Introduction
For the first time in two decades, the suicide rate in the US declined for consecutive years from 2018 to 2020 (Garnett, Curtin, & Stone, Reference Garnett, Curtin and Stone2022). Recent data, however, have revealed potentially concerning differences in suicide rates among racial and ethnic groups. The decline in suicide appears primarily driven by a decline among non-Hispanic White individuals, while rates among Black and Hispanic individuals have continued to rise (Curtin, Reference Curtin2022; Garnett et al., Reference Garnett, Curtin and Stone2022). Although suicide is considered an outcome most impacting White individuals, especially White males, suicide rates among Black individuals increased by 30% from 2014 to 2019 (Ramchand, Gordon, & Pearson, Reference Ramchand, Gordon and Pearson2021).
Two well-documented risk factors for suicide are suicidal ideation (SI) and prior suicide attempts (SA) (Bostwick, Pabbati, Geske, & McKean, Reference Bostwick, Pabbati, Geske and McKean2016; Harris & Barraclough, Reference Harris and Barraclough1997). Existing literature suggests that suicidality may develop along a continuum, from less severe forms, including thoughts of death or SI, to more severe behavior, including SAs (Sveticic & De Leo, Reference Sveticic and De Leo2012). In 2005, the National Comorbidity Survey (NCS) reported that 34% of individuals with SI progressed to developing a plan and 72% progressed from a plan to making an attempt (Kessler, Borges, & Walters, Reference Kessler, Borges and Walters1999; Sveticic & De Leo, Reference Sveticic and De Leo2012). Intervening at earlier points along this continuum may thus prevent progression to more severe forms of behavior.
Little is known, however, about the differential prevalence of SI and SAs among under-represented racial and ethnic groups as compared to White individuals and whether there are differences in the percentage of individuals in these groups who receive mental health care or reasons some don't. One potential explanation for why suicide among Black and Hispanic individuals is increasing is that these groups may be less likely to receive mental health treatment at earlier points along the suicide continuum (Han, Compton, Gfroerer, & McKeon, Reference Han, Compton, Gfroerer and McKeon2014; Congressional Black Caucus, 2019). To better understand why suicide may be increasing among these groups and to develop effective preventive interventions along the suicide continuum, it is important not only to examine differential rates of SI and SAs among these groups but also to identify potential disparities in receipt of mental health services among racial and ethnic subgroups experiencing SI and SAs.
Since the US does not have a population-based surveillance system for suicidal thoughts or attempts, the field relies on estimates from epidemiologic surveys, which have presented mixed and outdated results. The Epidemiologic Catchment Area (ECA) study of 1980–1984 found that White individuals were 1.7 times more likely than Black and Hispanic individuals to report SAs, while the NCS of 1990–1992 and NCS-R of 2001–2003 found no significant difference in past-year SI or SAs between racial/ethnic subgroups (Kessler, Berglund, Borges, Nock, & Wang, Reference Kessler, Berglund, Borges, Nock and Wang2005; Moscicki et al., Reference Moscicki, O'Carroll, Rae, Locke, Roy and Regier1988). In addition, the 2001–2003 National Survey of American Life (NSAL) provides prevalence estimates of SI and SAs for African Americans and Caribbean Blacks and the 2002–2003 National Latino and Asian American Survey (NLAAS) provides prevalence estimates for Asian Americans and Latinos, but it is difficult to directly compare estimates across surveys (Cheng et al., Reference Cheng, Fancher, Ratanasen, Conner, Duberstein, Sue and Takeuchi2010; Joe, Baser, Breeden, Neighbors, & Jackson, Reference Joe, Baser, Breeden, Neighbors and Jackson2006; Joe, Baser, Neighbors, Caldwell, & Jackson, Reference Joe, Baser, Neighbors, Caldwell and Jackson2009). Thus, in the context of rising suicide rates among Black and Hispanic individuals, research is needed on current racial and ethnic differences in SI, SAs, and receipt of mental health treatment.
The current study uses nationally-representative data from the 2009–2020 National Survey on Drug Use and Health (NSDUH) (Substance Abuse and Mental Health Services Administration, 2020b) to compare proportions of non-Hispanic White, non-Hispanic Black, and Hispanic adults among those with no suicidal behavior, past-year SI, and past-year SAs and whether these differences are accounted for by co-morbidities. We also examine differences in mental health service use among racial/ethnic groups who report recent SI or SA and reasons for not using services. Through these analyses, we hope to shed light on rising rates of suicide among Black and Hispanic individuals and inform upstream interventions along the suicide continuum.
