Actions to address the rising levels of obesity and type 2 diabetes (T2D), which predispose people to CVD, are a health-care priority(1–3). There is a particular need for culturally specific educational interventions targeted at black and minority ethnic groups, including South Asian populations(Reference Fox4–Reference Stockley6). In 2001, approximately two million ethnic South Asians were living in England and Wales(7). Approximately 215 000 South Asians were living in North West England(7) and this population is growing faster than those of other minorities(8).
South Asian men and women have a 2-fold and 1·5-fold higher risk of T2D, respectively, than the general population(9). Central obesity is more common in South Asians than in Caucasians(Reference Fox4, 9, Reference Bhopal, Unwin and White10) and is particularly prevalent in Pakistani women(Reference Bhopal, Unwin and White10, Reference Harwood, Mytton and Watkins11). Overall, South Asians are approximately 50 % more likely to die from CHD than the general population(Reference Fox4). In the South Asian context, women's health is devalued and neglected(Reference Fikree and Pasha12).
Dietary differences are likely to contribute to these health inequalities(Reference Fox4, Reference Parillo and Riccardi13, Reference Lovegrove14). Although dietary profiles of South Asians vary, the consumption of saturated fats is typically high and the consumption of fruit, vegetables and dietary fibre is sometimes low(Reference Fox4, Reference Kassam-Khamis, Judd and Thomas15, Reference Varghese and Moore-Orr16). Socio-cultural factors strongly influence dietary habits among South Asians. Important factors include Islamic guidance, cultural beliefs, family roles and expectations, language barriers, health knowledge and the level of acculturation(Reference Greenhalgh, Helman and Chowdhury17–Reference Choudhury, Brophy and Williams23). As South Asian women have a principal role in food preparation, measures to improve their understanding of food and health are particularly important if community-wide changes and effects are to be achieved.
Culturally specific diet and health education programmes have been implemented locally(Reference Fox4, Reference Stockley6, Reference Farooqi and Bhavsar24–Reference Davies, Damani and Margetts26). However, levels of cultural competency among health professionals working with South Asians require further improvement. The present qualitative study, conducted by a second-generation Pakistani (and a second-generation female translator) and two non-Pakistani researchers, aimed to assist this process by:
1. exploring health perceptions and diet that may contribute to the increased incidence of diet-related diseases and to cultural body image perceptions of obesity;
2. exploring the understanding of perceived health risks and the social construction of obesity;
3. elucidating the relevant barriers and motivations for dietary and lifestyle choices; and
4. developing a framework to better understand the factors underlying the women's health behaviours and how this relates to the initiation and maintenance of a healthier diet.
Methods
Participants
The study recruited first- and second-generation Pakistani women in Greater Manchester, England. Purposive recruitment and enquiries at community centres(Reference Campbell and McLean20) were used, or ‘snowballing’ (via personal contacts) and word of mouth. Efforts were made to include both English- and non-English speaking women, and (voluntary or involuntary) hard-to-reach women (e.g. defined as unable to drive or not permitted to leave home(Reference Hawthorne25)). Informed verbal consent was gained from all participants and the project received ethical approval from the University of Chester Research Ethics Committee.
Focus groups and individual interviews
Initially the study used both ethnographic and phenomenological approaches. Ethnography uses unobtrusive cross-cultural observations and informal discussions (e.g. with shopkeepers in South Asian food shops) as a means of interpreting social reality(Reference Savage27). Phenomenology aims to uncover meanings, without explanation, of a reality that is socially constructed through lived experiences. This allows for the description of realities as perceived by individuals within their community and the host community(Reference Fade28).
The researchers gathered data from participants during small focus groups, lasting approximately 1 to 2 h, or one-to-one interviews, lasting from 15 to 60 min. They were conducted in community centres or participants’ homes, in English and Urdu, and were led by either a Caucasian or a Pakistani researcher, experienced in qualitative methods, along with a trained female Pakistani translator. A pilot focus group session was conducted among seven Bangladeshi Muslim women.
