INTRODUCTION
Trauma is the principal cause of morbidity and mortality among individuals under 44 years old in North America. Moreover, unintentional injury is the fifth leading cause of death in all age groups worldwide. 1 , 2 The importance of rapid extrication and delivery of trauma patients to centres of definitive care was recognized as early as the Napoleonic wars, with purpose-built battlefield horse-drawn carriages; however, the modern era of trauma transport commenced with the use of rotor-wing aircraft during the Vietnam war.Reference Tobin, Via and Carter 3 Over the intervening five decades, helicopter transport has emerged as an integral component of emergency medical services and trauma networks. In concert with this, improved trauma outcomes have been noted over this same time period. While consensus exists regarding the primary use of helicopter transport in some instances (e.g., rural settings, delayed ground transport), it is not possible for helicopter transport to improve outcomes in all circumstances; from a practical perspective, few evidence-based guidelines exist to aid in the decision to assign trauma patients to one form of transport over another.
The purpose of this study was to investigate the relationship between trauma patient outcomes and mode of transport at a single Ontario Level I Trauma Centre, and specifically to investigate if the mode of transport confers a mortality benefit.
METHODS
Hamilton General Hospital (HGH) is one of 11 adult provincial Lead Trauma Hospitals (LTHs) in Ontario, Canada. HGH serves a population of 1.5 million residents in both urban and rural environments, and has approximately 800 trauma activations per year, with approximately one in seven patients arriving by rotor-wing transport. Trauma team activation occurs with patients meeting pre-defined mechanism, anatomical, or physiological criteria that are standard across the province, and consistent with broader patterns of practice. At minimum, the trauma team consists of a dedicated trauma team leader as well as physicians from anesthesia, general surgery, and orthopedics services. There are no tiered trauma team activations. Ground transportation is provided by a number of regional EMS services, most under the oversight of a single, centralized medical director. Most crews consist of two primary care paramedics (PCPs); less commonly crews also include advanced care paramedics (ACPs). Regional rotor-wing transport is provided by a provincially-funded not-for-profit organization independent of any single hospital; two critical care paramedics (CCPs) constitute the crew. Paramedical scope of practice is provincially regulated in Ontario, with specific off-line directives at the discretion of the local medical director. Dispatch of rotor-wing transport direct to scene involves the communication of local ground ambulance dispatch directly with the regional rotor-wing ambulance dispatch. Transport time greater than 30 minutes, prolonged extrication, or a perceived need for an expanded scope of prehospital practice typically prompt this interaction. Subsequently, rotor-wing dispatch then includes consideration of operational variables such as weather, crew status, and total distance of transport in the final decision about whether to deliver a request for service.
An historical, observational cohort study with data drawn from the chart-abstracted HGH Trauma Registry from the years 1995–2013 was undertaken. The HGH registry comprises the comprehensive data set contributed to the Canadian Institute for Health Information–administered Ontario Trauma Registry. The goals of this database include contribution to the reduction of injuries and related deaths in Canada, facilitating national and international comparisons of injuries, increasing awareness of injury as a public health challenge in Canada, and support for injury-related research. The database is populated and managed by full-time dedicated employees. Locally, inter-rater reliability is calculated quarterly and overall agreement is consistently ≥95%. The HGH Trauma Registry was electronically searched by one of the authors (AC), to capture all patients in the specified time frame meeting the defined inclusion criteria. Subsequently, the data were manually reviewed for exclusion criteria by a different author (IB) before being exported for statistical analysis.
Inclusion criteria were: age ≥18 years and trauma team activation. Exclusion criteria were: death prior to transport, Injury Severity Score (ISS)<12, chemical paralysis, >30% missing data for descriptive statistics, any missing data for TRISS-L calculation, any mixed modes of transport, and transport not direct from scene to LTH. The data abstracted included demographic, outcome, mechanism, and temporal variables.
Continuous variables were tested for normality by the D’Agostino and Pearson method, and measures of central tendency are reported as medians with interquartile ranges due to non-parametric distributions. Binary variables are reported as proportions with 95% confidence intervals. Significance was evaluated at p<0.05 with Mann-Whitney, chi-square test with Young’s correction, and Fisher exact tests as appropriate. TRISS-L analysis was applied to investigate mortality by transport method.Reference Offner, Jurkovich and Gurney 4 Data were collected and analyzed in Microsoft Excel (Microsoft Corp., Redmond, WA), and Prism 6 (GraphPad Software Inc., La Jolla, CA).
