Introduction
Current nosology classifies the observed manifestations of psychosis into two main categories of non-affective (e.g. schizophrenia, schizoaffective disorder) and affective psychosis (e.g. bipolar and major depressive disorders with psychotic features) (World Health Organization, 1992; American Psychiatric Association, 2013). However, the scientific accessibility of discrete ‘natural disease entities’ in psychiatry has been questioned since Kraepelin's original distinction between dementia praecox and manic-depressive psychosis (Kraepelin, Reference Kraepelin1899; Murray et al., Reference Murray, Sham, Van Os, Zanelli, Cannon and McDonald2004; Craddock and Owen, Reference Craddock and Owen2005; Hoff, Reference Hoff, Kendler and Parnas2017). On this basis, it has been proposed, and is now widely accepted, that the categorical classification system alone is too reductionist to explain the complexity of psychotic phenomena (Van Os et al., Reference Van Os, Gilvarry, Bale, Van Horn, Tattan, White and Murray1999; Linscott and van Os, Reference Linscott and van Os2010). Various evidence-based perspectives might support a scheme incorporating symptom dimensions in psychotic disorders, as a possible approach to address the following limitations of categorical distinctions.
First, the dichotomous model of non-affective and affective psychosis does not fit the cases presenting with both prominent mood and psychotic symptoms. This is testified by the notion of a third category of schizoaffective disorder (Kasanin, Reference Kasanin1933), which nevertheless implies further nosological challenges (Abrams et al., Reference Abrams, Rojas and Arciniegas2008).
In addition, if criteria-based classification systems could identify genuine disorders within the psychosis spectrum, the diagnostic overlap would be relevant to only a few patients. On the contrary, there is a large comorbidity index between schizophrenia, schizoaffective, bipolar, and major depressive disorders (Laursen et al., Reference Laursen, Agerbo and Pedersen2009; Upthegrove et al., Reference Upthegrove, Marwaha and Birchwood2017). Similarly, the 10-year outcomes of the Aetiology and Ethnicity in Schizophrenia and Other Psychoses (ÆSOP-10) study showed that diagnoses within psychosis other than schizophrenia at baseline tend to be unstable over time (Heslin et al., Reference Heslin, Lomas, Lappin, Donoghue, Reininghaus, Onyejiaka, Croudace, Jones, Murray, Fearon, Dazzan, Morgan and Doody2015).
Also, the dichotomous model is neither consistent with family studies showing familial co-aggregation of non-affective and affective psychosis (Cardno et al., Reference Cardno, Rijsdijk, Sham, Murray and McGuffin2002; Lichtenstein et al., Reference Lichtenstein, Yip, Björk, Pawitan, Cannon, Sullivan and Hultman2009; Chou et al., Reference Chou, Kuo, Huang, Grainge, Valdes, See, Yu, Luo, Huang, Tseng, Zhang and Doherty2017) nor with the accumulated evidence from genome-wide association studies that genetic risk is in part shared among schizophrenia, bipolar disorder, and major depressive disorder (International Schizophrenia Consortium et al., Reference Purcell, Wray, Stone, Visscher, O'Donovan, Sullivan and Sklar2009; Demjaha et al., Reference Demjaha, MacCabe and Murray2011; Cardno and Owen, Reference Cardno and Owen2014; O'Donovan and Owen, Reference O'Donovan and Owen2016; Power et al., Reference Power, Tansey, Buttenschon, Cohen-Woods, Bigdeli, Hall, Kutalik, Lee, Ripke, Steinberg, Teumer, Viktorin, Wray, Arolt, Baune, Boomsma, Borglum, Byrne, Castelao, Craddock, Craig, Dannlowski, Deary, Degenhardt, Forstner, Gordon, Grabe, Grove, Hamilton, Hayward, Heath, Hocking, Homuth, Hottenga, Kloiber, Krogh, Landen, Lang, Levinson, Lichtenstein, Lucae, MacIntyre, Madden, Magnusson, Martin, McIntosh, Middeldorp, Milaneschi, Montgomery, Mors, Muller-Myhsok, Nyholt, Oskarsson, Owen, Padmanabhan, Penninx, Pergadia, Porteous, Potash, Preisig, Rivera, Shi, Shyn, Sigurdsson, Smit, Smith, Stefansson, Stefansson, Strohmaier, Sullivan, Thomson, Thorgeirsson, Van der Auwera, Weissman, Breen and Lewis2017).
Last, several studies show the efficacy of agents which impact on dopamine signalling in the treatment of both non-affective and affective symptoms. For example, antipsychotics antagonise D2-receptor functioning and are used in bipolar disorder and schizophrenia (Post, Reference Post1999; Taylor et al., Reference Taylor, Paton and Kapur2015), and clozapine is prescribed for both treatment-resistant bipolar disorder and schizophrenia (Li et al., Reference Li, Tang, Wang and de Leon2015; Goodwin et al., Reference Goodwin, Haddad, Ferrier, Aronson, Barnes, Cipriani, Coghill, Fazel, Geddes, Grunze, Holmes, Howes, Hudson, Hunt, Jones, Macmillan, McAllister-Williams, Miklowitz, Morriss, Munafo, Paton, Saharkian, Saunders, Sinclair, Taylor, Vieta and Young2016; Howes et al., Reference Howes, McCutcheon, Agid, de Bartolomeis, van Beveren, Birnbaum, Bloomfield, Bressan, Buchanan and Carpenter2016). These findings suggest that dopamine dysregulation may contribute to both positive and manic symptoms, as supported by recent positron emission tomographic findings (Jauhar et al., Reference Jauhar, Nour, Veronese, Rogdaki, Bonoldi, Azis, Turkheimer, McGuire, Young and Howes2017).
