There has been a move to community-based mental healthcare for the past half-century: Reference Sjølie, Karlsson and Kim1 the number of in-patient psychiatric beds in the UK fell from 152 000 in 1954 to 29 802 in 2005. Reference Crompton and Daniel2 Crisis resolution and home treatment teams (known variously as CRHTTs, CRTs and HTTs; CRT will be used throughout this article) were established in the 1980s, but the first policy, mandated in The NHS Plan, did not come about until 2000. 3 By 2006, 343 teams had been introduced. Reference Crompton and Daniel2 They were designed as ward ‘gatekeepers’, providing intensive short-term care to vulnerable patients considered for admission or discharge. 4 Teams of approximately 14 multidisciplinary staff, predominantly nursing, were anticipated to have case-loads of 20-30 and to be available 24 hours a day, 7 days a week, to a wide variety of patients. Potential interventions would include assessment and engagement of patients in crisis, psychological support and education, medication review and administration, and social support and advocacy.
Despite these laudable aims, it has been argued that policy was implemented without sufficient evidence. Reference Pelosi and Jackson5,Reference Smyth and Hoult6 To date there has been little direct advice or guidance specifically to CRTs on markers of good care or outcomes. The Royal College of Psychiatrists is attempting to redress this with the recent piloting of the Home Treatment Accreditation Scheme (HTAS) that will, following refinement of goals through analysis of data obtained in this pilot, establish national standards for accredited teams. In this context of a questionable research base and the setting up of a national accreditation scheme, and under the spectre of future primary care (de)commissioning of services, we have set out to systematically review the existing evidence for CRTs and to provide a commentary on this. In particular, this review aims to establish: (a) whether CRTs have affected voluntary and/or compulsory admissions; (b) the clinical profiles of patients admitted despite CRTs; (c) whether CRTs are cost-effective; and (d) whether patients are satisfied with the care received.
Method
Search strategy
A systematic literature review was conducted and reviewed by R.A.C. and D.K.T. References were retrieved via PubMed and PsycINFO (1998-present) as well as through searches of studies in recent reviews Reference Sjølie, Karlsson and Kim1,Reference Hubbeling and Bertram7,Reference Winness, Borg and Kim8 and scanning reference lists of articles found: the keywords used were ‘psychiatr*’ or ‘mental’, and ‘crisis resolution’ or ‘crisis assessment’ or ‘crisis intervention’ or ‘intensive home treatment’ or ‘home treatment’. The last search was run on 29 March 2012.
Eligibility criteria
The following exclusion criteria were established in advance of the literature search.
-
• Participants: studies that looked specifically at children and adolescents, older adults or only staff were excluded, thus focusing only on working-age adults, for whom CRTs were intended. 3
-
• Interventions: only studies that described a CRT as defined in The NHS Plan, 3 and therefore only those published after 2000.
-
• Comparators: no comparators were required for inclusion in this systematic review.
-
• Outcomes: studies that addressed one or more of the research questions, that is: (a) voluntary and/or compulsory admission rates and duration of admission either between an area with a CRT compared with an area without, or pre- and post-CRT introduction in a certain catchment area; (2) the characteristics of patients admitted to hospital since CRT introduction; (c) the cost-effectiveness of CRTs; and (d) quantitative and qualitative measures of patient satisfaction with CRT care.
-
• Study design: both randomised controlled trials (RCTs) and non-RCTs were reviewed.
Studies that were not published in English were excluded.
Study selection
The initial search of electronic databases produced 2169 abstracts. First, these were sequentially screened on the basis of title and abstract and 1983 articles that clearly did not refer to a CRT were excluded. Second, 93 duplicates were removed by importing all remaining articles into an Excel file and matching titles, authors’ names and sources. At this stage, there were 79 articles that were read in full and those that did not meet the eligibility criteria were excluded. The reference lists of all articles that were reviews or meta-analyses were examined and this revealed 4 articles that had not been found in the initial literature search, such that 83 articles were read in full. Of these 83, 10 studies were excluded because they did not meet the participants’ eligibility criteria, 16 because they did not meet the intervention’s eligibility criteria, 18 because they did not meet the outcome’s eligibility criteria, and 2 studies were excluded because of duplicate publication (same content but different title and journal). Ultimately, 37 articles were reviewed. A flow diagram summarising the study selection process is shown in Fig. 1.