Methods
Data source and study sample
We used 2009–2020 data from NSDUH, which collects systematic information about drug use, health, and health services among non-institutionalized US civilians aged ⩾12 (Substance Abuse and Mental Health Services Administration, 2020b). NSDUH employs a multi-stage stratified sampling design to produce nationally-representative estimates. We limited our sample to adults aged ⩾18 who self-identified as non-Hispanic Black (hereafter referred to as Black), Hispanic, or non-Hispanic White (referred to as White) because suicide-related questions were only asked among adults (n = 426 008 unweighted). Participants received $30.00 for completion of the survey. The annual mean weighted response rate in 2009–2020 ranged from 60.4% to 75.6%. Response rates for racial and ethnic groups varied depending on the survey year but were comparable across years. For example, in the 2018 NSDUH, the weighted response rates for Hispanic, non-Hispanic Black, and non-Hispanic White individuals were 67, 73.1, and 66.2%, respectively, and 64.4, 70.6, and 64.7%, respectively, in the 2019 NSDUH (Substance Abuse and Mental Health Services Administration, 2020a).
This study was exempted from review by the Institutional Review Board at Yale School of Medicine as data are publicly available, de-identified. Study procedures followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline and updated guidance for reporting of race/ethnicity in medical research (Flanagin, Frey, Christiansen, & Committee, Reference Flanagin, Frey and Christiansen2021). Further details of the survey are available on the NSDUH website (Substance Abuse and Mental Health Services Administration, 2020b).
Measures
Suicidal thoughts and behaviors were assessed by several questions. SI was assessed by asking whether respondents had seriously thought about killing themselves (‘At any time in the past 12 months, did you seriously think about trying to kill yourself?’) or made a plan to kill themselves (‘During the past 12 months, did you make any plans to kill yourself?’). Those who responded yes to either question were asked if they had attempted to kill themselves in the past 12 months (SAs) (‘During the past 12 months, did you try to kill yourself?’) (Bommersbach, Rosenheck, & Rhee, Reference Bommersbach, Rosenheck and Rhee2022c; Substance Abuse and Mental Health Services Administration, 2018).
Sociodemographic characteristics included age, sex, marital status, education, employment, annual family income, health insurance coverage, and urban residence (based on metropolitan statistical areas) (US Census Bureau, 2020).
Past-year psychiatric disorders: Major depressive episode (MDE) was measured by a series of questions based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria for MDE (American Psychiatric Association, 1994). Substance use disorders (SUDs) were derived from questions addressing formal diagnostic criteria for substance abuse and dependence as defined in DSM-IV (American Psychiatric Association, 1994), which included alcohol, tobacco, cannabis, cocaine/crack, heroin/pain reliever, hallucinogen, stimulant, sedative, and an aggregate indicator of any substance abuse or dependence (excluding alcohol and tobacco).
Past-year mental health service use was assessed by questions concerning receipt of any outpatient or inpatient mental health services or prescription medications for mental health problems. Among respondents who did not report receipt of any mental health services, data were gathered about the subjective reasons for not receiving services from a list of 11 potential options.
Data analysis
First, the sample was divided into three groups: individuals with no past-year suicidal thoughts/behavior, past-year SI only, or a past-year SA. Next, bivariate logistic regression was used to compare the sociodemographic and clinical characteristics of the three groups, including whether the racial/ethnic subgroups were over or under-represented in the three groups. Odds ratios (OR) and 95% confidence intervals (CI) were reported.
Next, multivariable-adjusted analyses were conducted to determine if significant differences between the three comparison groups in the bivariate analyses remained significant after controlling for other factors associated with past-year suicidal thoughts/behaviors. In these models, past-year SI and SA were dependent variables while the primary independent variable of interest was racial/ethnic subgroups, and covariates included sociodemographic and clinical factors that had emerged as significantly associated with suicidal thoughts/behaviors in the bivariate analysis as well as survey year to identify period effects.
Next, we examined past-year mental health service use by racial/ethnic subgroup and year separately for those reporting SI and SAs. We further examined service use in a multivariable-adjusted interaction analysis in which mental health service use was the dependent variable. Independent variables included (1) main effects for Black and Hispanic individuals, (2) dichotomous variables representing SI and SA, and four interaction terms of each race by each type of suicidal thoughts/behavior. These analyses sought to determine whether individuals who are Black or Hispanic had greater or lesser likelihood of receiving mental health services, whether SI or SA were associated with service use, and whether the relationship of SI and SA to service use differed by racial/ethnic group.
