The rising prevalence of childhood obesity has been a global pandemic, not only in developed countries but also in developing countries(Reference Lobstein, Jackson-Leach and Moodie1,Reference Ng, Fleming and Robinson2) . Obesity during childhood is not only associated with an increased risk for impaired glucose tolerance and hypertension but also can increase the risk of chronic diseases including diabetes and some cancers during adulthood(Reference Simmonds, Burch and Llewellyn3,Reference Spear, Barlow and Ervin4) . Data from the 2014 Chinese National Survey on Students Constitution and Health indicated that among Chinese students aged 7–18, 9·4 % of boys and 5·1 % of girls were obese and the prevalence has increased dramatically from 1985 to 2014(Reference Wang, Dong and Wang5). Given the substantial rise in the prevalence of obesity among children, modifiable behavioural factors such as exercises and diet have been paid more attention compared to non-modifiable factors such as genetics(Reference Anderson and Butcher6).
Many individual-level factors related to physical activity (PA), sedentary behaviours (SB) and dietary behaviours have been identified to be determinants of childhood obesity(Reference Mead, Brown and Rees7). Familial characteristics such as parental weight status and socio-economic status also play important roles in these processes(Reference Manios, Androutsos and Katsarou8). Nonetheless, as recognised by the theoretical framework of the ecology of human development(Reference Bronfenbrenner, Morris, Lerner and Damon9), child development is the results of the complex interplay of not only the individual factors but also the environmental factors at multiple levels. Given the children spend regularly much time in the school setting, and the provisions, guidelines, activities and facilities within schools are accessible to all students, school is believed as a key environment to have population-level and long-lasting impact on children’s obesity. Indeed, most childhood obesity interventions were school-based(Reference Lobstein, Jackson-Leach and Moodie1). However, a systematic review analysed the evidence of school-based intervention for obesity and found mildly effective in reducing BMI among children(Reference Sobol-Goldberg, Rabinowitz and Gross10). In order to effectively design and implement obesity prevention strategies in schools, it is necessary to identify which school-level characteristics are related to obesity in students.
For now, a growing number of studies focused on the impact of school-level characteristics on students’ obesity-related behaviours. Some studies aimed to identify the association between the built environment and PA in school children and found that the increased accessibility to PA facilities may facilitate the PA level of students(Reference Button, Trites and Janssen11,Reference Haug, Torsheim and Samdal12) . Other studies reported that providing more physical education lessons, intramural and interschool programmes also has a favourable effect on improving students’ PA level(Reference Hobin, Leatherdale and Manske13,Reference Leatherdale, Manske and Faulkner14) . A cross-sectional study conducted in Xi’an, China, also suggested that less extracurricular exercise and sports meeting were related to less PA in adolescents(Reference Li, Dibley and Sibbritt15). Similar results were observed with respect to food choice of school children. Students’ intake of low-nutrient energy dense food and their BMI decreased in schools which followed the nutrition policy and restricted the availability of unhealthy foods(Reference Masse, de Niet-Fitzgerald and Watts16). However, only a few school-level PA-related characteristics have been found to explain the variance in students’ overweight or obesity(Reference Leatherdale17,Reference Leatherdale, Pouliou and Church18) . Even though some evidences in China suggested that school food environment (e.g. cafeterias and campus food stores) was associated with the prevalence of overweight/obesity in schools(Reference Jia, Li and Xue19,Reference Li, Xue and Wen20) , only a limited number of school-level characteristics were reported in these studies. Some other potential variables, such as school personnel and health management, were not taken into consideration.
The lack of evidence exploring multiple characteristics related to obesity in school environment is still an important gap in the literatures. Hence, in order to provide evidence for prevention and control of childhood obesity in Chinese primary schools, the present study aimed to investigate the broader range of school-level characteristics and to identify which school-level characteristics are related to obesity with consideration of individual-level characteristics.
Methods
Participants
This cross-sectional study was conducted in primary schools from an urban district and a rural district of Beijing, China from 2015 to 2016. All the public primary schools with at least fifty students at grade 4 were invited to complete the school-based obesity prevention survey. In total, thirty-seven of the forty-three schools (86 %) which meet the inclusion criteria provided the principal approval for the study. In the thirty-seven schools, 2–3 classes were randomly selected from all classes in grade 4 of each school. All the students with their parents’ informed consents were enrolled from each selected class. Of the 2480 students enrolled at grade 4 from thirty-seven primary schools, we finally included a total of 2201 students who had no vital organ diseases or disability and provided their parents’ informed consents.