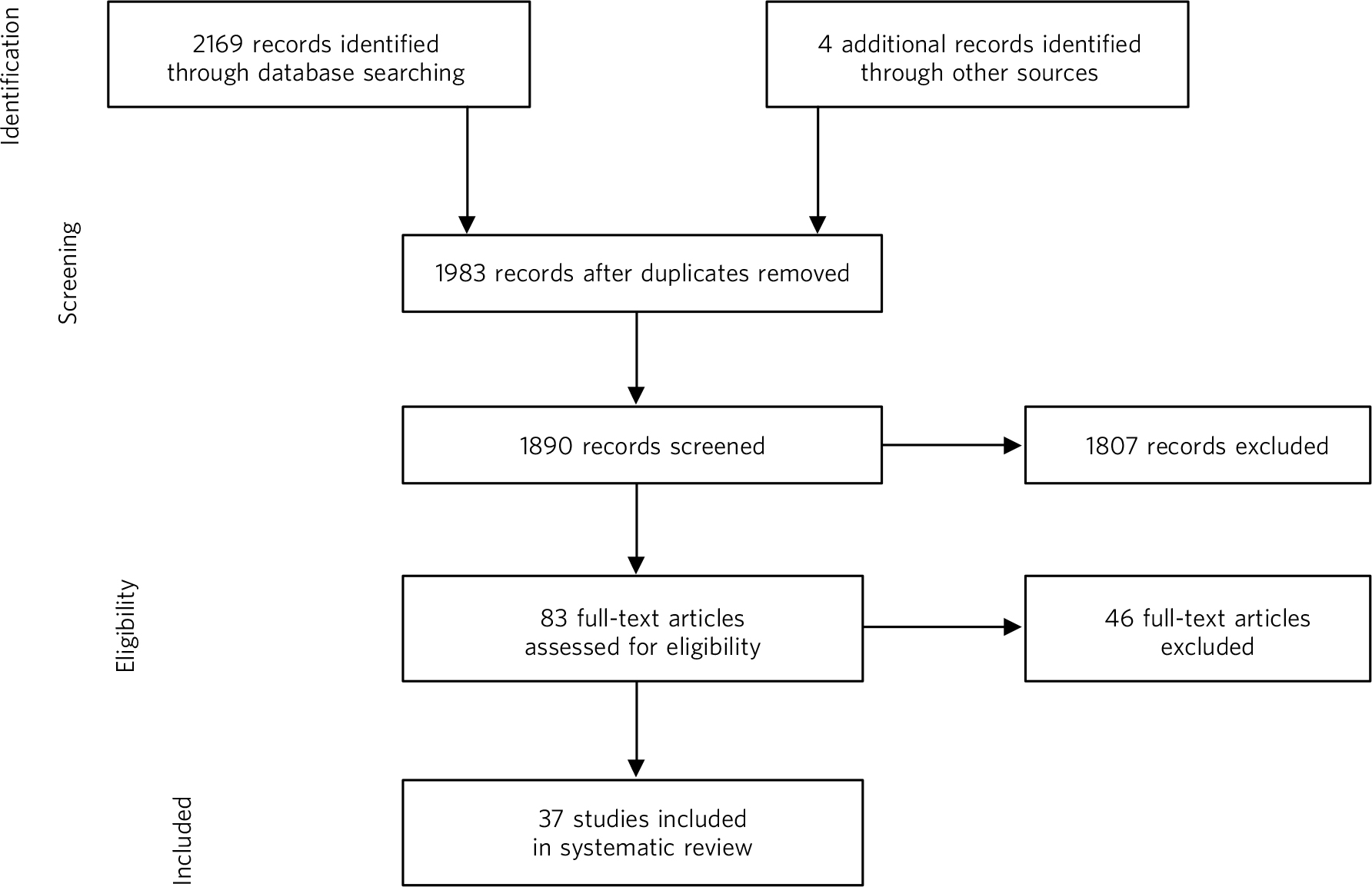
Fig 1 Flow diagram of study selection process.
Data extraction
We extracted the data to collate all the relevant information from each article: year and location of publication, study type, number and characteristics of participants, primary and secondary outcome measures, primary and secondary results and limitations of study.