Finally, among respondents who reported past-year SI or a SA and did not report receiving any mental health services, we compared the racial/ethnic groups on reasons for not receiving services.
We used Stata version 16.1 MP/4-Core for all analyses. We accounted for NSDUH complex survey design using svy commands to account for multi-stage, complex survey sampling techniques used in the data collection. We set p value <0.05 as the test of statistical significance.
Results
Characteristics of the study sample
In the entire NSDUH sample of adults aged ⩾18 from 2009 to 2020 (n = 426 008 unweighted, representing over 220 million adults nationwide), 20 791 (4.9%; representing 8 007 155 individuals) reported past-year SI alone, 3661 (0.9%; representing 1 123 676 individuals) reported past-year SI and SAs, and 401 556 individuals reported no suicidal thoughts/behavior. From 2009 to 2020, there was a significant increase in past-year SI, from 14.8% to 20.5% of all respondents (OR 1.33, 95% CI 1.21–1.45) but no significant change in the proportion of individuals with SI who reported past-year SAs (OR 1.14, 95% CI 0.92–1.40). We did not find any significant change in past-year SI or SAs between years 2019 and 2020 (i.e. pre- v. post-Covid-19 pandemic) for the study sample.
Bivariate comparison by suicidal thoughts/behavior
Compared to White individuals, Black individuals were significantly less likely to report past-year SI but among individuals with past-year SI, were more likely to report a past-year SA, as compared to no suicidal thoughts/behavior (Table 1, columns 4 and 5). Similarly, Black individuals with past-year SI were much more likely to report a past-year SA than past-year SI alone (OR 1.99, 95% CI 1.74–2.26) (Table 1, column 6). Hispanic individuals demonstrated similar patterns as they were significantly less likely to report past-year SI but were more likely to report a past-year SA, as compared to White individuals.
Table 1. Socio-demographic and clinical characteristics by suicidal thoughts/behavior among 426 008 US adults, 2009–2020

Note: Data are from National Survey on Drug Use and Health.
*<0.05; **<0.01; ***<0.001.
Multivariable-adjusted comparison by suicidal thoughts/behavior
In the multivariable analysis adjusted for factors significantly associated with suicidal thoughts/behavior in the bivariate, Black and Hispanic individuals remained significantly less likely than White individuals to report past-year SI, as compared to no suicidal thoughts/behavior [adjusted OR (aOR) 0.71, 95% CI 0.66–0.76; aOR 0.70, 95% CI 0.66–0.75, respectively] (Table 2). Black individuals with past-year SI also remained significantly more likely to report a past-year SA as compared to no suicidal thoughts/behavior, and much more likely when compared to SI alone (aOR 1.65, 95% CI 1.41–1.94). However, while Hispanic individuals were no longer more likely than White individuals to report a past-year SA as compared to no suicidal thoughts/behavior, they remained significantly more likely to report a past-year SA, as compared to those with SI alone (aOR 1.36, 95% CI 1.17–1.57).