Taken together, the above evidence challenges the binary categorization of non-affective and affective psychosis, enhancing research into non-categorical approaches. Pioneering studies using factor analysis examined associations among non-affective symptoms in schizophrenia and showed that these symptoms segregated in three groups (Liddle, Reference Liddle1987); however, these groups could not accommodate the whole symptom diversity in schizophrenia (Kay and Sevy, Reference Kay and Sevy1990). Thus, psychopathology models including also depressive and manic factors were proposed and replicated in schizophrenia (Lindenmayer et al., Reference Lindenmayer, Bernstein-Hyman and Grochowski1994; Salokangas, Reference Salokangas1997; Wickham et al., Reference Wickham, Walsh, Asherson, Taylor, Sigmundson, Gill, Owen, McGuffin, Murray and Sham2001; Wallwork et al., Reference Wallwork, Fortgang, Hashimoto, Weinberger and Dickinson2012). This type of structure was likewise confirmed in psychotic disorders (Salokangas, Reference Salokangas2003; Dikeos et al., Reference Dikeos, Wickham, McDonald, Walshe, Sigmundsson, Bramon, Grech, Toulopoulou, Murray and Sham2006; Demjaha et al., Reference Demjaha, Morgan, Morgan, Landau, Dean, Reichenberg, Sham, Fearon, Hutchinson, Jones, Murray and Dazzan2009), and in a sample of bipolar patients (Lindenmayer et al., Reference Lindenmayer, Bossie, Kujawa, Zhu and Canuso2008). Hence, its validity across the spectrum of non-affective and affective psychosis has been consistently supported.
Recent findings suggest a more fundamental general, transdiagnostic dimension encompassing non-affective and affective symptoms, in addition to five specific symptom dimensions (Reininghaus et al., Reference Reininghaus, Priebe and Bentall2013; Reininghaus et al., Reference Reininghaus, Bohnke, Hosang, Farmer, Burns, McGuffin and Bentall2016; Shevlin et al., Reference Shevlin, McElroy, Bentall, Reininghaus and Murphy2017). This conceptualization statistically reflects a bifactor model, with one general factor representing shared variance among all symptoms, and a set of specific factors where the remainder of the variance is shared among subsets of symptoms (Reise et al., Reference Reise, Morizot and Hays2007). This is the first study set to investigate, in an incidence sample of First Episode Psychosis (FEP) patients: (1) whether the general psychosis dimension holds across diagnostic categories of non-affective psychosis (i.e. schizophrenia, schizoaffective disorder) and affective psychosis (i.e. bipolar and major depressive disorder with psychotic features); (2) whether formation of specific symptom dimensions is justified in addition to a general psychosis dimension; and (3) the association of demographic characteristics (i.e. age, gender, ethnicity), social context (i.e. urbanicity), and clinical factors (i.e. diagnosis) with general and specific psychosis dimensions.
The hypotheses underlying the third aim, based on the existing literature, were:
(a) Positive symptoms would be more common in ethnic minority groups and in people living in more densely populated environments (van Os et al., Reference van Os, Hanssen, Bijl and Vollebergh2001, Janssen et al., Reference Janssen, Hanssen, Bak, Bijl, de Graaf, Vollebergh, McKenzie and van Os2003).
(b) Negative symptoms would be associated with indices suggestive of neurodevelopment impairment in psychosis (Limosin, Reference Limosin2014; Patel et al., Reference Patel, Jayatilleke, Broadbent, Chang, Foskett, Gorrell, Hayes, Jackson, Johnston, Shetty, Roberts, McGuire and Stewart2015), such as being a man or having an early age at onset.
Methods
Sample design and procedures
Individuals suffering from their FEP were recruited between 2010 and 2015 as part of the large EUropean network of national schizophrenia networks studying Gene–Environment Interactions (EU-GEI) study (http://www.eu-gei.eu). Specifically, FEP individuals were recruited as part of the ‘Functional Enviromics’ work package, which consisted of an incidence and a case-sibling-control study conducted across six countries with the aim to investigate clinical, genetic, and environmental interaction in the development of psychotic disorders.
The study had 17 catchment areas, including urban and less urban populations: Southeast London, Cambridgeshire and Peterborough (England); central Amsterdam, Gouda and Voorhout (the Netherlands); part of the Veneto region, Bologna municipality, city of Palermo (Italy); 20th arrondissement of Paris, Val-de-Marne, Puy-de-Dôme (France); Madrid (Vallecas), Barcelona, Valencia, Oviedo, Santiago, Cuenca (Spain); and Ribeirão Preto (Brazil).
Participants
We screened all subjects who were referred to mental healthcare services with a suspicion of psychosis. The ascertainment period of cases ranged from 12 months in London to 48 months in Val-de-Marne and Bologna, with a median of 25 months. In each site, a psychiatrist experienced in epidemiology research oversaw the local team, which was centrally trained to minimize non-differential recruitment bias in the different healthcare systems. Written consent was obtained from the subjects who agreed to take part of the case-sibling-control study. For incidence-only cases, local research ethics committees approved the extraction of demographics and clinical information from patient records. More detailed information is available on the EU-GEI core paper on the incidence rates of schizophrenia and other psychotic disorders (Jongsma et al., Reference Jongsma, Gayer-Anderson, Lasalvia, Quattrone, Mule, Szoke, Selten, Turner, Arango, Tarricone, Berardi, Tortelli, Llorca, de Haan, Bobes, Bernardo, Sanjuan, Santos, Arrojo, Del-Ben, Menezes, Velthorst, Murray, Rutten, Jones, van Os, Morgan and Kirkbride2018).
Patients were included in the current study if they met the following criteria during the recruitment period: (a) aged between 18 and 64 years; (b) presentation with a clinical diagnosis for an untreated FEP, even if longstanding [International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes F20-F33]; (c) resident within the catchment area at FEP. Exclusion criteria were: (a) previous contact with psychiatric services for psychosis; (b) psychotic symptoms with any evidence of organic causation; and (c) transient psychotic symptoms resulting from acute intoxication (ICD-10: F1x.5).
Measures
Data on age, gender, and ethnicity was collected using a modified version of the Medical Research Council Sociodemographic Schedule (Mallett, Reference Mallett1997). Ethnicity was defined as self-reported. Country of heritage or birth was used as a proxy for ethnicity in people of a North African background. The OPerational CRITeria (OPCRIT) system (McGuffin et al., Reference McGuffin, Farmer and Harvey1991; Williams et al., Reference Williams, Farmer, Ackenheil, Kaufmann and McGuffin1996) was used by centrally trained investigators, whose reliability was assessed throughout the study (κ = 0.7). The OPCRIT system allows to: (1) assess the pre-morbid history and current mental state; and (2) establish the diagnosis of psychotic disorders based on algorithms for several diagnostic classification systems. It consists of a checklist which can be filled using different sources, e.g. case records or clinical interviews. Fifty-nine items relate to the mental state examination. We used diagnoses based on Research Diagnostic Criteria (RDC) (Spitzer et al., Reference Spitzer, Endicott and Robins1978), since this classification system provides a better representation of schizoaffective disorder, which is a common presentation in clinical practice. OPCRIT RDC-based diagnoses have a good-to-excellent agreement with best-estimate consensus diagnostic procedures (Craddock et al., Reference Craddock, Asherson, Owen, Williams, McGuffin and Farmer1996). In each catchment area, population density was computed as a number of inhabitants per square kilometre, based on official population estimates.