All sessions involved using fictional vignettes, as previously used in health studies among South Asians(Reference Greenhalgh, Helman and Chowdhury17), interspersed with open-ended questions (e.g. ‘Why is Farah overweight?’). A vignette is a short description or character sketch of a person or story. The researchers drafted fictional vignettes involving a character named ‘Farah’, a 38-year-old, married, overweight Pakistani mother of four, living in Manchester. This technique was used to explore issues such as obesity, food, health, fatalism, faith, age and family dynamics. According to the method of progressive focusing where new and emerging issues are explored(Reference Coveney29), the vignette was adapted as the need for new data became apparent (e.g. exploring motivators). In total, five versions were used. Subtle references were made within the vignette to T2D (Farah being thirsty and tired), while later versions focused on her as a mother (e.g. with an overweight son) and wife (e.g. with an unwell husband). Comparing responses allows for further theories to emerge.
The participants were also shown a series of seven female silhouettes ranging from an underweight figure to an obese figure, i.e. representing an un-stated BMI of 17 kg/m2 to 35 kg/m2 (Fig. 1). These were used to explore the women's perceptions of body shape, as applied to Farah.
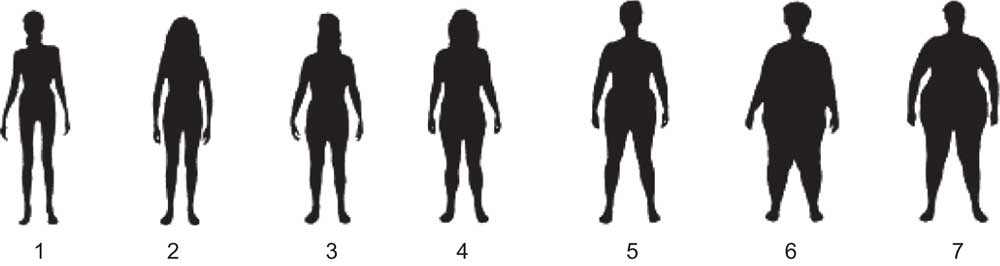
Fig. 1 The seven female silhouettes ranging from an underweight figure to an obese figure (representing an un-stated BMI of 17 kg/m2 to 35 kg/m2), used to explore the women's perceptions of body shape. Reprinted with permission from ‘The Body Test’ (1988). © Dietitians of Canada
All interviews were recorded and transcribed verbatim. For all sessions, selected second-generation women who read English were sent copies of their transcripts for member-checking, amending as necessary. The translator clarified nuances within the transcripts of the non-English speaking first-generation women.
According to recommendations for qualitative research(Reference Pope, Ziebland and Mays30), sampling ceased when no new themes emerged from the data collected.
Demographic data were collected using a questionnaire. These data included age, marital status, number of children, birthplace and how much education they had received. The women were asked to estimate how frequently they ate Pakistani v. English meals or ate away from home each week.
Analysis
The transcripts were initially analysed using theme identification and coding. The phenomenological analysis aimed to intensify the researchers’ understanding of the text in its constituent parts, using the method of Van Manen(Reference Van Manen31). The text was broken down and categorised manually into domains of Time, Space, Body and Human Relations (van Manen themes) with the added domains of Foodways(Reference Kassam-Khamis, Judd and Thomas15) and Health Beliefs (authors’ themes). The data were placed within each theme and then coded to identify sub-themes. Following the initial analysis (by A.F.L. and B.E.), additional interpretation and analysis of the emerging themes was then provided by a sociologist (P.C.) according to researcher triangulation. This process aims to reduce bias and is designed to enhance validity(Reference Draper32).
The sociological analysis allowed the researchers to ‘see’ the participants from a new perspective, taking into account the influences involved. This perspective formed the social construction of obesity beyond its biomedical definitions. The researchers sought to elucidate the participants’ understanding of health risks, knowledge, prevention, barriers and motivators for diet and lifestyle.