Table 2. Multivariable-adjusted logistic regression models examining factors associated with suicidal thoughts/behaviors among 426 008 US adults, 2009–2020
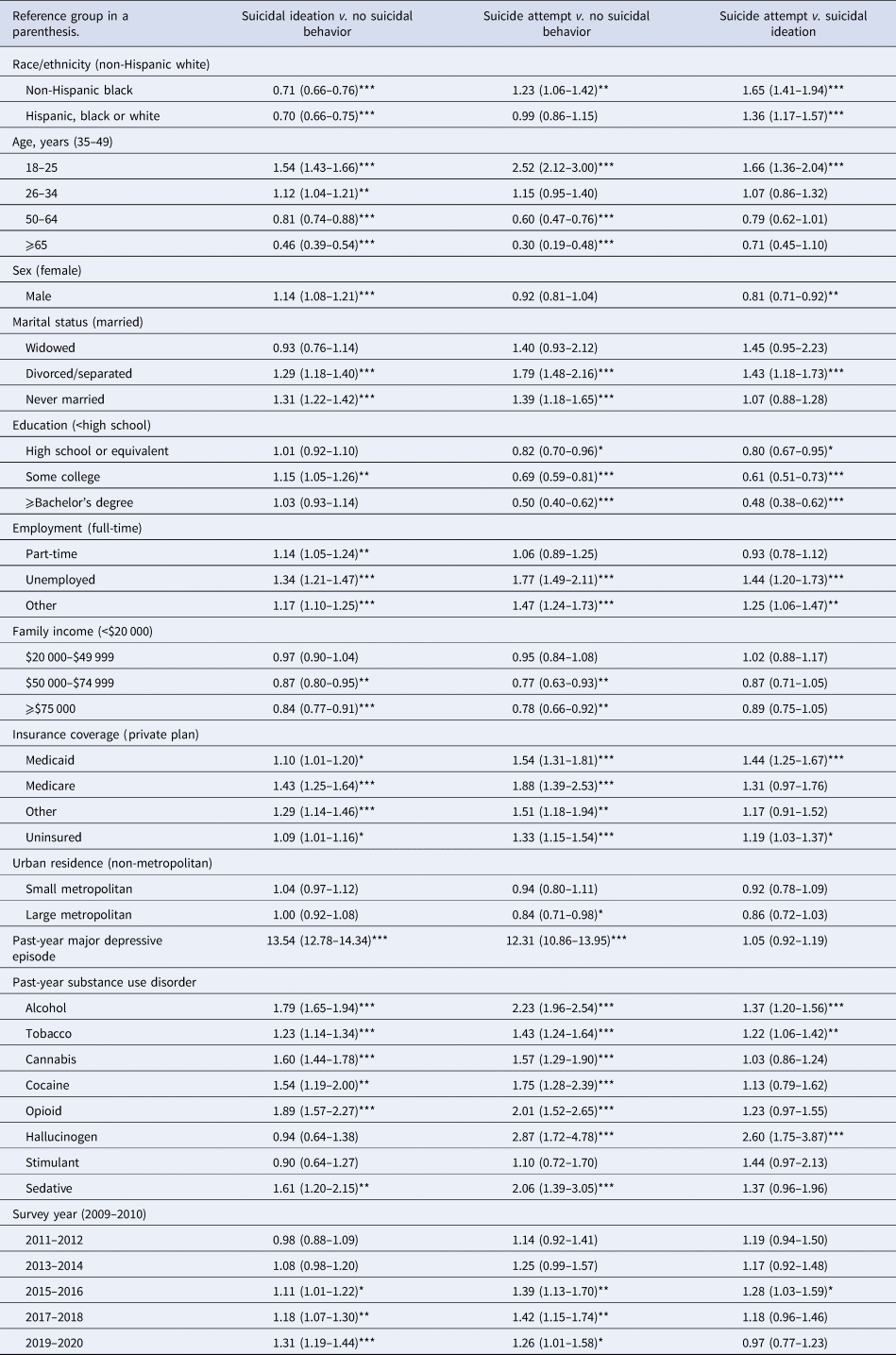
Note: Data are from National Survey on Drug Use and Health.
*<0.05; **<0.01; ***<0.001.
In subsequent interaction analyses, there was no significant interaction of race/ethnicity by survey year, by sex, or by either past-year SI or SA. Thus, the effects of race did not differ over the years, across sexes, or types of suicidal behavior. There was no consistent time trend that differentiated suicidality among Black or Hispanic individuals from Whites.
Mental health service use
Among individuals who reported past-year SI or SA from 2009 to 2020, lower percentages of Black and Hispanic individuals reported receiving mental health services, compared to White individuals (Fig. 1a and b).