TRISS-L analysis calculates a predicted survival using a derived logistic regression function, with input variables comprised of the motor component of the Glasgow Coma Scale (GCS), systolic blood pressure (SBP), ISS score, and age. TRISS-L was developed to offset the analytic bias inherent in the original TRISS method,Reference Baxt and Moody 5 , Reference Boyd, Tolson and Copes 6 thus allowing for the inclusion of patients intubated in the prehospital environment. Furthermore, updated regression coefficients specific to the population studied were utilized.Reference Lane, Doig and Stewart 7 Predicted survival is compared with actual survival individually for each cohort. Implied survival benefit is calculated with Z- and W-statistics. Z is a quantitation of the difference between predicted and actual survival in the sample population. It is expressed as a standardized score in units of standard deviation.Reference Flora 8 Absolute values of Z >1.96 are statistically significant at p<0.05; positive numbers imply that predicted deaths exceed actual deaths, and the converse is implied for negative numbers. W reports increase or decrease in deaths from the expected per 100 patients treated with a given intervention (e.g., mode of transport). It was not possible to calculate M-statistics (measuring goodness-of-fit to the coefficient derivation cohort), as the derivation data of fractions stratified by survival were not available in the published manuscript, or through communication with the corresponding author.Reference Boyd, Tolson and Copes 6 , Reference Lane, Doig and Stewart 7
The HGH Trauma Registry is administered by the MacTrauma Research Committee, and approval was obtained from the joint Hamilton Health Sciences/McMaster Health Sciences Research Ethics Board.
RESULTS
9,619 records from January, 1995 to March, 2013 were abstracted. Figure 1 provides a graphic illustration of the study population, and reasons for the 6,473 cases that were excluded, resulting in 3,146 records in our study cohort. Overall, patients excluded for missing data represented approximately 10% of all records.

Figure 1 Study flow diagram detailing selection of included patients. Inclusion and exclusion criteria applied to abstracted records, resulting in the final study population examined.
2,759 (87.7%) patients were transported from scene by ground transportation and 387 (12.3%) by rotor-wing aircraft. Table 1 provides characteristics of the study population, categorized by mode of transport. Patients transported by rotor-wing were younger (median age, 39 years versus 47 years; p<0.001), and unadjusted mortality was lower for rotor-wing patients than ground patients (8.8% vs. 16.1%; p<0.001). Distribution of categorized ISS scores for rotor-wing patients suggested more severe injury in this group. More rotor-wing transported patients required extrication (56.3% vs. 17.3%; p<0.0001), a difference not explained by varying proportions of mechanism of injury alone. Median extrication time was also longer for rotor-wing transported patients (40 minutes vs. 20 minutes; p<0.0001). Mechanisms of injury were similarly distributed between the transport groups. In both ground and rotor-wing transported patients, motor vehicle collisions and falls represented the most common mechanisms of injury; however, motor vehicle collisions for rotor-wing transported patients represented the dominant majority of patients transported (72.9% vs. 33.2%; p<0.0001). Falls represented a much smaller proportion of rotor-wing transported patients when compared with the ground transported cohort (9.8% vs. 33.1%; p<0.0001). The median total prehospital time was longer for rotor-wing patients compared to patients transported via ground (73 minutes vs. 45 minutes; p<0.0001) (Figure 2). Over the study period, two clear temporal trends emerged. Rotor-wing transport was used more frequently in recent years (16.5% vs. 6.3% of total transports in the second vs. first half of the dataset, p<0.0001). Also, seasonal variations in rotor-wing transport volume not explained by overall volume trends were present when compared with ground transported patients (66.7% vs. 53.2% of total transports occurring between April and September; p<0.0001).

Figure 2 Prehospital time by mode of transport. Time, in minutes, from call received to arrival at hospital by component parts. (“call”=call received; “dispatch”=ambulance dispatched; “scene”=arrival at scene; “depart”=departure from scene; “LTH”=arrival at Lead Trauma Hospital).
Table 1 Characteristics of study population.

TRISS-L analysis revealed that ground transported patients under-performed their predicted mortality, with 1.4 more deaths per 100 transports, whereas rotor-wing patients outperformed predictions, with 5.2 fewer deaths per 100 transports (see Figures 3 and 4).

Figure 3 Actual and TRISS-L predicted mortality by mode of transport. Predicted mortality as calculated by TRISS-L analysis compared with actual mortality derived from the database. The calculated difference on a per cent basis representing the W-statistic.