Results
Participants
Fifty-five women participated in six focus groups or ten one-to-one interviews. The first-generation women (n 44), median age 45 years, were born mainly in Pakistan (Table 1). The median age for the second-generation women was 32 years (overall range 23–80 years). Education levels ranged from no formal education (n 9) to post-graduate (n 2). Among first-generation women, 80 % had some education; whereas 100 % of second-generation women were educated. In the following, italicised quotes show the data gathered about Farah.
Table 1 Characteristics of the study participants: Pakistani women, Greater Manchester, UK
*One woman was not sure of her age.
Phenomenological analysis
Diabetes symptoms
The participants did not recognise Farah's symptoms of thirst and frequent tiredness as being suggestive of T2D. Some believed that Farah was not well and suggested tuberculosis, cancer or being overweight, and that she was not eating or drinking properly. A 50-year-old mother stated: ‘She's [Farah] not eating properly so her health is suffering. She probably can't work in the house any more. She could have some illness … she is too fat.’
Reasons for overweight
Reasons cited for Farah's weight gain included childbirth, her age (at 38 years she was considered ‘old’ by some participants) and inactivity.
Health action
Overall the women did not express a preference for a source of sound health advice. Some stated that they would consult a doctor, nurse, health visitor or social worker. However, others sought advice from elders: ‘I think professional doctors and nurses, we can find out from them … but mostly … we follow the tradition we learn from our parents.’
Motivation to change
A lack of motivation to address weight problems was expressed as: ‘Women tend to not think about themselves and don't like seeing their bodies.’ Barriers, evident among first-generation women, included the influence of the men in the family on home cooking, weight gain as being natural and unavoidable, and there appeared to be a lack of concern for preventing illness (‘… food has nothing to do with it, when your time's up, your time is up …’). The prevailing attitude seemed to be that health and weight gain were not things the women often thought about, as they were too ‘busy’. However, some women described themselves (and Farah) as ‘lazy’ in terms of taking exercise (e.g. walking) or changing their cooking habits.
A principal motivating factor was the need to look after their children and home and they sensed that they should do something about their weight when it caused pain.
Sociological analysis
Identity deconstruction: Muslim, Pakistani, British
Separating ‘dimensions’ of ethnicity was difficult, as reported by previous researchers(Reference Campbell and McLean20, Reference Nazroo33). The Muslim identity, described as being ‘100 % complex’, seemed to be the strongest identity as it dictated food habits. It has been suggested that Muslims are likely to learn about health from their mosque and the Koran(Reference Beishon and Nazroo34). However, the Koran was not a constant source of food information except for halal (meaning permitted; e.g. fruits, vegetables, nuts, honey, milk, meat slaughtered according to Islamic law)(35, 36) and haram (e.g. not permitted) foods (e.g. pork, lard, etc.) and alcohol avoidance(35, 36). The Pakistani cultural and spiritual identity was the second strongest influence. Among second-generation Pakistani women, the British identity may have been as strong as their Pakistani identity.
Family
Family life is essential and sacred within Islamic society. Women are assigned the ‘duty’ of looking after the household and act as ‘culture-bearers’. Indeed, the interests of family often took precedence over those of the individual woman, as has been previously reported(Reference Campbell and McLean20, Reference Mellin-Olsen and Wandel22). This is likely to diminish motivation and opportunities to address weight gain. Conversely, it could also provide motivation to change, as the participants acknowledged that weight gain and illness could interfere with family duties.
Emergent themes
Risk awareness. The participants did not always connect obesity with diabetes. One mother of eight perceived that diabetes was caused by stress, as previously reported among South Asians(Reference Greenhalgh, Helman and Chowdhury17, Reference Khajuria and Thomas37). Another woman from Rawlpindi understood a connection between obesity and diabetes, but believed that the former resulted from the latter.
Urban v. rural background. The women's region of origin may affect beliefs and practices, including education level, English literacy, empowerment and activity levels. For example, participants stated that urban women may have access to an English education and be more empowered within their marriages. However, some women suggested that the rural life might be beneficial, in terms of the climate, fresh air and the level of activity.