Data collection
Outcomes
Anthropometric measurements of students were conducted by the professional team of the district-level Primary and Secondary School Health Center according to the standard protocol(21). Students were required to wear light clothing and be barefooted when being measured. In order to guarantee the measurement quality and control the measurement error, 3 % of those students were additionally selected randomly to be measured for the second time in each survey day. Weight was measured using the lever weight scale and recorded to the nearest 0·1 kg. Height was measured using the wall-mounted stadiometer and recorded to the nearest 0·1 cm. BMI was calculated as weight divided by height squared (kg/m2). Obese children were defined according to BMI categories based on International Obesity Task Force criteria for Asian children, and children defined as thin, normal and overweight were classified as non-obese(Reference Cole and Lobstein22).
Individual-level variables
Individual-level variables included student and family variables. Student variables were collected by a self-administered questionnaire. The students completed the questionnaire during school time guided by two trained investigators. The questionnaire included information on sex, age, PA, SB and dietary behaviours. For PA, daily duration of moderate-to-vigorous physical activity was reported based on a validated 7-d Physical Activity Questionnaire(Reference Liu, Ma and Zhang23). Students were also asked whether or not they liked sports very much (Yes or No) as an additional indicator of PA. For SB, daily duration of watching TV/movies, playing video/computer/iPad/phone and doing homework were reported. Average daily screen time and homework time were classified into ≤2 h/d and >2 h/d separately in accordance to previous studies(Reference Galan, Boix and Medrano24). For dietary behaviours, weekly frequencies and servings of vegetables, fruits, meat, milk and sugar-sweetened beverages intakes were investigated with the questionnaire designed based on the validated Block Kids Food Screener(Reference Hunsberger, O’Malley and Block25). Students were also asked whether or not they perceived their eating speed is lower than the other students in the class (Yes or No) as an additional indicator of dietary behaviours.
The family variables were collected by asking one of the student’s caregivers to complete questionnaire, including the parents’ weight, height, education and occupation. Previous studies have demonstrated the validity of self-report weight and height in adults(Reference Wada, Tamakoshi and Tsunekawa26). BMI was calculated, and categories were defined according to the WHO classification of overweight and obesity for adults(27). Family socio-economic status was estimated by Green Score(Reference Green28). Parents’ education and occupation were used to calculate the Green score, i.e. Green Score = 0·7 × (father’s education + mother’s education) + 0·4 × (father’s occupation + mother’s education), then the level of socio-economic status was classified as low (<25th percentile) and average/high (≥25th percentile).
School-level variables
School-level variables were collected with an interviewer-administered school questionnaire, which was initially derived from policies, provisions and guidelines on supporting healthy school environment at national-level and district-level. Questions and themes were developed based on previous studies, that is, the PLAY-Ontario study(Reference Leatherdale, Manske and Faulkner14), the Environmental Determinants in Young people (SPEEDY) study(Reference Harrison, Bentham and Jones29) and the Health Behavior in School-aged Children (HBSC) study(Reference Galan, Boix and Medrano24). Prior to data collection, we conducted interviews with experts on school health, administrators at local school heath agencies and relevant school staffs to identify the potential key variables according to their experiences regarding obesity prevention strategies. Modifications were also made to the wording and formatting of the questions afterwards.
The final school-level questionnaire involved thirty indicators of five obesity-related themes: (1) School personnel allocation (four indicators): the number, and educational background of school health professionals; position of the responsible person in charge of obesity prevention and control; the management team of obesity prevention. (2) School management policies (seven indicators): written school guidelines; annual work plan; meetings on students’ obesity prevention; availability of students’ health records; monitoring students’ nutrition status; partnership of school sport and health department; participation of class administrators. (3) School health education (nine indicators): health education (e.g. having professional teachers and curriculum schedule), obesity-related lectures, courses and activities for students; obesity-related educational opportunities, feedback of the annual students physical examination, suggestions for overweight/obese students, and school obesity prevention report for parents; obesity-related educational opportunities for teachers. (4) School PA reported by the head of physical education teacher (seven indicators): duration of PA (e.g. compulsory physical education classes and other physical activities) in regular school time; alternative PA in extreme weather conditions; PA homework in holidays; frequency of intramural sports teams and clubs; school sports meeting; promoting overweight/obesity students’ PA involvement; playground equipment like climbing structure and swings, etc. (5) School food environment (three indicators): type of school lunch providers (school canteens or food companies); offering the recipes with food composition to parents; control the overeating of overweight/obese students at school lunch. Each indicator was classified into two categories (Yes or No).