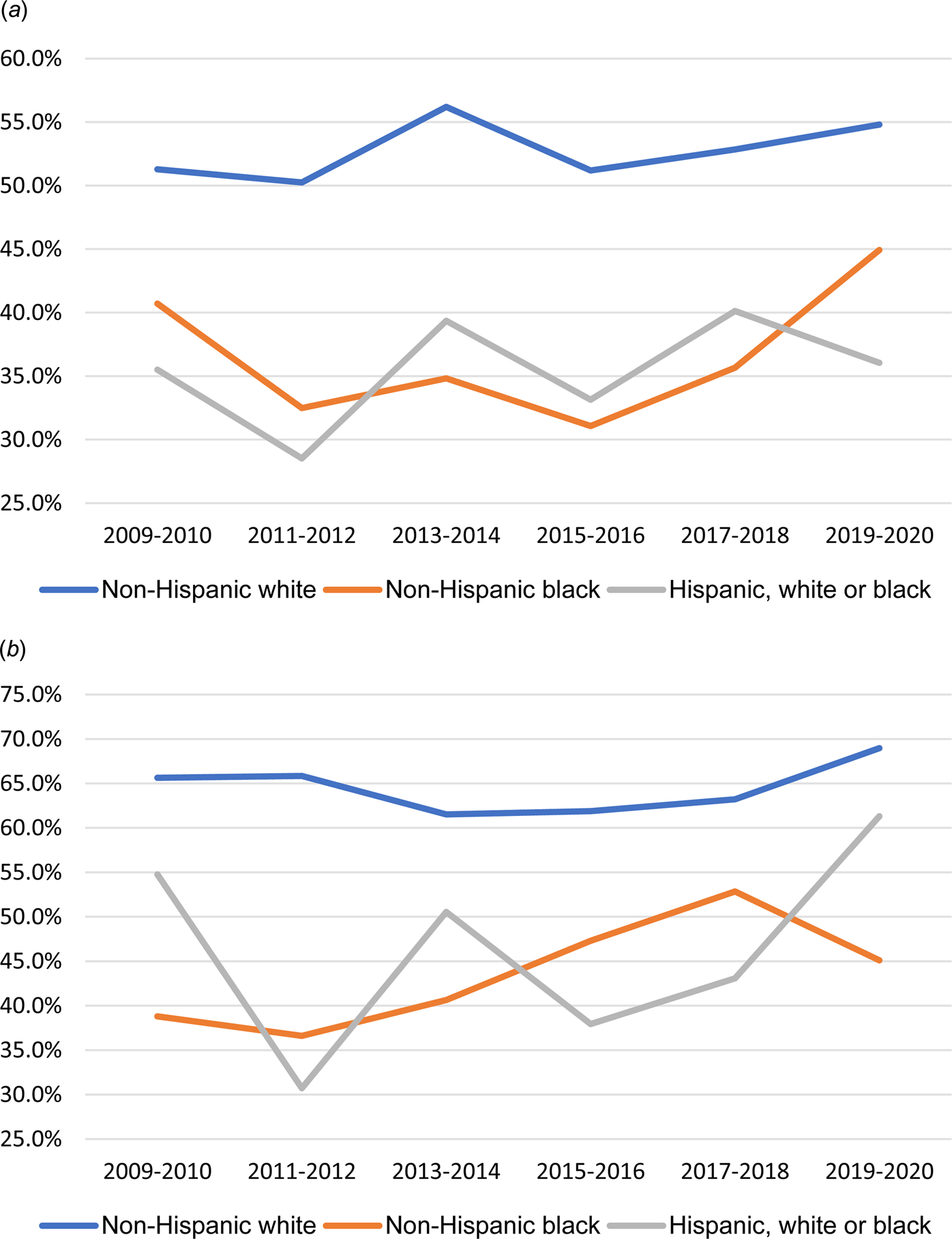
Fig. 1. Trends of receiving any mental health care in the past year by suicidal behaviors and race/ethnicity, 2009–2020. (a) Among US adults with past-year suicidal ideation, 2009–2020. (b) Among US adults with past-year suicide attempt, 2009–2020.
Note: Data are from National Survey on Drug Use and Health.
Multivariable-adjusted interaction analysis of past-year mental health service use (Table 3) showed significant main effects for suicidal thoughts/behavior on past-year mental health service use as well as main effects for race and ethnicity with Black and Hispanic individuals significantly less likely than White individuals to report receiving any mental health services (aOR 0.39, 95% CI 0.37–0.41; aOR 0.45, 95% CI 0.43–0.47, respectively). However, the interactions of race/ethnicity and past-year SI or SA in association with mental health service use were not significant, indicating that the significant relationship of SI and SA to mental health service use did not differ by racial/ethnic group. The results can also be understood as failing to support the possibility that the lower levels of service use among Black and Hispanic individuals account for either their lower risk for reporting SI or greater risk for reporting a SA.