Statistical analysis
Psychopathology items were dichotomized as 0 ‘absent’ or 1 ‘present’. In order to ensure sufficient covariance coverage for item response modelling, we used the items with a valid frequency of ‘present’ ⩾10% in our sample, which included individuals with ⩽20 missing values in the psychopathology rating. OPCRIT data used in the analysis contained missing values, which we assumed to be missing at random, allowing for the maximum likelihood estimator to provide unbiased estimates. We performed multidimensional item response modelling in Mplus, version 7.4 (Muthén and Muthén, Reference Muthén and Muthén2012) to estimate unidimensional, multidimensional, bifactor, and second-order models of psychosis.
Extending previous analyses of OPCRIT data in individuals with enduring psychosis (Reininghaus et al., Reference Reininghaus, Bohnke, Hosang, Farmer, Burns, McGuffin and Bentall2016), we estimated five alternative item-response models (online Supplementary Fig. S1): (a) a unidimensional model with one unique general factor (model A), which is consistent with the pre-Kraepelinian unitary concept of psychosis (Berrios and Beer, Reference Berrios and Beer1994); (b) a multidimensional model with five uncorrelated specific factors of positive, negative, disorganization, manic, and depressive symptoms (model B); (c) a multidimensional model with five correlated specific factors (model C), which, together with model B, is consistent with the pentagonal psychosis model (van Os and Kapur, Reference van Os and Kapur2009); (d) a bifactor model with one general latent factor along with five uncorrelated specific factors (model D) (Reininghaus et al., Reference Reininghaus, Bohnke, Hosang, Farmer, Burns, McGuffin and Bentall2016); and (e) a hierarchical model with five first-order specific factors and one general second-order factor (model E), which, as model D, is consistent with the notion of a transdiagnotic spectrum of non-affective and affective psychosis (Craddock and Owen, Reference Craddock and Owen2005; Reininghaus et al., Reference Reininghaus, Bohnke, Hosang, Farmer, Burns, McGuffin and Bentall2016). Some previous OPCRIT exploratory analysis showed a combined negative/disorganization dimension (Serretti et al., Reference Serretti, Rietschel, Lattuada, Krauss, Schulze, Muller, Maier and Smeraldi2001; Fanous et al., Reference Fanous, van den Oord, Riley, Aggen, Neale, O'Neill, Walsh and Kendler2005). We did not have a strong theoretical rationale for testing such a structure in a confirmatory analysis. By contrast, we considered specific negative symptoms as a clinically observable marker of neurodevelopmental impairment in psychosis (Limosin, Reference Limosin2014).
The five models were compared using Log-Likelihood (LL), Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), and Sample-size Adjusted BIC (SABIC) as model fit statistics. For the model showing the best fit, we calculated reliability and strength indices, such as McDonald's omega (ω), omega hierarchical (ω H), and index H. Coefficient ω is an estimate of the proportion of common variance accounted by general and specific symptom dimensions. Coefficient ω H is an estimate of the proportion of reliable variance accounted by the general dimension, treating variability in scores due to specific dimensions as measurement error (Rodriguez et al., Reference Rodriguez, Reise and Haviland2016b). Ωh formula can be extended to each specific factor, i.e. treating variability in scores due to the general factor as a measurement error, to compute omega hierarchical for subscales. Based on omega and omega hierarchical coefficients, which can vary from 0 to 1, we computed the ratios of ω/ω H, namely the relative omega, as the amount of reliable variance explained in the observed scores attributable to (1) the general factor independently from the specific symptom dimensions, and (2) each specific symptom dimension independently from the general factor. To estimate the extent to which symptom dimensions were represented by their own set of OPCRIT items and their replicability across studies, we computed the construct reliability index H (Hancock and Mueller, Reference Hancock, Mueller, Cudek, Du Toit and Sorbom2001). The index H ranges from 0 to 1, with values closer to 1 indicating better reliability and replicability (Rodriguez et al., Reference Rodriguez, Reise and Haviland2016a). Quantitative scores for all symptom dimensions were calculated using the ‘FSCORES’ function in Mplus.
Further, we examined the diagnostic classification accuracy based on general and specific symptom dimension scores using multinomial receiver operating characteristic (ROC) analysis in STATA 14 (StataCorp, Reference StataCorp2015). In addition, we performed a sensitivity analysis, examining subjects with item ratings based on face-to-face interview and based on clinical records separately.
We used multiple linear regression to examine the association between factor scores of general and/or specific psychosis dimensions as the outcome variable and demographic variables, including gender, age-at-first-contact with psychiatric services, ethnicity, and diagnosis as covariates. Country and assessment method were treated as a priori confounders.
To examine the individual-level effect of urbanicity on symptom dimension scores, standardized population density values were used as a continuous independent variable, while controlling the analysis for gender, age-at-first-contact, ethnicity, diagnosis, and assessment method. Sensitivity analysis included post-hoc multiple regressions within each country, where population density was dichotomized at its median as a dummy variable for urbanicity.
Results
Sample characteristics
We identified 2774 treated incidence cases of psychosis (Jongsma et al., Reference Jongsma, Gayer-Anderson, Lasalvia, Quattrone, Mule, Szoke, Selten, Turner, Arango, Tarricone, Berardi, Tortelli, Llorca, de Haan, Bobes, Bernardo, Sanjuan, Santos, Arrojo, Del-Ben, Menezes, Velthorst, Murray, Rutten, Jones, van Os, Morgan and Kirkbride2018), of whom 2182 had (complete or missing at random) OPCRIT data available for analysis under the provision of local research ethics committees (Table 1). OPCRIT item ratings were completed based on face-to-face assessment for 51% (n = 1112) and based on clinical records for 49% (n = 1070) of the sample. The sample prevalence of psychotic symptoms is presented in Supplementary Table S1.
