t tests, and Mann–Whitney U tests were performed to compare sociodemographic and disorder-related variables between individuals with COVID-19 vaccination hesitancy and those without, as appropriate. Binary logistic analyses were performed to examine independent correlates of COVID-19 vaccination hesitancy, with variables that significantly differed in univariate analyses and primary psychiatric disorders as independent variables. Significantly statistical difference was set at p < 0.05 (two-tailed).
Altogether, 1853 participants were included in this study. The proportion of COVID-19 vaccination hesitancy was 45.3% (95% CI: 43.1–47.5%), with 45.3% (95% CI: 42.6–48.1%) in MDD, 43.6% (95% CI: 38.6–48.7%) in BD, and 47.4% (95% CI: 41.6–53.3%) in SCZ subgroups. The proportion of COVID-19 vaccination hesitancy was 49.2% (95% CI: 46.7–51.8%) in community-dwelling patients, and 31.3% (95% CI: 26.9–35.8%) in hospitalized patients. Binary logistical regression analysis revealed that unemployed patients (OR 1.257, 95% CI: 1.038–1.522, p = 0.019), community-dwelling patients (OR 2.206, 95% CI: 1.737–2.801, p < 0.001), and those with a higher level of perceived stigma (OR 1.011, 95% CI: 1.002–1.019, p = 0.011) were more likely to have vaccine hesitancy (Table 1). No significant difference in vaccine hesitancy was found across the three major psychiatric disorders.
Table 1. Characteristics and analyses of participants with and without COVID-19 vaccination hesitancy
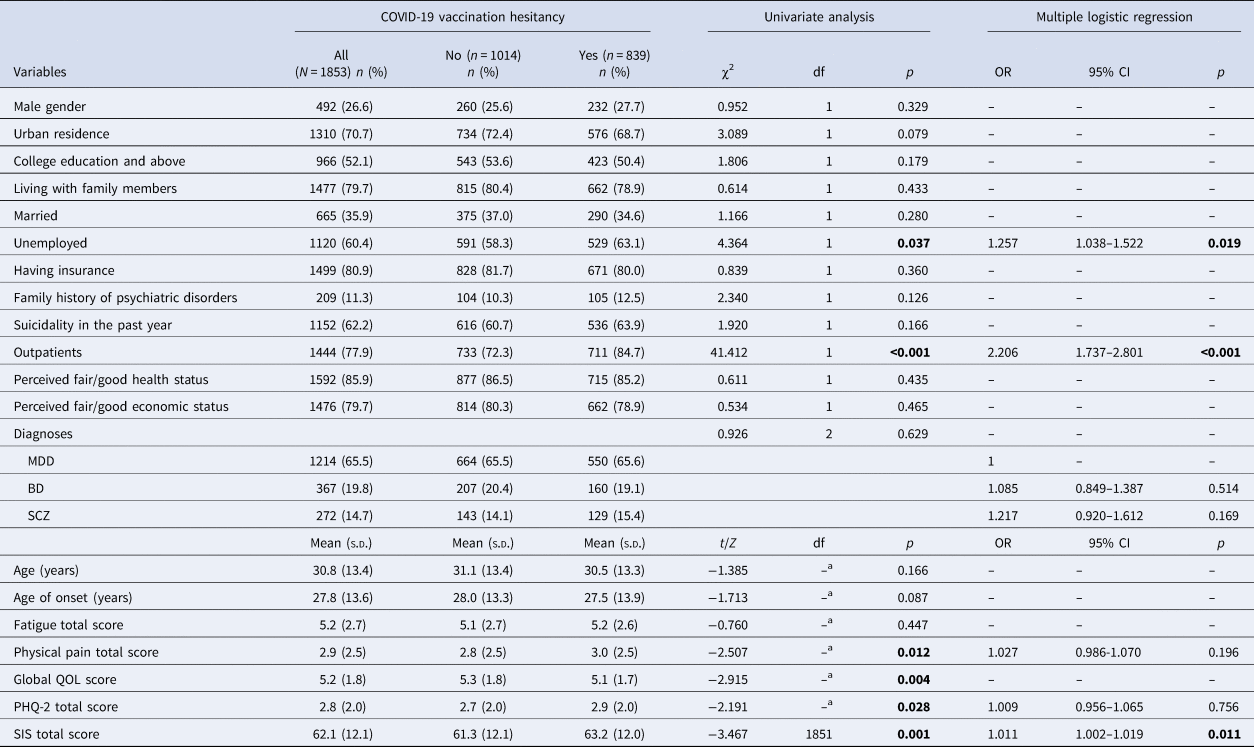
OR: odds ratio; CI: confidence interval; S.D., standard deviation; COVID-19, Corona Virus Disease 2019; PHQ-2, 2-item Patient Health Questionnaire; SIS, Social Impact Scale; QOL, Quality of Life; MDD, major depressive disorder; BD, bipolar disorder; SCZ, schizophrenia.
a Mann–Whitney U test; bolded values: <0.05.
We found that the vaccine hesitancy rate was high in patients with severe mental illness, particularly in community-dwelling patients, which is considerably higher than the finding in Israel (Danenberg et al., Reference Danenberg, Shemesh, Tzur Bitan, Maoz, Saker, Dror and Bloch2021). Consistent with the result in a general population in the USA (Malik, McFadden, Elharake, & Omer, Reference Malik, McFadden, Elharake and Omer2020), there is a higher rate of vaccine hesitancy in those unemployed compared to those employed, which could partly be due to the strong encouragement from all employers in China for vaccination in their employees in response to the pandemic.
Community-dwelling patients with severe mental illness had a higher rate of vaccine hesitancy than hospitalized patients, probably because they received less public education on the importance and safety of the vaccines compared to hospitalized patients. Additionally, hospitalized patients are more likely to experience crowded living conditions compared to their community-dwelling counterparts (e.g. shared common dining and bathroom spaces, and group activities that increase close contacts) (Brody et al., Reference Brody, Shi, Shaffer, Eden, Wyka, Alexopoulos and Kanellopoulos2021), which may lead to greater awareness of the need to protect themselves. We also found that patients with a higher level of perceived stigma were more likely to have vaccine hesitancy. Psychiatric patients with a higher level of stigma usually have more limited medical knowledge (Thornicroft et al., Reference Thornicroft, Mehta, Clement, Evans-Lacko, Doherty, Rose and Henderson2016), and a lack of awareness about the efficacy and safety of COVID-19 vaccination.
In conclusion, this was the first multicenter study on COVID-19 vaccine hesitancy involving both community-dwelling and hospitalized patients with severe mental illness. Due to the high rate of vaccine hesitancy, vaccination promotion strategy should focus on patients with severe mental illness, particularly those who are unemployed and community-dwelling, or have a high level of perceived stigma.
Acknowledgements
The authors thank all clinicians and patients involved in this study.
Conflict of interest
None.