At each school, two trained investigators completed a school-level questionnaire by conducting face-to-face interview with the school health professional, who was responsible for obesity prevention and control. In order to improve the reproducibility of the data, a main investigator took part in data collection of all schools. In order to ensure the reliability and accuracy of the information, plausible answers were asked by investigators to provide more details, or to confirm via relevant school staffs (e.g. school administrators, physical education teachers and health education teachers). Reviewing available documents and field observation were also conducted if required.
Statistical analyses
To take account of the hierarchical data structure (students nested within schools), generalised linear mixed models were used to estimate which school-level characteristics were associated with students’ obesity while controlling for potential individual-level variables. Consistent with previous studies, our statistical analyses used three-step modelling procedures(Reference Haug, Torsheim and Samdal12,Reference Leatherdale17) .
First, the null model was established to determine whether the difference in students’ obesity among schools was random or fixed, and the school-level variance term was used to calculate the intra-class correlation for obesity among schools.
Second, a series of univariate multilevel analyses were performed to identify any individual- and school-level variables potentially associated with obesity. In these exploratory models, sex, age and school location (rural or urban) were adjusted as fixed terms with school as a random effect. Each individual- and school-level variable was included one by one, only variables that were statistically significant at P < 0·20 were retained(Reference Hobin, Leatherdale and Manske13). After these initial screening stages, a ‘school-based obesity prevention index’ was calculated as the additive score of retained school-level variables (Yes = 1 point, No = 0 point), with the higher value reflecting the higher quality of school obesity prevention and control. The use of additive score was also found in previous HBSC study(Reference Button, Trites and Janssen11) and COSI study(Reference Wijnhoven, van Raaij and Sjoberg30). Based on the median number, the school-based obesity prevention index was further converted into a dichotomous variable for the following analysis.
Finally, a multivariate model was performed to simultaneously examine how the identified individual-level variables and the school-based obesity prevention index were associated with students’ obesity, with adjusting same confounders in the second step. Since cross-level interactions were suggested in the previous study(Reference Leatherdale, Pouliou and Church18), we additionally examined the interaction terms between school- and individual-level variables in the same model. Statistical tests were considered to be significant if two-sided P < 0·05. All statistical calculations were performed with SAS software (V9.3; SAS Institute Inc.).
Results
General characteristics of participants
There were 1107 (50·3 %) boys and 1094 (49·7 %) girls included in our final analysis. The average age of participants was (10·00 ± 0·41) years. The average BMI of participants was 18·20 ± 3·66 kg/m2, with 17·2 % of them classified as obese.
Potential individual- and school-level variables associated with childhood obesity
The associations of individual-level variables with childhood obesity at P < 0·20 are showed in Table 1. Findings from univariate analyses indicated that student variables including liking sports, screen time, homework time, perceived eating speed, as well as family variables including parental weight status were associated with obesity. Nevertheless, the variables of moderate-to-vigorous physical activity, dietary pattern and family socio-economic status did not show significant effects at P < 0·20 and were not included in final analyses (online Supplemental Table S1).
Table 1 The individual-level variables associated with childhood obesity (P < 0·20)*
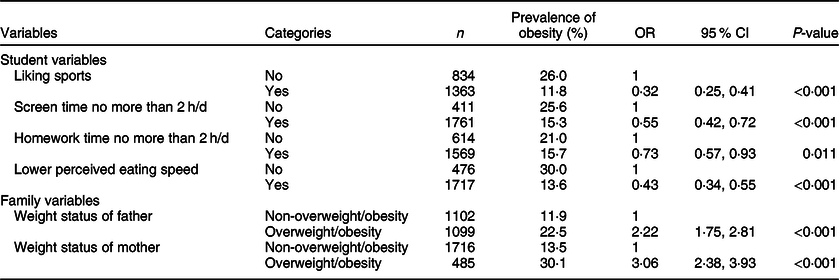
* Adjusted for sex, age and school location (rural or urban) with school as a random effect.