Table 1. Demographic and clinical characteristics of the sample included in the factor analysis

a Psychopathology assessment methods included face-to-face interview or review of clinical notes.
b Study countries were England, the Netherlands, France, Spain, Italy, and Brazil.
c 29 missing values excluded from tabulation and age analysis.
d Other and missing self-reported groups excluded from ethnicity analysis.
e Schizophrenia spectrum encompassed Broad Schizophrenia (N = 194) and Narrow Schizophrenia (N = 648); Schizoaffective disorder encompassed Schizoaffective/manic (N = 112); Schizoaffective/depressive (N = 566); Schizoaffective/bipolar (N = 86).
Fifty-seven per cent of FEP were men. Subjects were mostly people of a White ethnicity. Other main ethnic groups included Black African and Black Caribbean, North African, Mixed, and Asian. Mean age-at-first-contact with psychiatric services was 32.1 years; this was lower in men (M = 30.1) compared with women (M = 34.7; t = −9.6, p < 0.001). Age-at-first-contact differed across ethnic groups, with individuals of Black ethnicity (M = 29) being younger than individuals of White ethnicity (M = 32.7; F = 7.72, p < 0.001). The most common RDC-based diagnosis was broad or narrow schizophrenia (38.6%), followed by schizoaffective disorders (35%), unspecified non-organic psychotic disorder (16.3%), bipolar disorder (5.9%), and psychotic depression (4.2%).
Symptom dimensions in the EU-GEI sample
The bifactor model was the best fit for the OPCRIT symptom data compared with all other models, as consistently indicated by each of the model fit statistics (Table 2), and explained 54% of the total variance.
Table 2. Model fit statistics of unidimensional, multidimensional, bi-factor, and second-order models
LL, log-likelihood; AIC, Akaike Information Criterion; BIC, Bayesian Information Criterion; SABIC Sample-size Adjusted Bayesian Information Criterion.
a A difference of 10 in AIC, BIC and SABIC is considered important. Lower values indicate a statistically better model fit.
Figure 1 shows that, within the bifactor model, general and specific dimensions accounted for 93% of the common variance. Overall, statistical indices derived from the bifactor model suggest that its explained variance was due to individual differences in both general and specific symptom dimensions, which therefore might complement each other in reflecting the psychopathological structure at FEP. This is illustrated by the relative omega coefficients, which, for example, showed that 47% of the reliable variance was due to the general factor when partitioning out the variability in scores due to the specific factors (Fig. 1). High H values were consistently observed for all latent factors, indicating that they were well defined, and that the bifactor model had high reliability and replicability (Fig. 1). Sensitivity analysis showed that the bifactor model was the best fit for the OPCRIT data in both the assessment methods (online Supplementary Tables S2.1 and S2.2).
Fig. 1. Bifactor model. (□) Observed variables (No. of OPCRIT items); (○) Unobserved variables (latent factors); (→) standardized item loading estimation onto latent factors; G, general psychosis factor; specific symptom factors: DEP, depression; MAN, mania; DIS, disorganization; NEG, negative; POS, positive. Reliability and strength estimates: H = construct reliability index; ω = McDonald omega; ω H = hierarchical omega; ω/ω H = Relative omega. Explanatory note: McDonald's ω is an estimate of the proportion of the common variance accounted by general and specific symptom dimensions. Relative omega (ω/ω h) is the amount of reliable variance explained in the observed scores attributable to (1) the general factor independently from the specific symptom dimensions, and (2) each specific symptom dimension independently from the general factor. H is an index of the quality of the measurement model based on the set of OPCRIT items for each symptom dimension. Index H can range from 0 to 1, with values closer to 1 indicating a better construct reliability and replicability across studies.
Symptom dimensions and item factor loadings
Table 3 shows standardized factor loadings for the bifactor model. On the general dimension, a positive factor loading was observed for all OPCRIT items with statistically significant loadings. In addition, the magnitude of factor loadings of items on the general dimension was small, except for some manic/delusional items for which loadings of moderate magnitude were observed. On the specific dimensions, most of the items showed moderate to strong positive loadings. Finally, latent factor scores were strongly and positively associated with simplified weighted OPCRIT sum scores for use in clinical practice (online Supplementary Table S3).
Table 3. Standardized factor loadings in the bifactor model
General, general psychosis factor; specific symptom dimensions: DEP, depression; MAN, mania; DIS, disorganisation; NEG, negative; POS, positive. Only loadings ⩾0.2 for the general factor are shown for simplicity. Significance: *** = p < 0.001; ** = p < 0.01.
Symptom dimensions and categorical diagnoses
Findings from regression analyses are shown in Table 4 and predicted symptom dimension scores for each RDC-based diagnostic category are reported in Fig. 2. Compared with bipolar disorder, factor scores for the positive dimension were moderately higher in schizophrenia and schizoaffective disorder; factor scores for the negative dimension were moderately higher in schizophrenia, schizoaffective and psychotic depression; and factor scores for the depressive dimension were markedly higher in psychotic depression and schizoaffective disorder. Bipolar disorder showed the highest factor scores for the manic and the general dimensions. Dimension scores based on ICD diagnostic categories are presented in Supplementary Fig. S2 and Supplementary Table S4.