Climate. Participants often blamed the colder British climate for weight gain, because it caused them to sweat less and to engage in less outdoor activity. Such associations have been reported previously among South Asians(Reference Greenhalgh, Helman and Chowdhury17, Reference Mellin-Olsen and Wandel22). Some women also linked the appropriateness of the traditional diets with climate, i.e. eating clarified butter (ghee) was acceptable in Pakistan where women were more active.
Food traditions/expectations. Typically, food was prepared from scratch every day using recipes passed down by word of mouth and was described as being ‘healthier’. Most of the participants reported eating such food at least once a day, often in the evening with the family. Breakfast was sometimes described as an ‘English meal’ at which South Asian food was rarely eaten, as has been reported in other studies(Reference Khajuria and Thomas37).
There was a strong influence of family expectations (including male dominance) on food preparation (e.g. the amount of oil used in curry) and consumption. Generally, younger Pakistani women received advice (whether it was asked for or not) from their elders. Pakistani men also have a responsibility for maintaining traditional cultural practices(Reference Campbell and McLean20). The social importance of cooking for guests and of celebratory meals was described. Hence, it may be difficult for the Pakistani woman to change food practices.
Some women described eating their family meals while sitting on the floor, rather than around a table. One second-generation woman explained this as a traditional means of controlling the amount eaten: legs closer to the stomach was said to reduce the amount eaten.
English v. Pakistani food. Some perceived that English food is processed ‘fast’ foods and breakfast-type foods. The women had mixed perceptions of Pakistani food, as it was perceived to have many healthy ingredients (including ginger and garlic), but also could be unhealthy, such as common use of fat and frying. Other ingredients were considered to have specific benefits, e.g. karela (thought to counteract diabetes), black onion seeds and honey. Certain food combinations were considered inadvisable (e.g. it was suggested that eating fish and milk together could cause skin conditions).
According to questionnaire data, first-generation women consumed more traditional meals (6·3 meals/week) than English meals (2·0 meals/week). Second-generation women ate slightly fewer traditional meals and reported eating slightly more meals away from home each week (Table 2). Chips and beans seemed to be a favourite English meal (a halal option). Some were aware that eating takeaway meals could be unhealthy.
Table 2 Mean number of times per week the participants reported to eat Pakistani meals, English meals or takeaways, according to country of birth: Pakistani women, Greater Manchester, UK
*Forty participants were born in Pakistan, three were from India and one from East Africa, although all considered themselves ‘Pakistani’.
Obesity and health. Perceptions of a healthy and overweight women's body size varied. When asked what the ‘overweight’ Farah looked like, the participant's responses ranged from silhouettes 4 to 7 corresponding to a BMI of 22·5 kg/m2 up to 35 kg/m2. Silhouette 3, corresponding to a BMI of 20 kg/m2, was generally considered the healthiest.
Increased weight may not always be perceived as unhealthy and may be viewed as indicating good health, wealth or status(Reference Greenhalgh, Helman and Chowdhury17, Reference Mellin-Olsen and Wandel22). Body shape perceptions may also be affected by modesty traditions and some pointed out that a woman dressed in traditional clothing was not always aware of her shape.
Table 3 summarises other potential differences in the viewpoints between British Pakistani women and health professionals.
Table 3 Some possible differences between the health and lifestyle viewpoints of British Pakistani women and UK health professionals
Health Action Transition model
To our knowledge, existing health models do not take account of the information obtained in the present study. Accordingly, a new Health Action Transition model of health improvement in first-generation Pakistani women in North West England is proposed (Fig. 2). The model allows the multi-directional dimensions underlying the construction of health and its impact on dietary change to be addressed.