Data analysis
For each of the four review aims, a table is presented with characteristics of included studies, primary outcome and risk of bias within the studies. Meta-analyses generally present an elegant means of summarising the existing literature. However, the means in which previously published findings are reported prevented meta-analysis from being usefully conducted for the purposes of this work. For both cost-effectiveness and patient satisfaction only one study in each provided sufficient detail for inclusion into a meta-analysis, and thence this was not carried out.
Results
Have CRTs affected voluntary and compulsory in-patient admissions?
Voluntary admission rates and duration
The NHS Plan 3 stated that CRTs should produce a 30% reduction of both rate and length of admission. Twenty studies, of varying quality, addressed this question (see online Table DS1 for characteristics of included studies and risk of bias within studies), but, perhaps due to the inherent ethical and clinical problems of randomisation in such a vulnerable population, only one was an RCT. Reference Johnson, Nolan, Pilling, Sandor, Hoult and McKenzie9 This RCT compared a CRT in inner London with standard care, consisting of in-patient services, local community mental health teams and two crisis houses. Patients receiving care from a CRT were less likely than controls to be admitted at the 8-week and 6-month study points, but compulsory admissions were not significantly reduced. By 6 months, the number of days spent in hospital was also statistically less in the CRT group, but the severity of clinical and social outcomes was similar between groups. The study was limited in that 104 admitted patients were excluded from the analysis for several different reasons, including patients not following study procedures (n = 25) and incapacitous or non-consenting patients (n = 46): inevitably, such patients were likely to be more disturbed than average but represent part of a typical CRT case-load.
Twelve ‘pre- and post-CRT comparison’ studies compared outcomes before and after the introduction of a CRT, with eight studies showing reduced admission rates post-introduction and four reporting no difference. One study found statistically significant reductions in admission rates (71% v. 49%) and mean number of bed days (19.1 v. 12.9) in the 6 weeks following a crisis. Reference Johnson, Nolan, Hoult, White, Bebbington and Sandor10 Likewise, another study Reference Barker, Taylor, Kader, Stewart and Le Fevre11 showed a 24% decrease in acute psychiatric admissions, a 22% decrease in mean duration of in-patient stay, a 17% reduction in Mental Health Act admissions, and a 4% decrease in readmissions. Keown and colleagues Reference Keown, Tacchi, Niemiec and Hughes12 found admission rates decreased by 45% after CRT implementation, and more so for females and younger adults: they postulated this was because younger women may have more support in the community or stay out of hospital for childcare. This research also found that the length of stay increased from 15.5 to 25 days after CRT implementation.
Conversely, two studies, one in Australia Reference Adesanya13 and one in Scotland, Reference Forbes, Cash and Lawrie14 found no statistically significant differences in admission rates, although both CRTs studied experienced staff shortages. A study of a CRT in Wales Reference Tyrer, Gordon, Nourmand, Lawrence, Curran and Southgate15 found overall bed usage unchanged, attributed to a reduction in informal admissions coinciding with compulsory admissions increasing. Similarly, another study, in England, found no differences, although it lacked statistical power. Reference Jacobs and Barrenho16
Interpreting admission rate and duration data These ‘pre- and post-CRT’ studies aid discussion but face the inherent confounders of temporally distinct assessments and the fact that CRT introduction often coincides with bed reductions. Reference Tyrer, Gordon, Nourmand, Lawrence, Curran and Southgate15 In an examination of admission rates in 229 primary care trusts in England, of which 34 had CRTs, researchers Reference Glover, Arts and Babu17 found that admissions nationally fell 11% between 1998 and 2004. However, in the 34 primary care trusts that had CRTs, admissions had fallen by 10% more - and by 23% more in the 12 primary care trusts with teams that were on call 24 hours a day - although CRTs had not made a significant difference in bed use. Reductions in admission were most noticeable in more established teams and variability may also arise as, despite being conceptualised as gatekeeping all potential admissions, the National Audit Office found CRTs typically involved in only 53% of admissions and had influenced the decision to admit in only 46%. Reference Morgan18 Contemplating CRTs further reducing admissions must be contextualised by consideration that current bed numbers may be close to a practical minimum. Reference Lelliott19 An interesting finding was work showing a relationship between CRT introduction and increased length of admission. Reference Keown, Tacchi, Niemiec and Hughes12 The interpretation of this is open to debate, but a posited explanation is that CRT gatekeeping means those actually admitted were typically more ill; alternatively, it is conceivable that fewer admissions resulted in less ward pressure to discharge.