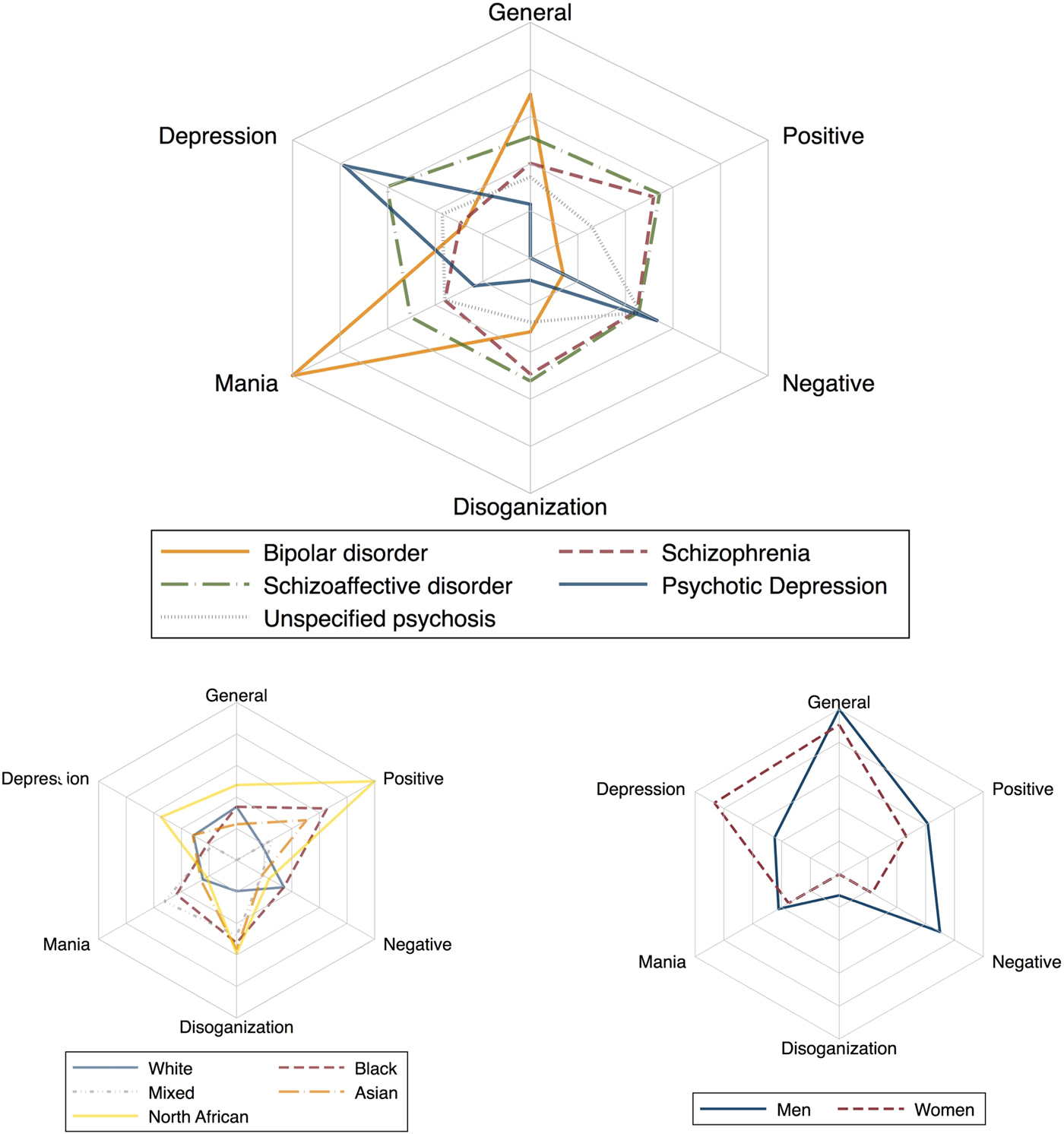
Fig. 2. Predicted symptom profiles by RDC-based diagnostic category, gender, and ethnicity. Explanatory note: After the estimation of the bifactor model, the continuous scores for general and specific symptom dimensions were computed using the function ‘FSCORES’ in Mplus (setting mean = 0 and standard deviation = 1), and used as the outcome variable in the regression analyses.
Table 4. Symptom dimension scores by sociodemographic, categorical diagnosis, and social context variables

B, unstandardised regression coefficient; CI, confidence interval.
a Covariates in multiple models were gender, age, ethnicity, diagnosis, study country, and type of assessment method (interview v. case records).
b Population density analysis was adjusted for gender, age, ethnicity, diagnosis, and type of assessment method (interview v. case records).
Finally, ROC analysis showed that classification accuracy into RDC categories based on general and specific symptom dimension scores was markedly higher for patients with psychopathology rating based either on face-to-face interview (95% CI 0.54–0.63) or case note review (95% CI 0.56–0.65), compared with a classification by chance (95% 0.32–0.41). Moreover, symptom dimensions showed similar diagnostic classification accuracy across countries (online Supplementary Figs S3.1 and S3.2).
Symptom dimensions by gender, age-at-first-contact, and ethnicity
Findings on factor scores by gender, age-at-first-contact, and ethnicity, are shown in Fig. 2 and Table 4. Early age-at-first-contact was associated with higher scores for the general, negative, disorganized, and manic symptom dimensions, and with lower scores for the depressive symptom dimension. Men showed fewer depressive symptoms and more negative symptoms than women, even after adjusting the analysis for several confounders. Table 4 further shows that participants of Black and North African ethnicity presented with higher scores on the positive symptom dimension compared with an individual of White ethnicity. Finally, higher scores for the disorganization dimension and lower scores for the depressive dimension were observed in Black compared with White ethnicity. Noteworthy, the magnitude of the effect was small for all the results.
Symptom dimensions by urbanicity
A moderate positive association was observed for more densely populated environments and the general dimension score. Table 4 further shows a weaker positive association between population density and specific negative, disorganization, and manic symptom dimensions. Post-hoc analysis of symptom dimensions within countries showed that positive symptoms were more common in urban study sites in the UK (i.e. London v. Cambridge), whereas a negative association was observed in Spain (online Supplementary Table S5).
Discussion
Principal findings
This is the first study on general and specific symptom dimensions in an incidence sample of psychosis. First, we found in our FEP sample that manic and delusional symptoms primarily underlie the identified general psychosis factor across diagnostic categories of non-affective and affective psychosis. Second, findings showed that specific dimensions of positive, negative, disorganized, manic and depressive symptoms are complementary to the general dimension. Third, general and specific symptom dimensions discriminated well between diagnoses of psychotic disorders. Forth, positive symptoms were more common among individuals of Black and North African ethnicity. Fifth, there was some evidence that early age-at-first-contact was associated with higher scores for several dimensions, such as of negative, disorganised and manic symptoms. Sixth, men presented with more negative and less depressive symptoms than women. Finally, higher scores for the general dimension were observed for individuals living in urban neighbourhoods.