Table 3. Multivariable-adjusted interaction analyses of mental health service use and race/ethnicity on suicidal behaviors among 426 008 US adults, 2009–2020
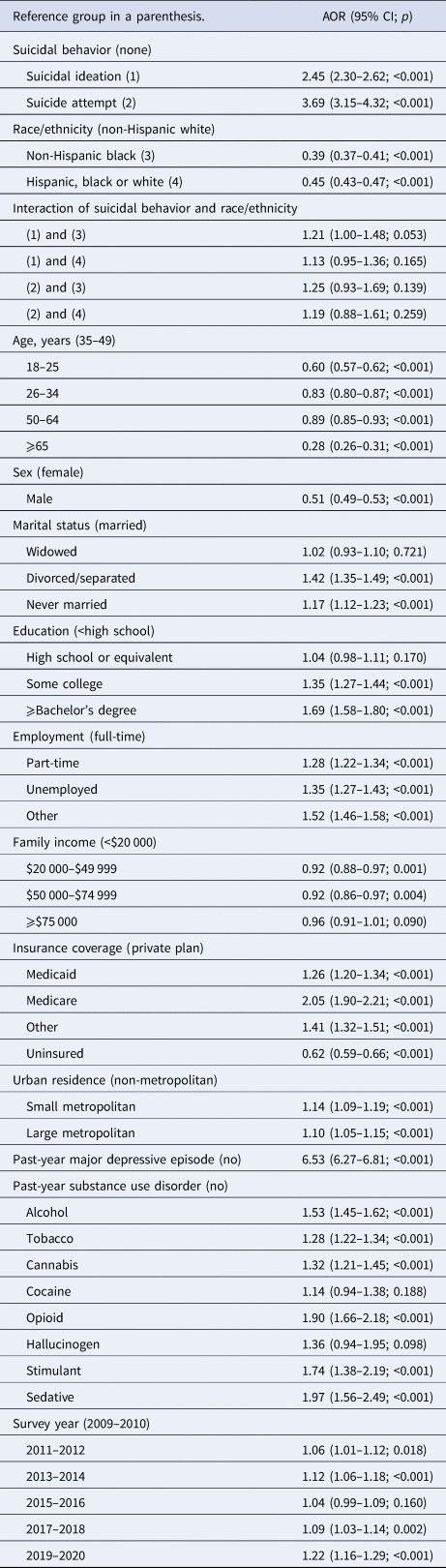
Note: Data are from National Survey on Drug Use and Health. AOR, adjusted odds ratio; CI, confidence interval.
Among those who did not receive services, Black and Hispanic individuals reporting SI were more likely to report not knowing where to go for mental health services (32.6% and 40.2%, respectively) and Hispanic individuals were more likely to report fearing that others would know they had received services (Table 4). Among those who made a past-year SA, Hispanic individuals were more likely to think they could handle without treatment and to fear that others would know they had received services.
Table 4. Reasons for not getting mental health treatment among those who did not receive mental health care by race/ethnicity and suicidal behavior, 2009–2020

Note: Data are from National Survey on Drug Use and Health.
Bold indicates sample sizes by suicidal behavior.
Discussion
In this nationally representative sample of US adults from 2009 to 2020, Black and Hispanic individuals were significantly less likely than White individuals to report past-year SI but among individuals with past-year SI, were significantly more likely to report a past-year SA, a result that was essentially unchanged after controlling for a large number of potentially confounding sociodemographic and clinical factors. Stated differently, Black and Hispanic individuals report less frequent thoughts of suicide than White individuals but when they do, they are more likely to report active attempts. Stark differences were also found in use of mental health services with less use by Black and Hispanic individuals. However, interaction analyses suggested no significant relationship between service use and racial/ethnic differences in SI or SA. There were few significant differences between racial/ethnic groups who did not use mental health services in the reasons for not using such services. Black and Hispanic individuals were more likely to report not knowing where to go for treatment and Hispanic individuals were more likely to report concerns about stigma.