The seven school-level variables which were associated with students’ obesity at P < 0·20 are showed in Table 2, including one variable from school personnel allocation, two variables from school management policies, two variables from school health education and two variables from school PA. Moreover, one variable was statistically associated with obesity, suggested that students attending a school that reached the national standard of the number of health professionals (at least one health professional every 600 students) were less likely to be obese compared with the others (OR 0·68, 95 % CI 0·51, 0·91, P = 0·010). The full list of school-level variables which were analysed is provided in online Supplemental Table S2. We further calculated the school-based obesity prevention index for each school (range from 0 to 7 points), which was the cumulative score from these seven school-level variables. According to the median number of 5, eleven schools with 642 students were classified as higher index value and twenty-six schools with 1559 students were classified as lower index value.
Table 2 The school-level variables associated with childhood obesity (P < 0·20)*
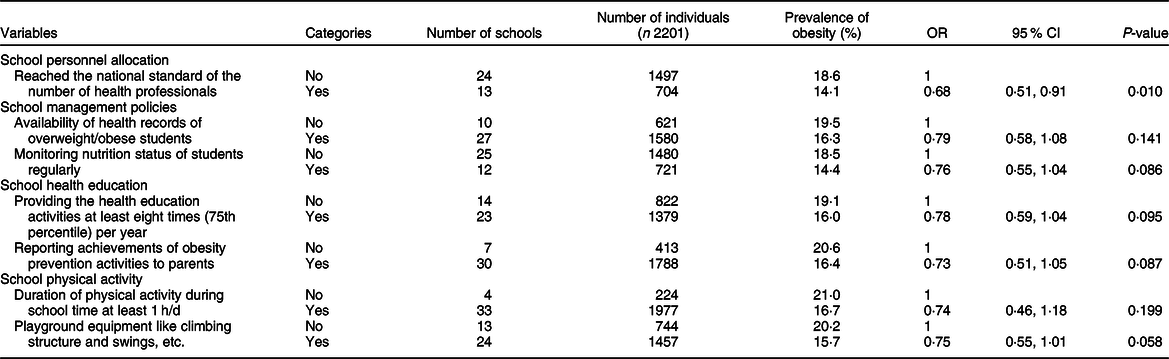
* Adjusted for sex, age and school location (rural or urban) with school as a random effect.
The associations of individual-level and school-level variables with childhood obesity
The adjusted OR in the final multivariate model are presented in Table 3. In individual-level, students with screen time ≤2 h/d showed the lower prevalence of obese compared with students with screen time >2 h/d (OR 0·65, 95 % CI 0·48, 0·86, P = 0·003). It was also lower among students liking sports and having perceived lower eating speed compared with those counterparts, with an OR of 0·34 (95 % CI 0·26, 0·43, P < 0·001) and 0·45 (95 % CI 0·35, 0·59, P < 0·001), respectively. The increased risk was found for the students of paternal overweight/obesity (OR 2·09; 95 % CI 1·63, 2·69, P < 0·001) and maternal overweight/obesity (OR 2·77; 95 % CI 2·12, 3·61, P < 0·001). In school level, the results suggested that the school-based obesity prevention index was associated with students’ obesity. If a student attended a school which had the index value above 5, he/she was less likely to be obese than a student attending a school that had the index value ≤5 (OR 0·56; 95 % CI 0·40, 0·79, P = 0·001). No statistically significant interactions were found between the individual-level variables and school-based obesity prevention index on obesity, suggesting that the association between school-based obesity prevention index and students’ obesity was not moderated by individual-level variables in the present study.