Limitations
Before interpreting our findings, we must consider potential limitations. Symptoms were rated with a semi-structured face-to-face interview or from case note review. Still, study investigators underwent a specific and centrally organized training for OPCRIT and demonstrated good inter-rater reliability for individual item ratings; moreover, OPCRIT is a tool specifically designed to allow use with different sources (McGuffin et al., Reference McGuffin, Farmer and Harvey1991; Cardno et al., Reference Cardno, Jones, Murphy, Asherson, Scott, Williams, Owen and McGuffin1996; Rucker et al., Reference Rucker, Newman, Gray, Gunasinghe, Broadbent, Brittain, Baggaley, Denis, Turp, Stewart, Lovestone, Schumann, Farmer and McGuffin2011). However, we found consistently lower symptom ratings using case note review compared with face-to-face interviews. It is possible that clinicians failed to record all symptoms; alternatively, patients presenting with less severe psychopathology had a shorter contact with services, and therefore less chances to be interviewed by researchers. Whether or not differences in ratings are genuine or a surrogate of different sources of item ratings, we treated this potential bias as artificial confounding of our findings and adjusted all analyses for the type of assessment method. On the other hand, the use of an incidence sample allowed the best possible approximation of the true distribution of psychosis symptoms at FEP, which may have reduced potentially inflated presence of positive and negative symptoms in previous studies conducted in hospital settings (Allardyce et al., Reference Allardyce, Suppes and Van Os2007). Also, OPCRIT does not cover some relevant aspects of negative symptoms related to passive social withdrawal, lack of motivation, and difficulties in abstract/symbolic thinking. Consequently, we constructed a narrow negative symptom dimension with three items. Finally, some authors have argued that, in a bifactor model, the general factor may be difficult to interpret and in general may overfit the data (Bonifay et al., Reference Bonifay, Lane and Reise2016). However, the bifactor model allows solutions to dimensionality issues that arise when the conceptual breadth of a construct cannot be fully determined (Reise et al., Reference Reise, Morizot and Hays2007), as is likely to be the case for the construct of psychosis, which, in the past, has been considered as unidimensional and multidimensional at the same time. For example, the bifactor model discerns each specific symptom dimension from the common item effect, which is captured by the general dimension, thus allowing an accurate evaluation of the unique contribution of each subset of symptoms. Last, this solution provides crucial information which cannot be determined from the other models, i.e. how much of the phenotypic variance that we aim to measure is due to a unidimensional construct v. a multidimensional construct of psychosis. Hence, it was a suitable model for addressing dimensionality issues for psychosis and generating reliable phenotypes.
Comparison with previous research
In our study, the bifactor model of psychopathology best explained the observed symptoms at FEP compared with unidimensional and multidimensional models. Our findings are consistent with, and extend, previous research on psychotic symptoms in people with enduring psychotic disorders (Reininghaus et al., Reference Reininghaus, Priebe and Bentall2013; Reininghaus et al., Reference Reininghaus, Bohnke, Hosang, Farmer, Burns, McGuffin and Bentall2016) and the general population (Shevlin et al., Reference Shevlin, McElroy, Bentall, Reininghaus and Murphy2017) to a multinational incidence sample of FEP. They provide further evidence that non-affective and affective psychotic disorders lie on a common mood-psychosis spectrum (Murray et al., Reference Murray, Sham, Van Os, Zanelli, Cannon and McDonald2004). In addition, we provided the first evidence in psychosis that a bifactor solution shows better model fit statistics compared with a second-order hierarchical solution. However, compared with findings in enduring psychosis (Reininghaus et al., Reference Reininghaus, Bohnke, Hosang, Farmer, Burns, McGuffin and Bentall2016), we found a less specific general psychopathology factor with more general disturbances and affective features. As illnesses develop, the non-affective psychotic phenomena may become more and affective features less prominent.
We found some evidence of gender differences in symptom dimension scores. Men showed less depressive symptoms and more negative symptoms compared with women. This finding is consistent with other studies in stable schizophrenia (Shtasel et al., Reference Shtasel, Gur, Gallacher, Heimberg and Gur1992; Roy et al., Reference Roy, Maziade, Labbé and Mérette2001; Galderisi et al., Reference Galderisi, Bucci, Ucok and Peuskens2012), first episode psychotic disorder (Morgan et al., Reference Morgan, Castle and Jablensky2008), and the general population (Maric et al., Reference Maric, Krabbendam, Vollebergh, de Graaf and van Os2003). In our sample, we also showed that early age-at-first-contact was associated with a higher level of general and specific psychopathology. Notably, it has been proposed that gender-related and symptom profiles differences in psychosis may be suggestive of different neurodevelopmental trajectories (Castle and Murray, Reference Castle and Murray1991; Seeman, Reference Seeman1997; Riecher-Rössler and Häfner, Reference Riecher-Rössler and Häfner2000).
We further found that symptom dimensions vary in terms of ethnicity. Consistent with a previous report (Kirkbride et al., Reference Kirkbride, Hindocha, Hameed, Perez and Jones2016), we provided evidence that people of Black ethnicity presented at FEP with more positive and disorganized symptoms and fewer depressive symptoms compared with people of White ethnicity. Moreover, in line with another study (Veling et al., Reference Veling, Selten, Mackenbach and Hoek2007), we found in our sample that the North African group presented at FEP with more positive symptoms compared with people of White ethnicity. It has been debated whether similar findings reflect true differences in symptom presentation or instead result from raters being more likely to overrate symptoms in the context of ethno-cultural diversity (Mukherjee et al., Reference Mukherjee, Shukla, Woodle, Rosen and Olarte1983; Hutchinson et al., Reference Hutchinson, Takei, Sham, Harvey and Murray1999; Barrio et al., Reference Barrio, Yamada, Atuel, Hough, Yee, Berthot and Russo2003; Arnold et al., Reference Arnold, Keck, Collins, Wilson, Fleck, Corey, Amicone, Adebimpe and Strakowski2004; Vega and Lewis-Fernandez, Reference Vega and Lewis-Fernandez2008). Recent studies using standardized procedures for assessing symptomatology blind to ethnicity have suggested that misdiagnosis or rating bias cannot account for differences across ethnic groups (Morgan et al., Reference Morgan, Charalambides, Hutchinson and Murray2010). However, we must remain cautious in interpreting these results.