Gatekeeping crisis admissions and risk Tyrer and colleagues Reference Tyrer, Gordon, Nourmand, Lawrence, Curran and Southgate15 found a higher number of deaths by suicide in an area covered by a CRT compared with another area locally that had none, and compared with the same area 9 months before CRT introduction. Conversely, another study Reference Keown, Tacchi, Niemiec and Hughes12 found that suicide rates remained constant, concluding that CRTs are as safe as standard hospital care. Whether CRTs, by keeping individuals in crisis in the community, have increased risk has been - surprisingly, given their role - under-explored.
Involuntary admissions
Since 1999, the number of detentions under the Mental Health Act 1983 has remained relatively stable 20 - with some increase in Section 2 and reduction in Section 3 admissions - contrary to expectations that CRTs would decrease use of the Act. Nine studies investigating this have had mixed results, with two reporting a decrease, one of which was not significant; two no difference; and five reporting an increase (Table DS1). One study Reference Furminger and Webber21 used focus groups to qualitatively explore this: staff inferred that if the CRT referred patients for a Mental Health Act assessment then the ‘least restrictive option’ had already been attempted, with the next logical option detention under the Act. Further, approved mental health professionals expressed increasing difficulty negotiating informal admissions with ward staff and felt compulsory admission was the only way to get the patient admitted. The decreased use of Section 3 may be related to the fact that CRTs facilitate early discharge, Reference Furminger and Webber21 although changes in culture and practice of the Mental Health Act assessments may have contributed. Keown and colleagues Reference Keown, Weich, Bhui and Scott22 reported that involuntary admissions had increased by 64%, directly associated with a reduction by 62% in provision of beds: the authors suggested that non-availability of beds was causing delays in or unfeasibility of planned admissions, resulting in patients deteriorating to such an extent that they required compulsory admission. However, although this has also been suggested elsewhere, Reference Keown, Tacchi, Niemiec and Hughes12,Reference Tyrer, Gordon, Nourmand, Lawrence, Curran and Southgate15 there is no current empirical evidence for this hypothesis.
Clinical profiles of patients admitted to hospital despite the introduction of CRTs
Seven observational studies addressed this question (see online Table DS2 for characteristics of included studies). The most common reason for admission was risk to self. Reference Brimblecombe, O'Sullivan and Parkinson31-Reference Tomar, Brimblecombe and O'Sullivan33 Brimblecombe and colleagues Reference Brimblecombe, O'Sullivan and Parkinson31 found that 21.1% of patients taken on by CRTs were later admitted: 53.2% due to risk to self; 11.3% due to risk to others; and 8.1% as carers could not cope. However, another study Reference Cotton, Johnson, Bindman, Sandor, White and Thornicroft34 found those at risk of violence or unintentional self-harm through self-neglect or recklessness were more likely to be admitted than those at risk of ‘deliberate’ self-harm. Uncooperativeness was also cited as a reason for admission. Reference Brooker, Ricketts, Bennett and Lemme32,Reference Cotton, Johnson, Bindman, Sandor, White and Thornicroft34 Psychosis was associated with hospitalisation in some work, Reference Guo, Biegel, Johnsen and Dyches28,Reference Cotton, Johnson, Bindman, Sandor, White and Thornicroft34 although others found no diagnostic differences, Reference Tomar, Brimblecombe and O'Sullivan33,Reference Harrison, Alam and Marshall35 with one study Reference Tomar, Brimblecombe and O'Sullivan33 also finding no significant differences in demographic variables in those admitted. Overall, research findings have been inconsistent.
Are CRTs cost-effective?