While much attention has been focused on the recent increase in SAs and suicide deaths among Black adolescents (Congressional Black Caucus, 2019; Xiao, Cerel, & Mann, Reference Xiao, Cerel and Mann2021), very little attention has been paid to racial/ethnic differences in suicidal behavior among adults, despite the observed increase in suicide rates among Black and Hispanic adults in data from the National Center for Health Statistics (Curtin, Reference Curtin2022; Garnett et al., Reference Garnett, Curtin and Stone2022). Our results provide updated epidemiologic estimates of racial and ethnic differences in past-year SI and SAs and are believed to be the first study in adults to show that among individuals with past-year SI, Black adults may be more likely than Whites to report a past-year SA. These findings are consistent with several recent studies of adolescents showing that Black and Hispanic adolescents are less likely to report past-year SI but may be more likely to report SAs (Lindsey, Sheftall, Xiao, & Joe, Reference Lindsey, Sheftall, Xiao and Joe2019; Romanelli, Xiao, & Lindsey, Reference Romanelli, Xiao and Lindsey2020; Xiao, Romanelli, & Lindsey, Reference Xiao, Romanelli and Lindsey2019). Data from older epidemiologic surveys of adults, including the ECA, NCS, and NCS-R, either found no significant racial/ethnic difference or greater rates of SAs among White adults (Baca-Garcia et al., Reference Baca-Garcia, Perez-Rodriguez, Keyes, Oquendo, Hasin, Grant and Blanco2010; Kessler et al., Reference Kessler, Berglund, Borges, Nock and Wang2005; Moscicki et al., Reference Moscicki, O'Carroll, Rae, Locke, Roy and Regier1988; Olfson et al., Reference Olfson, Blanco, Wall, Liu, Saha, Pickering and Grant2017). In addition, data from the NSAL and NLAAS examined lifetime SI and SAs but did not directly compare suicidal thoughts/behavior across racial/ethnic groups (Cheng et al., Reference Cheng, Fancher, Ratanasen, Conner, Duberstein, Sue and Takeuchi2010; Joe et al., Reference Joe, Baser, Breeden, Neighbors and Jackson2006, Reference Joe, Baser, Neighbors, Caldwell and Jackson2009). It is important to note that our findings on SAs do not generalize to the general population as past-year SAs were only assessed among individuals who reported past-year SI, not among the entire survey sample. Another potential explanation for our diverging results include the possibility that SAs among Black individuals may have disproportionately increased in recent years compared to other racial groups, although we did not find evidence supporting this possibility. This explanation may find support from the finding of a recent study that past-year SAs among Black adults with MDE have nearly doubled and increased more than any other demographic subgroup (Bommersbach, Rosenheck, & Rhee, Reference Bommersbach, Rosenheck and Rhee2022b) [under review]. It is also possible that, even in the absence of a differential temporal trend, our use of a larger sample size resulted in greater power to detect differences between racial/ethnic groups.
Our results demonstrating that when Black and Hispanic individuals report suicidality, they are much more likely to report more severe suicidal behavior and less likely to report SI, and it is alarming given the recent rise in suicide deaths among Black and Hispanic individuals (Curtin, Reference Curtin2022). An often-cited explanation for this rise in suicide is that minoritized populations may be less likely to receive mental health care when experiencing suicidality, either due to reduced help-seeking behavior (Taylor & Kuo, Reference Taylor and Kuo2019), concerns about stigma (Nadeem et al., Reference Nadeem, Lange, Edge, Fongwa, Belin and Miranda2007), greater comfort with alternative treatment options, or structural barriers (Lillie-Blanton & Hoffman, Reference Lillie-Blanton and Hoffman2005). While our results demonstrate that Black and Hispanic individuals are less likely to receive mental health services, this did not account for the greater frequency of SA. Thus, other explanations are likely contributing to these findings.
Reporting styles may partially explain these results. Black and Hispanic individuals may be less likely to report suicidal thoughts or behavior until they reach a more severe threshold, either due to differences in socio-cultural norms for the expression of distress, perhaps reflecting greater mental health stigma. Our study clearly found Hispanic individuals experiencing suicidality were particularly concerned about stigma. Second, it is possible that disparities in aspects of service use not measured in this study may contribute to the findings. For example, Black and Hispanic individuals may be less likely to receive evidenced-based treatment or timely treatment in proximity to need, either due to possible provider bias and structural racism or less frequent expression of suicidality, as our study may suggest (Wang et al., Reference Wang, Lane, Olfson, Pincus, Wells and Kessler2005). Prior studies have demonstrated that Black patients are more likely to experience mental health treatment delays, less likely to receive prescription medication for depression, and report less satisfaction with services (Alegria et al., Reference Alegria, Chatterji, Wells, Cao, Chen, Takeuchi and Meng2008; Bommersbach, Jegede, Stefanovics, Rhee, & Rosenheck, Reference Bommersbach, Jegede, Stefanovics, Rhee and Rosenheck2022a; Cook et al., Reference Cook, Zuvekas, Carson, Wayne, Vesper and McGuire2014, Reference Cook, Hou, Lee-Tauler, Progovac, Samson and Sanchez2019; Maura & Weisman de Mamani, Reference Maura and Weisman de Mamani2017; McFarland & Klein, Reference McFarland and Klein2005; Olfson, Cherry, & Lewis-Fernandez, Reference Olfson, Cherry and Lewis-Fernandez2009; Remmert, Guzman, Mavandadi, & Oslin, Reference Remmert, Guzman, Mavandadi and Oslin2022; Wang et al., Reference Wang, Lane, Olfson, Pincus, Wells and Kessler2005; Wells, Klap, Koike, & Sherbourne, Reference Wells, Klap, Koike and Sherbourne2001). Additionally, our results suggest that Black and Hispanic individuals with SI are less likely to know where to go for treatment, suggesting a failure of the mental health system to ensure services are known and approachable for these populations. A better understanding of how these well-documented disparities impact outcomes among minoritized populations with suicidal thoughts or behavior are needed (Washington, 2006).