Table 3 The adjusted odds ratios for the individual- and school-level variables associated with childhood obesity*
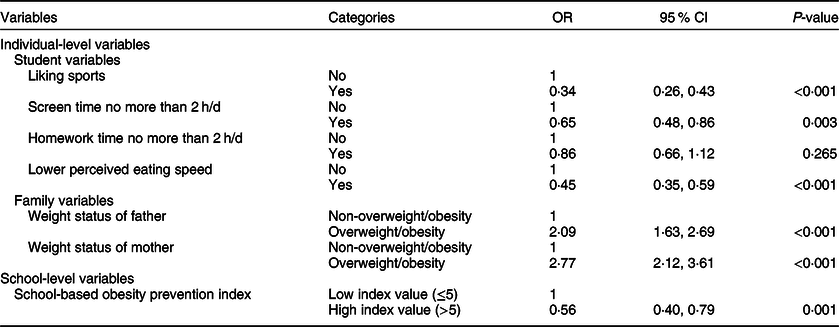
* Adjusted for sex, age and school location (rural or urban) with school as a random effect.
Discussion
We comprehensively investigated a total of thirty school-level variables involving school personnel, management, health education, PA and food environments. We ultimately identified seven variables potentially related to students’ obesity and further established the school-based obesity prevention index. Our results suggested that the index was associated with students’ obesity after controlling for individual-level variables. Contrary to previous studies which reported only few school-level variables having statistically significant association with obesity, our study not only examined individual effect size of each school-level variable but also created the school-based obesity prevention index to detect accumulative effect. From a public perspective, it is promising to develop effective obesity interventions based on empirical initiatives implemented by primary schools in China.
With respect to the student variables we took into consideration, we found that liking sports was associated with lower odds of being obese. Previous findings also supported that children’s activity preferences may have impact on their PA behaviours thereby influence their weight status, suggesting that even if young people with access to environmental resource may not use them(Reference Haug, Torsheim and Samdal12). Besides, we observed a positive association between screen time and obesity, whereas the same association has not been observed in other SB time such as homework time. A recent review suggested that screen time and predominantly TV viewing were associated with unhealthy dietary behaviours in children(Reference Pearson and Biddle31). Meanwhile, longer screen time often implies shorter homework time and PA time due to the daily waking time limit(Reference Spear, Barlow and Ervin4,Reference Chastin, Palarea-Albaladejo and Dontje32) . These could be the explanations why the association between screen time and obesity was stronger than other SB time in our results. Finally, a positive association has been seen regarding perceived eating speed and obesity. Ochiai et al.(Reference Ochiai, Shirasawa and Ohtsu33) also found fast eating speed increased the risk of being overweight compared with medium eating speed. Due to a reduced awareness of satiety, quickly eating may lead to higher energy intake, eating slowly could also be effective for preventing overeating and obesity in children(Reference Otsuka, Tamakoshi and Yatsuya34). Regarding family variables, our study showed that childhood obesity had strong association with parental weight status, which could be explained by both genetics and environmental interactions between children and parental weight(Reference Bahreynian, Qorbani and Khaniabadi35,Reference Lazzeri, Pammolli and Pilato36) . For example, previous studies found that parental dietary pattern was associated with children’s dietary pattern(Reference Hebestreit, Intemann and Siani37), and family factors can explain 61 % variance of healthy food intake(Reference Bogl, Silventoinen and Hebestreit38). This result supported the idea that school-based obesity intervention with home involvement might be more effective.
It is of particular note that most of the variables in univariate analysis were not statistically significant under significance level of P < 0·05 when we explored the associations between school-level characteristics and obesity. The paucity of statistically significant associations has also been seen in previous studies(Reference Leatherdale17,Reference Harrison, Bentham and Jones29) . As numerous school-based obesity intervention studies suggested, obesity prevention is a complex task which needs comprehensive programmes involving PA and nutrition(Reference Feng, Wei and Lin39). Single-component strategy such as educational interventions may have limited efficiency in prevention of childhood obesity(Reference Sbruzzi, Eibel and Barbiero40). In light of the above, our study advances the method to obtain more insights into the impact of school-level characteristics. We observed the cumulative effect of seven school-level factors, indicating that the school-based obesity prevention index above 5 can make a substantial contribution to obesity prevention and to some extents make schools flexible to choose the strategies which are suitable for their own contexts.
Of the school-level factors examined in univariate analysis, the number of health professionals was the only one that had a significantly negative association with the risk of students’ obesity. The health professionals play an important role in students’ health since they are not only in charge of the disease control but also undertaking health education, supervision and promotion in Chinese primary schools. According to School Health Regulations from Chinese government, every 600 students need a health professional in primary schools, and if the number of students is <600, at least one health professional should be allocated. However, the situation of insufficient personnel is still common even among schools in Beijing, suggesting that it is urgent for stakeholders to improve the quantity of health professionals in primary schools.