Eight studies addressed this question (see online Table DS3 for characteristics of included studies). One of these Reference McCrone, Johnson, Nolan, Pilling, Sandor and Hoult36 re-analysed previously reported RCT data, Reference Johnson, Nolan, Pilling, Sandor, Hoult and McKenzie9 three were ‘pre- and post-CRT comparisons’, Reference Damsa, Hummel, Sar, Di Clemente, Maris and Lazignac26,Reference Ford, Minghella, Chalmers, Hoult, Raftery and Muijen27,Reference McCrone, Johnson, Nolan, Pilling, Sandor and Hoult37 one compared police and crisis handling of psychiatric emergencies, Reference Scott30 and one was a national audit using a decision model. Reference McCrone, Knapp and Hudson38 Overall, as might be expected, the CRTs were less expensive than in-patient care, although no statistical testing was reported in some work. Reference Damsa, Hummel, Sar, Di Clemente, Maris and Lazignac26,Reference Scott30 One ‘pre- and post-CRT comparison’ Reference Scott30 found that the average case cost was US$1520 for the crisis service and US$1963 for the police intervention. The second study Reference Damsa, Hummel, Sar, Di Clemente, Maris and Lazignac26 compared two 6-month periods before and after the introduction of a CRT, and found that in-patient care costs fell sufficiently to more than cover the small rise in emergency care costs. The third study Reference Ford, Minghella, Chalmers, Hoult, Raftery and Muijen27 found no difference overall with the lower cost per individual mitigated by more people receiving acute care.
A decision model was developed by the National Health Service to estimate the costs and potential savings of CRTs. Reference McCrone, Knapp and Hudson38 This concluded that expected 28-day care costs were £630 less than if CRT treatment had not been considered. Given that roughly 50% of patients in crisis are considered for CRT, Reference Morgan18 of whom approximately 69% are not admitted, Reference McCrone, Knapp and Hudson38 estimated savings in the UK are £66 million per year. However, this model makes a number of simplifications and only applied to the period of the crisis, so the longer-term costs or savings are unknown.
Other work Reference McCrone, Johnson, Nolan, Pilling, Sandor and Hoult36,Reference McCrone, Johnson, Nolan, Pilling, Sandor and Hoult37 investigated cost-effectiveness using previously collected data. Reference Johnson, Nolan, Pilling, Sandor, Hoult and McKenzie9,Reference Johnson, Nolan, Hoult, White, Bebbington and Sandor10 Over a 6-month follow-up period CRT patients cost £2438 less than in-patients. Reference McCrone, Johnson, Nolan, Pilling, Sandor and Hoult36 In the prospective controlled trial Reference McCrone, Johnson, Nolan, Pilling, Sandor and Hoult37 the finding that a CRT patient costs less per 6 months than an in-patient was only significant when patients who had any CRT contact were compared with those that had no contact, rather than comparing pre- or post-CRT groups.
Are patients satisfied with CRT care?
Thirteen studies addressed this question (see online Table DS4 for characteristics of included studies): two systematic reviews, Reference Hubbeling and Bertram7,Reference Winness, Borg and Kim8 one RCT, Reference Johnson, Nolan, Pilling, Sandor, Hoult and McKenzie9 six quantitative analyses, Reference Johnson, Nolan, Pilling, Sandor, Hoult and McKenzie9,Reference Johnson, Nolan, Hoult, White, Bebbington and Sandor10,Reference Scott30,Reference Ruggeri, Salvi, Perwanger, Phelan, Pellegrini and Parabiaghi39-Reference Khan and Pillay41 three qualitative analyses, Reference Khalifeh, Murgatroyd, Freeman, Johnson and Killaspy42-Reference Goldsack, Reet, Lapsley and Gingell44 and two using both. Reference Barker, Taylor, Kader, Stewart and Le Fevre11,Reference Clark, Khattak, Nahal and Linde45 Some studies Reference Tyrer, Gordon, Nourmand, Lawrence, Curran and Southgate15,Reference Ford, Minghella, Chalmers, Hoult, Raftery and Muijen27 attempted to collect patient satisfaction data as secondary analyses, but had response rates considered too low to report given the issue of response bias.