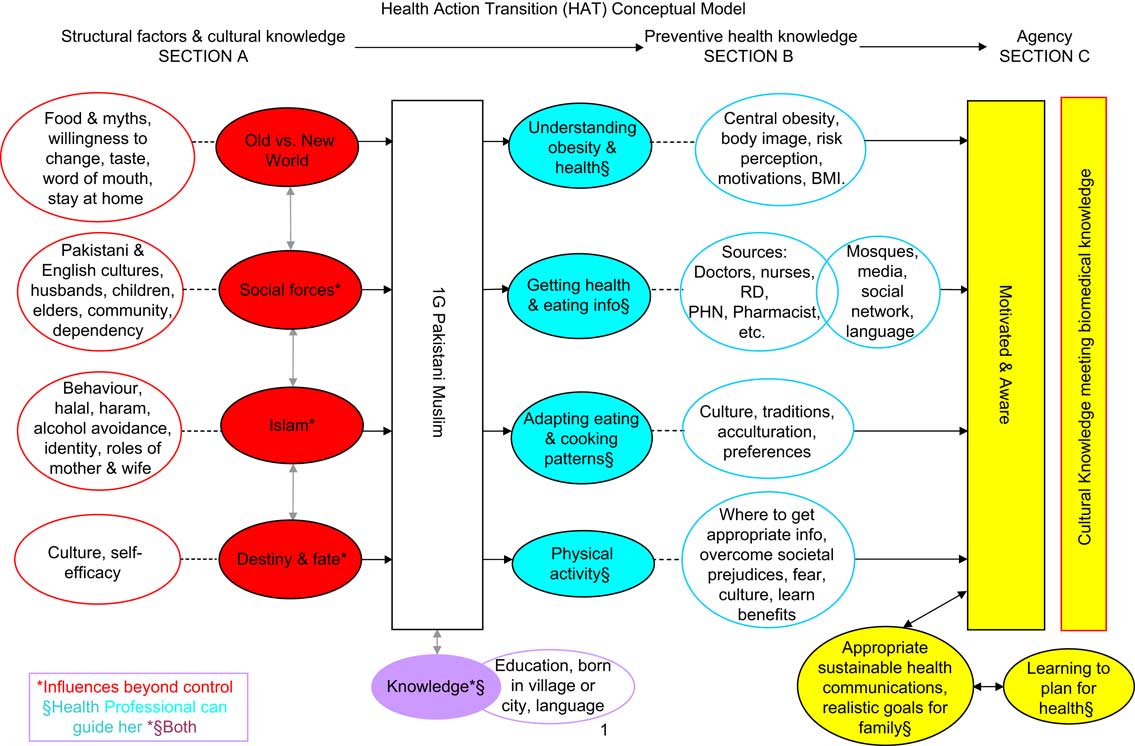
Fig. 2 The newly proposed Health Action Transition conceptual model of health improvement in first-generation Pakistani women in North West England. ![]() represent the background influences (uncontrollable) and
represent the background influences (uncontrollable) and ![]() the interconnected factors;
the interconnected factors; ![]() represent professional guidance (controllable) and
represent professional guidance (controllable) and ![]() their related actions, location and time;
their related actions, location and time; ![]() are those influences both controllable and not (RD, registered dietitians; PHN, public health nutritionists)
are those influences both controllable and not (RD, registered dietitians; PHN, public health nutritionists)
The model is in three parts: Section A is entitled ‘Structural Factors and Cultural Knowledge’, Section B is ‘Preventive Health Knowledge’ and Section C is ‘Agency’. Section A represents the uncontrollable aspects in the woman's life and Section B represents the controllable aspects via increased health knowledge. The boxes on the far left of Section A represent the woman not yet taking responsibility for her health or possibly being unmotivated to act (as perceived by the health professional). Moving to the right, the circles then delineate concepts (or ‘dimensions’) related to her understanding of health, obesity, foodways and cooking patterns. Section B suggests that the Pakistani woman will ideally be influenced by various health professionals and not just by her peers and elders. Rather than considering weight gain as inevitable, this woman takes control of her health.