We showed that high population density is positively associated with the general and specific disorganized, negative and manic dimensions. In our multinational sample, we were not able to replicate previous findings on the relationship between urbanicity and the positive dimension (Kirkbride et al., Reference Kirkbride, Boydell, Ploubidis, Morgan, Fearon, Dazzan, Morgan, Murray and Jones2007). Nevertheless, stratified analysis by country was consistent with the previously reported association between urbanicity and positive symptoms in the UK. The relationship between urbanicity and a higher incidence of psychotic disorders is well-established (Vassos et al., Reference Vassos, Pedersen, Murray, Collier and Lewis2012). However, it has been found to show non-linearity (Kirkbride et al., Reference Kirkbride, Hameed, Ankireddypalli, Ioannidis, Crane, Nasir, Kabacs, Metastasio, Jenkins, Espandian, Spyridi, Ralevic, Siddabattuni, Walden, Adeoye, Perez and Jones2017), which implies that the effect of urbanicity may depend on exposure to additional socio-environmental factors associated with urban contexts, for example cannabis use (Kuepper et al., Reference Kuepper, van Os, Lieb, Wittchen and Henquet2011) and childhood adversities (Frissen et al., Reference Frissen, Lieverse, Drukker, van Winkel, Delespaul and Investigators2015). Similarly, our findings support the hypothesis that urban environment does not have a dimension-specific effect and may act to confer risk for different psychopathological outcomes in psychosis (van Os et al., Reference van Os, Hanssen, de Graaf and Vollebergh2002). Noteworthy, similar findings have been reported in the general population (van Os et al., Reference van Os, Hanssen, Bijl and Vollebergh2001), which may require future studies to consider the additive interaction between putative risk factors for psychosis and urbanicity.
Implications
In the context of a general effort to move away from DSM and ICD categories (Demjaha et al., Reference Demjaha, Morgan, Morgan, Landau, Dean, Reichenberg, Sham, Fearon, Hutchinson, Jones, Murray and Dazzan2009; Reininghaus et al., Reference Reininghaus, Bohnke, Hosang, Farmer, Burns, McGuffin and Bentall2016; Kotov et al., Reference Kotov, Krueger, Watson, Achenbach, Althoff, Bagby, Brown, Carpenter, Caspi and Clark2017; Van Dam et al., Reference Van Dam, O'Connor, Marcelle, Ho, Cameron Craddock, Tobe, Gabbay, Hudziak, Xavier Castellanos, Leventhal and Milham2017; Whalen, Reference Whalen2017; Zachar and Kendler, Reference Zachar and Kendler2017), we found evidence that supports, and may inform, the use of dimensional measures in the field of psychosis. In our sample, the bifactor model was a valid platform for research into FEP. Nevertheless, the plausibility of our statistically-guided approach depends on the extent to which: (1) symptom dimensions represent coherent environmental and biological factors; and (2) meaningful clinical information or decisions may derive from the latent constructs.
From a research perspective, our findings suggest that the general dimension may reflect a phenotype for the study of general risk factors. For example, urbanicity may impact on the risk and profile of psychosis through the combination of other, more specific socio- or bio-environmental factors. In addition, we showed a substantial variation of sociodemographic determinants at the specific dimension level, which may support an integrated socio-developmental model of psychosis (Morgan et al., Reference Morgan, Charalambides, Hutchinson and Murray2010).
We may further suggest using the general dimension as a quantitative measure of psychopathology for research into the genetic component shared across psychotic disorders. The evidence is required to establish the extent to which pathophysiology of schizophrenia, bipolar disorder, and psychotic depression is shared at the level of pathways and neuronal cell mechanisms (Forstner et al., Reference Forstner, Hecker, Hofmann, Maaser, Reinbold, Muhleisen, Leber, Strohmaier, Degenhardt, Treutlein, Mattheisen, Schumacher, Streit, Meier, Herms, Hoffmann, Lacour, Witt, Reif, Muller-Myhsok, Lucae, Maier, Schwarz, Vedder, Kammerer-Ciernioch, Pfennig, Bauer, Hautzinger, Moebus, Schenk, Fischer, Sivalingam, Czerski, Hauser, Lissowska, Szeszenia-Dabrowska, Brennan, McKay, Wright, Mitchell, Fullerton, Schofield, Montgomery, Medland, Gordon, Martin, Krasnov, Chuchalin, Babadjanova, Pantelejeva, Abramova, Tiganov, Polonikov, Khusnutdinova, Alda, Cruceanu, Rouleau, Turecki, Laprise, Rivas, Mayoral, Kogevinas, Grigoroiu-Serbanescu, Becker, Schulze, Rietschel, Cichon, Fier and Nothen2017). Based on the data presented on specific symptom dimensions, it is intriguing to speculate whether the distribution of psychotic symptoms reflects a gradient of neurodevelopmental impairment or socio-environmental risk (Morgan et al., Reference Morgan, Charalambides, Hutchinson and Murray2010; Howes and Murray, Reference Howes and Murray2014) resulting in different patterns of functional abnormalities (Murray and Lewis, Reference Murray and Lewis1987; Murray et al., Reference Murray, O'Callaghan, Castle and Lewis1992; Demjaha et al., Reference Demjaha, MacCabe and Murray2011; Owen and O'Donovan, Reference Owen and O'Donovan2017).
From a clinical perspective, although each patient presents with a specific pattern of psychopathology and response to treatment at FEP, attention has been traditionally focused on the positive dimension management. Mental health professionals may integrate observations of the whole range of symptoms and signs with a consideration of neurodevelopmental and socio-environmental risk factors. Such an approach should aim to plan and optimize pharmacological and non-pharmacological treatments (Murray et al., Reference Murray, Quattrone, Natesan, van Os, Nordentoft, Howes, Di Forti and Taylor2016), thus focusing further on treatment of negative, disorganized and affective dimensions (Wykes et al., Reference Wykes, Huddy, Cellard, McGurk and Czobor2011; Giacco et al., Reference Giacco, McCabe, Kallert, Hansson, Fiorillo and Priebe2012; Carbon and Correll, Reference Carbon and Correll2014; Pelayo-Teran et al., Reference Pelayo-Teran, Diaz, Perez-Iglesias, Suarez-Pinilla, Tabares-Seisdedos, de Leon and Crespo-Facorro2014; Rosenbaum et al., Reference Rosenbaum, Tiedemann, Sherrington, Curtis and Ward2014).