All seven quantitative studies report overall positive patient experience, although the RCT Reference Johnson, Nolan, Pilling, Sandor, Hoult and McKenzie9 showed only a trend and not a statistically significant difference between in-patient and CRT satisfaction. Johnson and colleagues Reference Johnson, Nolan, Hoult, White, Bebbington and Sandor10 reported a highly significant difference in patient satisfaction pre- and post-CRT implementation, and Scott Reference Scott30 found over 85% of patients were satisfied with CRT care. Ninety-two per cent of patients who responded to a survey in one study said they would be prepared to use the service again. Reference Kalucy, Thomas, Lia, Slattery and Norris40 In another study, Reference Barker, Taylor, Kader, Stewart and Le Fevre11 93% of patients reported some clinical improvement during their CRT care, with 27% feeling totally recovered at discharge. The study also reported that 89% felt safe during CRT care and 78% felt ready to be discharged from care. In a study of ethnic variation in satisfaction, Reference Khan and Pillay41 it was found that whereas both White and Asian patients preferred home treatment to admission, explanations for this varied. For example, Asian patients showed greater concerns about religious and dietary requirements as well as greater levels of stigma surrounding hospitalisation.
Qualitative studies inevitably provide more depth of experience. One systematic review Reference Winness, Borg and Kim8 clustered its findings into three factors: access and availability; being understood as a ‘normal’ person; and dealing with a crisis in an everyday context. Patients appreciated having easy and rapid access to a service 24 hours a day, 7 days a week. Reference Hopkins and Niemiec43,Reference Goldsack, Reet, Lapsley and Gingell44 Lack of frequent or prompt communication, possibly due to demands on resources, can cause the patient much anxiety and distress. Reference Clark, Khattak, Nahal and Linde45 Two aspects of the service frequently referred to as important in interviews were the practical help the team provided and being available to talk. Practical help came in many different forms, including providing medication, helping with daily routines such as showering, doing food shopping for the patient, and help with housing difficulties such as domestic chores and coordinating and paying utility bills. Patients also reported valuing the availability of staff to talk, Reference Hopkins and Niemiec43-Reference Clark, Khattak, Nahal and Linde45 including providing advice, information about other services, emergency numbers, appointment details and psychoeducation. However, some patients reported not receiving enough information, Reference Goldsack, Reet, Lapsley and Gingell44 or receiving too much information in the form of confusing, jargon-filled leaflets.
Patients appreciated it when staff were reassuring, ‘like a friend’, and not ‘fazed’ by anything, Reference Hopkins and Niemiec43 and establishing strong relationships with staff was deemed very important to most patients interviewed. Reference Barker, Taylor, Kader, Stewart and Le Fevre11,Reference Hopkins and Niemiec43,Reference Goldsack, Reet, Lapsley and Gingell44 Patients were grateful for the hope and encouragement the team provided. Reference Goldsack, Reet, Lapsley and Gingell44 Two studies reported that patients appreciated being treated as individuals, with services flexible to their needs. Reference Hopkins and Niemiec43,Reference Goldsack, Reet, Lapsley and Gingell44 A strong association was found between the level of personal engagement in the service and patient satisfaction with the service, and its absence was mostly reported in teams that lacked resources. Reference Clark, Khattak, Nahal and Linde45
A stated detrimental feature to forming such good relationships was a lack of consistency in who visited the patients’ homes. Reference Hopkins and Niemiec43-Reference Clark, Khattak, Nahal and Linde45 However, many patients found such inconsistency acceptable if staff were adequately briefed and worked well together as a team, Reference Goldsack, Reet, Lapsley and Gingell44 with most patients understanding the nature of a shift-based service. Another concern was when patients felt the team was at full capacity, as time and resources, such as visits, could be rushed or they were given telephone calls instead. Reference Clark, Khattak, Nahal and Linde45 Patients also emphasised the need for good communication between them, the team, the social network, different staff members and different mental health teams. They appreciated when family were kept informed and were told how best to support them. Reference Hopkins and Niemiec43,Reference Goldsack, Reet, Lapsley and Gingell44 They also appreciated when they were included in decisions, Reference Goldsack, Reet, Lapsley and Gingell44,Reference Clark, Khattak, Nahal and Linde45 although another study found patients in crisis were less concerned about this as they were less capable of making decisions. Reference Hopkins and Niemiec43
Evidence suggests that patients prefer home treatment to hospital admission due to the stigma of the latter, Reference Goldsack, Reet, Lapsley and Gingell44 and they can carry on with some day-to-day activities and find ways to deal with the crisis in the context of their own life situation. Reference Clark, Khattak, Nahal and Linde45 However, some patients felt they were discharged to the CRT before they were ready, or would have preferred hospitalisation because they felt unsafe, that they were putting too much strain on their family, or because the home environment was a contributing factor to their mental health problems. Reference Clark, Khattak, Nahal and Linde45 Khalifeh and colleagues Reference Khalifeh, Murgatroyd, Freeman, Johnson and Killaspy42 assessed the impact of CRTs on mothers and their children: interestingly, although most mothers preferred home treatment because they felt better looked after at home, most children preferred hospital admission as it relieved them of distress and responsibility. Common difficulties reported by the mothers were with meeting the children’s physical needs, being dependent on the children and children witnessing distressing symptoms. Despite this, mothers were commonly reluctant to seek help with parenting because of fears their children could be taken away.