Section C is the stage which health-care professionals would ideally wish her to reach. The model should help health professionals understand that certain influences are uncontrollable and that she might have a strong sense of predestination. Respecting these issues, health professionals can promote preventive measures that can help the woman take some responsibility for protecting her long-term health, for example in making informed decisions about weight loss. By taking these complexities into consideration, health professionals can encourage healthier behaviours in the Pakistani woman, who will then extend these to her family and community.
Discussion
The present qualitative study aimed to provide insight into the social and cultural constructs underlying perceptions of diet, weight gain and health risks among British Pakistani woman in North West England, and how these relate to Westernised biomedical models, in order to facilitate efforts to promote good eating practices and address health inequalities.
Qualitative research methods are valuable in allowing the exploration of complex behaviours, attitudes and interactions(Reference Mays and Pope38) and have previously been used to explore diet and health in South Asians(Reference Greenhalgh, Helman and Chowdhury17, Reference Fagerli, Lien and Wandel21, Reference Choudhury, Brophy and Williams23, Reference Bandesha and Litva39, Reference Fagerli, Lien and Wandel40). Various socio-cultural factors can hamper research among South Asian groups, especially women. Accessing women who are mostly housebound can be difficult. If perhaps unused to giving their opinion, such women may be concerned about giving the ‘right’ answer. Some may be reluctant to discuss health and weight issues. The current research reached a cross-section of Pakistani women, including non-English speaking and the hard-to-reach. It employed a South Asian researcher and translator in order to aid access and communication and to apply both ‘insider’ and ‘outsider’ perspectives. The analysis was also enhanced by rigorous qualitative research methods and a sociological perspective.
Strengths and limitations
Common limitations in qualitative and transcultural research include the use of relatively small samples and the need to translate and interpret interviews. It could be argued that a study limitation was the use of a non-Pakistani moderator and the broader applicability of these findings needs to be tested. Data concerning the socio-economic status of the women and length of UK residency were not collected. The usefulness of BMI silhouettes was limited because they represented weight gain in Caucasian women, characterised by hip adiposity, rather than in South Asian women, who tend to accumulate fat centrally. Furthermore, BMI thresholds for diabetes risk are lower in South Asian women than in Caucasian women(41).
Pakistani women, food and health
The present study supports evidence of a lack of understanding about T2D and its relationship with weight gain among South Asians(Reference Choudhury, Brophy and Williams23) and demonstrates that preventive measures are still required(Reference Mather and Keen42). The participants expressed concerns about weight gain, including the contributory roles of stress, climate, age and childbirth, many of which have been reported previously(Reference Greenhalgh, Helman and Chowdhury17, Reference Mellin-Olsen and Wandel22, Reference Khajuria and Thomas37). Importantly, the women expressed a strong sense of fatalism with regard to health risks and weight gain (also previously reported) but desired more health knowledge.
Multiple dimensions of identity were exhibited, including being Muslim, Pakistani, British, female and mothers. For the second-generation women, Islam is considered in relation to halal and haram food (e.g. checking food labels for vegetarian or halal ingredients) when shopping in a non-Asian food store. The women were strongly influenced by cultural traditions and family expectations with regard to food preparation and consumption, and these represent important barriers to change. The study supported other evidence that South Asian groups prefer traditional food over English food(Reference Jamal43). The women adhered to traditional Pakistani food habits, important to them, socially and culturally. Radical changes to these habits would be neither possible nor desirable for them. Other researchers have identified these influences on diet and food shopping, together with factors such as age, lack of time, language barriers, climate and access to foods(Reference Mellin-Olsen and Wandel22, Reference Farooqi and Bhavsar24, Reference Bandesha and Litva39, Reference Lawrence, Devlin and Macaskill44). Cultural barriers may outweigh personal motivation for weight loss, such as personal appearance(Reference Farooqi, Nagra and Edgar45).
The prioritisation of the family's expectations and needs concurs with other evidence that exercise beyond housework is considered selfish by some South Asian women(Reference Sriskantharajah and Kai46). These perceptions may be at odds with individualistic motivations in commercialised healthy living (e.g. gym membership) and with individualistic models of behaviour change that involve concepts such as self-efficacy or empowerment. However, family concerns could be a motivator where weight gain compromises the woman's role as family carer. Also, the health of the children or husband may also be an important motivator towards dietary change.
