Introduction
Ageing is frequently said to be at the top of the policy agenda, locally, nationally and internationally. The Brown Government positioned it alongside climate change and terrorism as one of the three ‘grand challenges’ facing the UK. Look closer, however, and it is not ‘ageing’, the lifelong process, but old age that is at the forefront of political concerns. From a combined critical social policy and critical gerontology perspective (Estes, Reference Estes2001; Baars et al., Reference Baars, Dannefer, Phillipson and Walker2006) this paper argues that this narrow focus restricts the scope of social policy and, far worse, it results in needless pain, discomfort and reduced quality of life among hundreds of thousands of older people, and will continue to do so unless a new approach is taken. Globally, too, blinkered policy thinking is undermining effective responses to the ageing challenge. To support these bold claims this article adduces recent research findings, including those from the largest programme of research on ageing ever mounted in the UK and one of the largest in the world, to establish the solid foundations for a new approach. Then, given the weight of evidence supporting this, the conundrum of policy inaction is considered. The article concludes by sketching the outlines of a possible social policy on ageing aimed at prioritising the life course, called ‘active ageing’. Projected increases in the scale of age-associated chronic conditions add urgency to the need for such a social policy. While the case is made in terms of UK policy and practice the need for concerted action to prevent chronic conditions is global.
It is argued that the critical component of this social policy on ageing is a life-course perspective. This recognises, first, that life experiences powerfully shape how people grow old and, secondly, that these experiences are socially rather than biologically constructed (Elder, Reference Elder1975; Dannefer, Reference Dannefer2003; Walker, Reference Walker and Baars2006). This perspective opens the way not only for social analyses of the factors that cumulatively determine different life-course trajectories and old age outcomes, and inequalities in both, but also for social policies that reflect the true dynamic nature of ageing, rather than static conventional notions of ‘natural stages of life’.
The ageing challenge
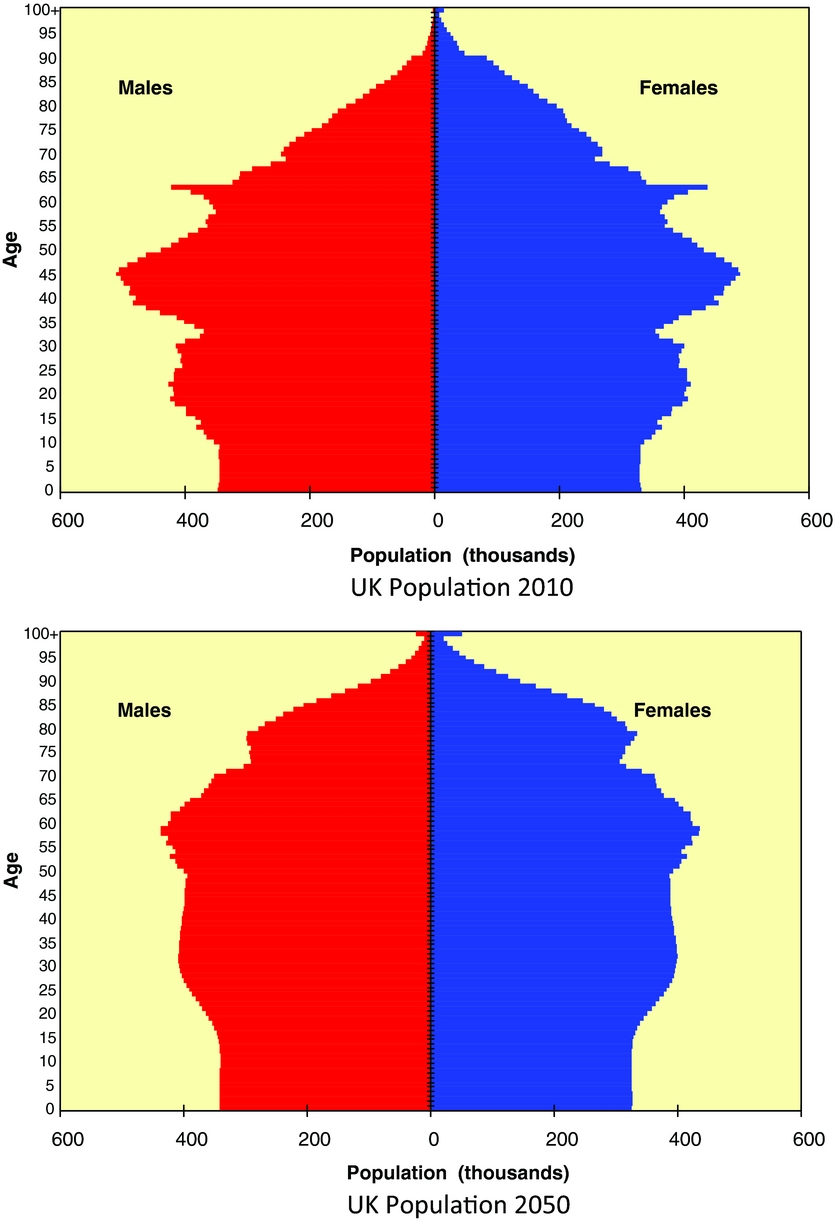
Social policy analysts are well aware of the demographic revolution taking place and so this essential background is restricted to only a brief summary. Population ageing results from a combination of declining fertility and rising longevity. On the one hand for nearly 40 years the UK fertility rate has been below the replacement level (i.e. the level needed to maintain population size) of 2.1 children per woman. In 2014, the total fertility rate was 1.83 children per woman and the average age of mothers increased to 30.2 years. On the other hand, while life expectancy increases were originally the result of reductions in infant mortality, it is now falling rates at older ages that are driving the remarkable extension of life. For example, the mortality rate for women in their early 80s has declined from 120 per 1000 population in the 1950s to 75 per 1000 by the 1990s, and for men in their early 80s the decline was from 160 to 120 per 1000 population (ONS, 2015). There are other influences on population ageing, including net migration and the age of inward and outward migrants, and the larger than average birth cohorts in the 1950s and 1960s, but these two are by far the most important. As in other developed countries this combination results in a transition in the age structure of the population, shown in Figure 1, from a pyramid to a pear shape. In fact, according to the United Nations (UN), the UK has been an ‘ageing society’ since 1930 when the age group 65+ reached 7 per cent of the total population (UN, 2005), and is expected to attain ‘super-aged’ status around 2020 when this age group breaks the 20 per cent barrier.