These results have a number of potential implications for suicide prevention. First, providers should be aware of increasing rates of suicide and higher rates of SAs among Black and Hispanic individuals. Training on suicide risk assessment should avoid propagating generalized beliefs that White males are most impacted by suicidality. Such teaching may result in under-recognition of suicidality among Black and Hispanic individuals. In addition, the results of our study raise the question of whether Black and Hispanic individuals are more likely to under-report SI. Such a finding may have impeded accurate clinical assessment of suicidality, but requires replication in clinical samples.
Additionally, as research continues to shed light on potential racial/ethnic differences in suicidal behavior, suicide prevention programs would do well to recognize differential risks for suicide across race/ethnicity, including the interpersonal and structural impacts of racism, adverse childhood experiences, and socioeconomic disparities (Washington, 2006; Xiao et al., Reference Xiao, Cerel and Mann2021). Continued efforts to dismantle structural racism in healthcare settings is critical to ensuring that Black and Hispanic individuals experiencing suicidality feel comfortable seeking professional care and receive timely, evidence-based care. In addition, interventions outside the healthcare system to improve identification of high-risk individuals are needed, including training in suicide risk assessment for clergy, religious leaders, and school personnel; public health promotion campaigns that target mental health stigma, especially among Hispanic populations; and continued expansion of community-based crisis services.
Several potential limitations deserve mention. Most notably, the retrospective, self-report nature of the data introduces the possibility of recall and reporting bias. Future research could consider examining medically-verifiable SAs to mitigate this limitation. In addition, SAs were only assessed among individuals reporting past-year SI so, as stated previously, our findings on SAs are only applicable to individuals with SI. In addition, SAs were assessed with a single question that may have mis-classified non-suicidal self-injury. Third, NSDUH does not survey individuals who are currently incarcerated. Given that racial minorities are over-represented in prisons and jails, rates of SI and SAs may have been underestimated in this study. Finally, the broad racial and ethnic categories available in NSDUH did not allow for more nuanced understanding of racial and ethnic subgroups (Jegede, Na, Rhee, Stefanovics, & Rosenheck, Reference Jegede, Na, Rhee, Stefanovics and Rosenheck2021).
In spite of these limitations, this nationally representative study suggests that Black and Hispanic individuals are less likely than White individuals to report SI but when they do, they are more likely to report attempts. While they are less likely to report receiving mental health treatment, less service use does not underlie the difference in suicidal behavior across racial/ethnic groups. Thus, it is likely that other factors, including differences in reporting styles, socio-culturally acceptable forms of distress, and possible structural racism in the mental health system, may differentially impact racial/ethnic subgroups and risk of both suicide precursors and suicide mortality. Further study of these phenomena is needed.
Data
The data have not been previously presented orally or by poster at scientific meetings.
Author contributions
Study concept and design: all authors; data acquisition and statistical analyses: Rhee; interpretation of data: all authors; drafting of manuscript: Bommersbach and Rhee; critical revision of manuscript for important intellectual content: all authors.
Conflict of interest
Each author completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Bommersbach reported none. Rosenheck reported none. Rhee was supported in part by the National Institute on Aging (NIA) through Yale School of Medicine (#T32AG019134) in the past 3 years. Dr Rhee has also been funded by the NIA (R21AG070666), National Institute of Mental Health (#R21MH117438), and Institute for Collaboration on Health, Intervention, and Policy (InCHIP) of the University of Connecticut. Dr Rhee serves as a review committee member for Patient-Centered Outcomes Research Institute (PCORI) and Substance Abuse and Mental Health Services Administration (SAMHSA) and has received honoraria payments from PCORI and SAMHSA. Dr Rhee has also served as a stakeholder/consultant for PCORI and received consulting fees from PCORI. Dr Rhee is currently a co-editor-in-chief of Mental Health Science and is pending to receive honorarium payments annually from the publisher, John Wiley & Sons, Inc.