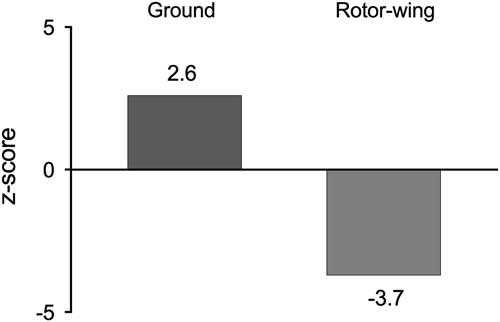
Figure 4 TRISS-L effect size by mode of transport. Standardized Z-scores representing the direction and size of effect suggested by TRISS-L analysis. Positive scores indicate actual mortality is higher than predicted; negative scores indicate the converse. Magnitude suggests effect size, and statistical significance (p<0.05) is achieved at an absolute value of 1.96.
DISCUSSION
For the past five decades, the establishment of evidence-based guidelines for the transport of trauma patients has been a long-sought, yet difficult to achieve objective. Numerous studies utilizing a range of local as well as national trauma registries have attempted to clarify the optimal mode of transport for trauma patients.Reference Baxt and Moody 5 , Reference Boyd, Corse and Campbell 9 - Reference Younge, Coats and Gurney 22 Sample sizes have ranged from the hundreds to thousands for single-centre studies, to hundreds of thousands for multi-centre studies. Common limitations in all these investigations have included a lack of generalizability, missing data, and difficulty controlling for differences between ground and air transported groups. Recent reviews and systematic reviews provided mixed messages with respect to overall outcomes, citing evidence of both clear benefit and alternatively lack thereof with helicopter transport. The heterogeneous nature of the involved study populations and designs have likely contributed to this lack of clarity.Reference Moga and Harstall 23 - Reference Thomas, Cheema and Wedel 25 Specific to the Canadian context, only three previous studies exist comparing the outcomes of ground versus helicopter transported patients, two of which directly assessed mortality.Reference Cummings and O’Keefe 26 - Reference McVey, Petrie and Tallon 28
Our study represents some of the most robust Canadian data to date regarding mortality in trauma patients transported directly from scene to a trauma centre, stratified by mode of transport. The geographic milieu for our study was that of a mixed rural/urban catchment area, containing 13% and 5% of the provincial and national populations, respectively. Our study represents a large and likely generalizable dataset, specific to the Canadian trauma transport context. Confounding was limited with the inclusion of solely scene-transported patients. Furthermore, the use of TRISS-L analysis allowed the inclusion of patients ill enough to require intubation in the prehospital environment.
Our results suggest that trauma patients transported from scene by rotor-wing aircraft have more significant mechanism and injuries than those transported by ground ambulance. Our results also suggest that mode of transport carries a mortality benefit, with air transported patients outperforming their predicted outcome as well as outperforming the ground transported comparison group. This improved survival was found to exist even in the face of significantly longer prehospital times. Both triage guidelines as well as experience suggest that, when faced with a patient that is perceived to be more significantly injured, the reaction to call for air transport is a common one. Given that the majority of our study population, as well as approximately half our study catchment area, can be reached within thirty minutes’ driving, it is also not surprising that prehospital times were longer for rotor-wing transported patients, given the complexity of mobilizing this remote and sophisticated resource. Despite this extended prehospital time, it may be that the expanded scope of practice delivered by the CCPs that staff Ontario’s provincial air ambulance service may provide the most rapid access to life-prolonging and stabilizing therapies that would not be available if attended by a basic or advanced care paramedic staffing a ground ambulance. Our data suggest that the projected time-to-hospital must be considered in the context of this and other potential variables when making decisions regarding dispatch of first responders.