In addition to the importance of health professionals in schools, we also found monitoring the nutrition status regularly and having the health records of overweight/obese students had beneficial effects on obesity prevention, which were also undertaken by existing intervention studies as feedback and motivation strategies(Reference Feng, Wei and Lin39). Moreover, our results proved that providing health education activities frequently was one of the predictors, and parental involvement may accentuate the impact in alignment with the evidence of system reviews(Reference Katz, O’Connell and Njike41,Reference Oosterhoff, Joore and Ferreira42) . Furthermore, schools with longer duration of PA may decrease the likelihood of students being obesity. Previous study found that school hours almost contributed to half of total moderate-to-vigorous physical activity in students, supporting that enough PA during school hours may facilitate childhood obesity prevention(Reference Sprengeler, Wirsik and Hebestreit43). At last, our results also indicated that students’ obesity may benefit from better playground equipment. This may be explained by increased PA level when more facilities are available(Reference Galan, Boix and Medrano24,Reference Nichol, Pickett and Janssen44) . Apart from those factors, we did not observe any variable from food environment under the statistical significance at P < 0·20, thereby no variables from this theme were included in the school-based obesity prevention index. However, Li et al.(Reference Li, Xue and Wen20) found the presence of cafeterias was associated with increased overweight/obesity risk in rural middle school students, and another Chinese study also suggested that having food regulations in school cafeterias and campus food stores were related to lower intake of energy dense foods as well as the prevalence of overweight/obesity in those primary and middle schools(Reference Jia, Li and Xue19). The availability of healthy and unhealthy food was also associated with students’ nutrition status(Reference Masse, de Niet-Fitzgerald and Watts16,Reference Fox, Dodd and Wilson45,Reference Terry-McElrath, O’Malley and Johnston46) . Since we only investigated three indicators about school food environment, further investigative work is required to provide more evidence how the foods offered by schools contribute to students’ obesity.
There are some limitations in this study. First, it is a cross-sectional study which does not allow us to infer the causal relationship. However, the evidence of associations is still meaningful for further experimental studies. Moreover, our data were collected in a sample from two districts of Beijing, and only students from grade 4 were included, so the results may not be generalised to the entire population. However, according to the experience of our previous studies, the students at grade 4 can well understand and complete the questionnaire and they have less study pressure influencing their daily behaviours compared with senior students; hence it is a representative group for most students in primary schools. Besides, previous studies suggested that neighbourhood environments surrounding schools are also related to students’ obesity(Reference Jia, Xue and Cheng47). However, this information is unavailable in the present study, and future study should also take school neighbourhood environmental factors into consideration. Finally, our data were based on a questionnaire. But, the school-level questionnaire was completed by trained investigators so that the reliability of data can be ensured. The school questionnaire still needs further validation.
Conclusions
This study reveals that the specific school-level characteristics had cumulative effects on obesity, and several individual-level characteristics were also related to obesity among Chinese primary school children. From a population-level perspective, the prevalence of obesity was lower in schools with the higher school-based obesity prevention index compared with that in schools with the lower index. Further school-based obesity intervention should consider these aspects in particular and evaluate whether both improving the school- and individual-level characteristics would be effective in preventing childhood obesity.
Acknowledgements
Acknowledgements: We thank all the school staffs, students and parents who took part in the study. We are grateful for the support from schools, school health centres and all the members in our research team. Financial support: This study was funded by grants from National Key R&D Program of China (2016YFC1300204), the State General Administration of Sport of China (2017B025) and Chinese Medical Board (11-064). All the funders had no role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: The authors’ contributions were as follows: L.C. and H.J.W. designed the study; L.C., D.W. and Y.C. collected data; L.C. and Q.L. conducted data cleaning and analysis; L.C. wrote the manuscript; H.J.W., A.H. and Y.S. revised and improved drafts of the manuscript. All authors have been read and approved the final manuscript. Ethics of human subject participation: This study was conducted according to the Declaration of Helsinki, and all procedures involving research study participants were approved by the Ethics Committee of Peking University Health Science Center. Written informed consent was obtained from the parents of all participants.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980019004592.