We may further suggest promoting mental health professionals to adopt treatment plans guided by dimensions, and increasing their confidence in dimensional classifications. Reconciling contradictory concerns of clinicians and researchers (Kendell and Jablensky, Reference Kendell and Jablensky2003) may represent the first milestone towards a gradual nosology refinement.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291718002131
Acknowledgements
The EU-GEI Project was funded by the European Community's Seventh Framework Programme under grant agreement No. HEALTH-F2-2010-241909 (Project EU-GEI). The work was further funded by: Clinician Scientist Medical Research Council fellowship (project reference MR/M008436/1) to MDF; Veni grant from the Netherlands Organisation for Scientific Research (grant no. 451-13-022) to UR; Sir Henry Dale Fellowship, jointly funded by the Wellcome Trust and the Royal Society (grant no. 101272/Z/13/Z) to JBK; National Institute for Health Research (NIHR) Biomedical Research Centre for Mental Health at South London and Maudsley NHS Foundation Trust and King's College London. The Brazilian study was funded by the Säo Paulo Research Foundation under grant number 2012/0417-0. Funders were not involved in design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript, and decision to submit the manuscript for publication.
Conflict of interest
The authors have no conflicts of interest to declare in relation to the work presented in this paper.
Appendix
Non-author EU-GEI collaborators
Kathryn Hubbard1, Stephanie Beards1, Simona A. Stilo2, Mara Parellada3, Pedro Cuadrado4, José Juan Rodríguez Solano5, Angel Carracedo6, Enrique García Bernardo7, Laura Roldán3, Gonzalo López3, Bibiana Cabrera8, Esther Lorente-Rovira9, Paz Garcia-Portilla10, Javier Costas6, Estela Jiménez-López11, Mario Matteis3, Marta Rapado3, Emiliano González3, Covadonga Martínez3, Emilio Sánchez7, Ma Soledad Olmeda7, Nathalie Franke12, Fabian Termorshuizen13,14, Daniella van Dam12, Elsje van der Ven13,14, Elles Messchaart14, Marion Leboyer15–18, Franck Schürhoff15–18, Stéphane Jamain16–18, Grégoire Baudin15,16, Aziz Ferchiou15,16, Baptiste Pignon15,16,18, Jean-Romain Richard16,18, Thomas Charpeaud18,19,21, Anne-Marie Tronche18,19,21, Flora Frijda22, Giovanna Marrazzo23, Lucia Sideli22, Crocettarachele Sartorio22,23, Fabio Seminerio22, Camila Marcelino Loureiro24,25, Rosana Shuhama24,25, Mirella Ruggeri26, Sarah Tosato26, Chiara Bonetto26 and Doriana Cristofalo26.
Affiliations
1Department of Health Service and Population Research, Institute of Psychiatry, King's College London, De Crespigny Park, Denmark Hill, London SE5 8AF, UK
2Department of Psychosis Studies, Institute of Psychiatry, King's College London, De Crespigny Park, Denmark Hill, London SE5 8AF, UK
3Department of Child and Adolescent Psychiatry, Hospital General Universitario Gregorio Marañón, School of Medicine, Universidad Complutense, IiSGM (CIBERSAM), C/Doctor Esquerdo 46, 28007 Madrid, Spain
4Villa de Vallecas Mental Health Department, Villa de Vallecas Mental Health Centre, Hospital Universitario Infanta Leonor / Hospital Virgen de la Torre, C/San Claudio 154, 28038 Madrid, Spain
5Puente de Vallecas Mental Health Department, Hospital Universitario Infanta Leonor/Hospital Virgen de la Torre, Centro de Salud Mental Puente de Vallecas, C/Peña Gorbea 4, 28018 Madrid, Spain
6Fundación Pública Galega de Medicina Xenómica, Hospital Clínico Universitario, Choupana s/n, 15782 Santiago de Compostela, Spain
7Department of Psychiatry, Hospital General Universitario Gregorio Marañón, School of Medicine, Universidad Complutense, IiSGM (CIBERSAM), C/Doctor Esquerdo 46, 28007 Madrid, Spain
8Department of Psychiatry, Hospital Clinic, IDIBAPS, Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM), Universidad de Barcelona, C/Villarroel 170, escalera 9, planta 6, 08036 Barcelona, Spain
9Department of Psychiatry, School of Medicine, Universidad de Valencia, Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM), C/Avda. Blasco Ibáñez 15, 46010 Valencia, Spain
10Department of Medicine, Psychiatry Area, School of Medicine, Universidad de Oviedo, Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM), C/Julián Clavería s/n, 33006 Oviedo, Spain
11Department of Psychiatry, Servicio de Psiquiatría Hospital “Virgen de la Luz”, C/Hermandad de Donantes de Sangre, 16002 Cuenca, Spain
12Department of Psychiatry, Early Psychosis Section, Academic Medical Centre, University of Amsterdam, Meibergdreef 5, 1105 AZ Amsterdam, The Netherlands
13Rivierduinen Centre for Mental Health, Leiden, Sandifortdreef 19, 2333 ZZ Leiden, The Netherlands
14Department of Psychiatry and Neuropsychology, School for Mental Health and Neuroscience, South Limburg Mental Health Research and Teaching Network, Maastricht University Medical Centre, P.O. Box 616, 6200 MD Maastricht, The Netherlands
15AP-HP, Groupe Hospitalier “Mondor”, Pôle de Psychiatrie, 51 Avenue de Maréchal de Lattre de Tassigny, 94010 Créteil, France
16INSERM, U955, Equipe 15, 51 Avenue de Maréchal de Lattre de Tassigny, 94010 Créteil, France
17Faculté de Médecine, Université Paris-Est, 51 Avenue de Maréchal de Lattre de Tassigny, 94010 Créteil, France
18Fondation Fondamental, 40 Rue de Mesly, 94000 Créteil, France
19CMP B CHU, BP 69, 63003 Clermont Ferrand, Cedex 1, France
20EPS Maison Blanche, Paris 75020, France
21Université Clermont Auvergne, EA 7280, Clermont-Ferrand 63000, France
22Department of Experimental Biomedicine and Clinical Neuroscience, Section of Psychiatry, University of Palermo, Via G. La Loggia n.1, 90129 Palermo, Italy
23Unit of Psychiatry, “P. Giaccone” General Hospital, Via G. La Loggia n.1, 90129 Palermo, Italy
24Departamento de Neurociências e Ciencias do Comportamento, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo, Av. Bandeirantes, 3900-Monte Alegre- CEP 14049-900, Ribeirão Preto, SP, Brasil
25Núcleo de Pesquina em Saúde Mental Populacional, Universidade de São Paulo, Avenida Doutor Arnaldo 455, CEP 01246-903, SP, Brasil
26Section of Psychiatry, Department of Neuroscience, Biomedicine and Movement, University of Verona, Piazzale L.A. Scuro 10, 37134 Verona, Italy