For three decades, TRISS-based analysis has been a commonly utilized tool for evaluating outcomes in trauma patients. Although ubiquitous, a number of limitations have been identified with TRISS.Reference Schluter, Nathens and Neal 17 , Reference Gabbe, Cameron and Wolfe 29 - Reference Schluter 31 First, the use of variables recorded on admission to hospital as opposed to field values may misrepresent illness severity in patients who receive prehospital resuscitation. In our study, a subset of patients with recorded prehospital TRISS-L variables were compared with first recorded LTH values and no significant differences were noted. Second, given the reliance on population-specific coefficients in the model, changes in case mix or advances in trauma care can lead to inaccuracy of predicted survival. In our study, although we were unable to calculate an M-statistic, our use of updated coefficients derived from a population that included our own (but preceding the study period) should have minimized the risk of confounding for this reason. Third, specific to TRISS-L methodology, chemical paralysis is a necessary exclusion criteria. The original TRISS methodology excluded all intubated patients, as the Revised Trauma Score, of which total GCS and respiratory rate are components, was required for the model. One of the main criticisms of the original TRISS methodology was this systematic exclusion of these patients who were also more likely to be critically injured. As a result, TRISS-L analysis was developed in an attempt to negate this bias by including only the GCS motor score in its model, based on the knowledge that it is the component of the GCS most predictive of survival.Reference Offner, Jurkovich and Gurney 4 In spite of being less broadly used, we chose to employ TRISS-L analysis for this reason. Intubated patients were not excluded; however, those chemically paralyzed were excluded, as the GCS motor score becomes impossible or unreliable to measure thereafter. Specific to our study population, 3.5% of the total study population (323 patients) were excluded for chemical paralysis. Furthermore, 316 of these also belonged in the group excluded for “transport not direct from scene” (i.e., interfacility transports). This left only seven patients in the “direct from scene” group excluded for chemical paralysis: five patients in the rotor-wing group, and two patients in the ground group. We feel that this number of excluded patients was unlikely to significantly bias our results. Finally, it has been proposed that the derivation of the original TRISS model was performed with statistical methods that are now outdated, and that there is imperfect generalizability to all mechanisms of injury. Attempts have been made to improve the model performance using updated statistical methods and some have advocated for the use of alternative models altogether.Reference Galvagno, Thomas and Stephens 32 Regardless, and while recognizing its shortcomings, we purposefully chose a TRISS-based method, as it remains a standard in the field for comparison with previously published works. Moreover, its ease of use allows for local implementation with smaller datasets and without the need for complex statistical support. This local application allow for the identification of context-specific trends on a regional basis to guide allocation of trauma transport resources.
Our study has a number of additional specific limitations that merit consideration. First, similar to many health services research studies, our use of retrospective database-extracted cohorts introduced the risk of missing or incorrect data confounding outcomes. That said, our missing data proportion of approximately 10% is certainly comparable to or better than other similar database-driven trauma transport studies.Reference Rogers, Osler and Krasne 30 Data entry was performed by full time, skilled technologists with many years of experience, further limiting the likelihood of error. Second, a minimal amount of penetrating trauma is present in this dataset, so our results may be poorly generalizable to this group. Third, the final TRISS-L analysis was underpowered. Previous literature suggests that adequately powered studies using logistic regression models are achieved with 12–15 outcomes of interest (in our case, deaths) per variable.Reference Babyak 33 , Reference Peduzzi, Concato and Kemper 34 TRISS-L analysis employs four variables (GCS motor score, SBP, ISS, age), and as such 48–60 deaths among air transported patients would be sufficient. In our case, 34 deaths were noted in the rotor-wing transported cohort. Regardless, in this group an absolute Z-score of >1.96 was noted, as the effect size observed was large enough to offset any potential deficiency in power. Finally, data that would have been particularly helpful in extending the scope and conclusions of this work (e.g., transport distance, procedures performed in transport) were not captured in a consistent or easily extractable manner. This limitation is significant in that it did not allow for the examination of factors that are unique to each transport modality (i.e., the expanded scope of CCPs, improved access to remote locations) as they relate to patient outcomes. While the TRISS-L analysis highlighted a wide difference between the groups examined, it is thus impossible for us to differentiate with any certainty what contributed to this difference. While it is conceivable that the advanced training of CCPs contributed to the outcomes within the rotor-wing transported group, it is unclear what exactly about the care delivered would have led to this difference, and other possible explanations for our findings also exist. Overall, our results provide an essential hypothesis, generating consideration for future research on this topic, and should serve to inform prospective study design as well as the data captured in trauma registries.
CONCLUSIONS
Rotor-wing and ground transported trauma patients represent heterogeneous populations with respect to age, location/mechanism of injury, and injury severity. Accounting for these differences, in the mixed rural/urban Canadian population studied, rotor-wing patients were found to outperform their predicted mortality, whereas ground patients underperformed predictions. Further research examining details of transport is necessary to draw any further conclusion about causality, and to establish best practice for triage of trauma patients to any given mode of transport.
Competing Interests: Dr. Buchanan reports grants from Regional Medical Associates in support of this study.