This familial collectivism suggests that conventional health models that place emphasis on individuals and their self-efficacy (e.g. the Health Belief Model(Reference Conner and Norman47)) may not be readily applicable to South Asian women.
Health promotion and education
Many of the aforementioned barriers to research in South Asian groups also hamper nutrition and health intervention programmes(Reference Fox4, Reference Hawthorne25, Reference Fagerli, Lien and Wandel40, Reference Thomas48). Experience from a health project among South Asians in Manchester has illustrated the difficulties in engaging communities and the importance of addressing wider social determinants of health, beyond ethnicity(Reference Bandesha and Litva39).
The food and health practices of the participants in the present study were strongly influenced by their peers and elders. This reinforces that family-based educational interventions are useful in these communities. The participants did appear to recognise the important role of health-care professionals, however. Other recent evidence also suggests that South Asian women may be strongly, though passively, influenced by their doctor's recommendations and that word of mouth may have an important role in promoting programmes(Reference Choudhury, Brophy and Williams23). Other evidence suggests that Pakistani-born people with diabetes expect empathy and care from health workers, rather than an authoritarian style(Reference Fagerli, Lien and Wandel40).
Positive aspects of traditional food practices should be reinforced, including cooking from scratch using a variety of fresh and healthy ingredients (such as ginger and garlic) and family meals. The importance of breakfast and lunch should also be emphasised. Only recently have validated tools been developed to assess diets in this group(Reference Sevak, Mangtani and McCormack49) and capturing the complexity of these diets remains a challenge.
Health Action Transition model
Various models have been developed to describe and facilitate behaviour change with regard to health(Reference Greene, Rossi and Rossi50–Reference Baranowski, Cullen and Nicklas52) and ideally should be culturally and socially sensitive(Reference Kelly53). Designed in response to the findings, a new conceptual model was developed to consider public health nutrition and health promotion planning within a sociological context. To our knowledge it is the first model to describe the cultural and sociological influences among Pakistani women with regard to diet, weight gain and health. It is designed to demonstrate the complexity of the interwoven influences on the Pakistani woman and to help the health professional engage with her using concepts beyond BMI or waist circumference measurements.
The model implies a continuous progression (with a positive health-related outcome) from awareness through to initiation and maintenance of action. It also demonstrates a sustained educational process in which many controllable influences and motivators may contribute (e.g. general practitioners’ surgeries, Asian food suppliers and stores, community centres and children). Some forces may be uncontrollable (e.g. Islamic food laws and family/societal roles). According to this model, the woman maintains her traditional ways of cooking and eating patterns but understands the risks associated with overweight/obesity and becomes more aware of healthier habits (e.g. using less oil or salt). Step by step she will take responsibility by taking control of her health, applying this knowledge to her family and community.
The model may be used to tailor preventive health information that integrates cultural beliefs with biomedical knowledge. Moreover, it may be used to improve cultural awareness among health professionals (particularly dietitians and nutritionists) working with and counselling Pakistani women about weight management and as an educational tool in the training of these professionals.
Conclusions
Health education programmes that aim to address obesity and its associated risks in South Asian communities must take into account the complex beliefs and practices and the multiple religious, ethnic and social identities that interact within this population. The present study provides further insight into these factors and proposes a Health Action Transition conceptual model for use in designing and implementing education interventions for British Pakistani women.
Acknowledgements
Partial funding for the study was received from Dr Mahmood Adil, Department of Health, North West Government Office. The authors have no conflicts of interest. A.F.L. is the field researcher and lead analyst; P.C. is an independent sociologist and secondary analyst; B.E. is the corresponding author, project lead, co-field worker and secondary analyst. The authors wish to thank Mrs Hina Akhtar (translator) and the many women who participated in the study. They also acknowledge the assistance of Mr Lee Baker in the development of this manuscript.