One study Reference Hopkins and Niemiec43 found most patients least satisfied with the end of treatment, either because it happened too quickly or because of poor communication with the service they were being referred to. Reference Clark, Khattak, Nahal and Linde45 These problems were not universal, however, and most patients accepted the ending of CRT care as long as they were given sufficient warning, explanation and details when changes were going to occur, and a specific plan for what they should do if a crisis were to occur again.
Discussion
Crisis resolution teams were implemented in the UK based on projected reductions on hospital admissions - both rates and durations - and compulsory detentions, improved patient satisfaction and cost savings, but without adequate evidence that they would be effective in meeting these aims. This systematic review illustrates an overall trend of falling admission rates that is massively confounded by national changes in in-patient bed numbers, although rates fell more so for areas that had a CRT, Reference Glover, Arts and Babu17 and the evidence overall supports a modest positive effect in reducing admission rates and duration. Data surrounding compulsory Mental Health Act admissions are similarly likely affected by cultural changes in practice, and evidence for the effects of CRTs on this is limited: although there is some conflict in research findings, more studies reported an increase in Mental Health Act admissions, certainly against hypothesised predictions. The most consistent findings are that patients are generally satisfied with the care received from CRTs and that such teams are cost-effective alternatives to hospital admission.
Despite their ubiquity, CRTs remain under-researched and the existing data highlight inherent difficulties undertaking research in CRTs, particularly a gold-standard RCT. Comparisons of temporally or geographically distinct data-sets are reasonable initial attempts to circumvent this, but weaken findings, particularly against an acknowledged background of change of practices and resources. The availability of in-patient beds and the lowest safe and sustainable number that can and should be provided is an emotive and widely debated issue. Positive patient feedback and constructive criticism are to be welcomed but this must be contextualised by low return rates, inevitable bias in such samples, and a wider finding that the process of asking about ‘service satisfaction’ generally produces positive results.
Other difficulties interpreting the research include the fact that CRTs vary widely in the populations they serve, both sociodemographically and operationally through inclusion and exclusion criteria, and their relations and referral routes with primary care, in-patient wards, community teams and so forth. There is no agreement on the exact size, staffing profile or working hours for such teams, and even where and when they operate it is clear CRTs are not gatekeeping all admissions. Admission rates and duration are the most commonly studied factors, most likely as they are key conceptual functions of such teams as well as the fact that they are ostensibly ‘easier’ and more objective markers to evaluate, although the problems with this are noted above. Our inability to meta-analyse the existing data underscores the need to adhere to statistical conventions of presenting appropriate measures such as error measures. There is a stark lack of data on risk and longer-term outcomes: do CRTs longitudinally modify factors such as self-harm, readmission rates or social markers of functioning?
We are all entering a brave new world of primary care commissioning and payment by results. Presumed continuance of existing practice and staffing levels, particularly in the face of underwhelming evidence, is not viable. Difficulties with RCTs in emergency or crisis services are inherent, but there are ways around this, including active controls in a ‘standard’ v. ‘enhanced’ trial. Undertaking this, particularly in a larger multisite study, would allow an attempt to tease out team confounders around the nature of service provided, and patient confounders such as the nature and duration of illness and sociodemographic factors. Incorporated into this - or circumventing it completely through alternative naturalistic methodology - longer-term follow-up studies are required.




eLetters
No eLetters have been published for this article.