Perhaps the UN was premature in allocating these classifications to countries that still have relatively small older populations. A careful look at demographic history would have revealed that life expectancy had been rising, in a linear fashion, since 1840 and shows no signs of abating (Oeppen and Vaupel, Reference Oeppen and Vaupel2002). The ONS (2015) projects a continuation of this trend: around 75 per cent of UK population growth between 2012 and 2040 is in the over-60 age group, with increases from 14 to 22 million. Within that broad age group, the fastest growing section of the UK population is the oldest-old, those aged 85 and over, and the ONS projects an exponential rise in the number of centenarians (Figure 2).
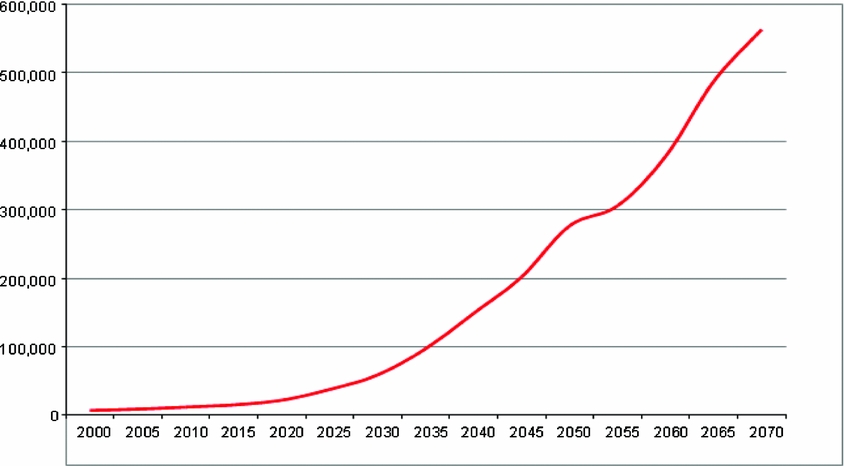
Figure 2 Numbers and projections of centenarians, UK 2000–2065
Clearly such momentous shifts in population age structure cannot occur without presenting major challenges to all levels of society – from the increasing risk of precarity faced by older women who assume the main responsibility in caring for their aged parents, to the ageing workforce, to the currently rising need for long-term care among the very elderly. These are challenges aplenty for social policy and, in addition, there are major issues around the distribution of resources between generations, when one end of the life course is shrinking and the other is expanding. The rise in life expectancy has produced a relatively new social risk, the need for extended care in late old age, which the UK has not planned for adequately compared, for example, to Germany (Glendenning and Igl, Reference Glendenning, Igl, Walker and Naegele2009). Indeed, insufficient planning has been transformed into a ‘care crisis’ by the austerity programmes of the 2010 Coalition and 2015 Conservative Government (Foster et al., Reference Foster, Haux, Brenton and Deeming2014; ADASS, 2015). The UK's response to these challenges has been, at best, reactive and largely remedial. The challenge of ageing has not been taken up either comprehensively or consistently, despite some highly promising signs in the early years of the century (Cabinet Office, 2002; DWP, 2005; DCLG, 2008). While it did consider some of the main policy questions arising from population ageing, such as longer working lives, housing, health and the family, the Foresight Review (Government Office for Science, 2016) did not take the opportunity to adopt a comprehensive social policy framework.
The new dynamics of ageing
Whereas this demographic context is quite well known, new evidence provides powerful insights into the drivers and consequences of both individual and population ageing. In particular the New Dynamics of Ageing (NDA) research Programme amassed a wealth of such vital evidence that should inform policy and practice.
The 10-year NDA Programme was the first multi-disciplinary collaboration between five UK Research Councils (AHRC, BBSRC, EPSRC, ESRC and MRC) and thus spanned all disciplines with relevance to ageing. The Programme was established in 2005 with the aims of understanding the changing nature of ageing, the various influences shaping those changes and their implications for both individuals and society. The Programme consisted of two substantive themes – ageing well across the life course, and ageing and its environment – with eight sub-themes: active ageing; autonomy and independence; later-life transitions; the oldest old; resources for ageing; locality, place and participation; the built and technological environment; and the global dynamics of ageing. There were 35 individual projects lasting between 18 months and 4 years, which split into two groups. On the one hand there were 11 large collaborative research projects which were multi-disciplinary, multi-site and multi-work-package in structure. On the other hand there were 24 smaller-scale projects which included a few that were not multi-disciplinary. In addition there were 10 Canadian projects which were attached to partner NDA ones and funded by the Canadian Institute on Ageing (Walker, Reference Walker2014). Full details of the projects and their findings can be found at http://www.newdynamics.group.shef.ac.uk/.
While the NDA was a particularly noteworthy investment in ageing research, because of its size and scope, it is certainly not the only programme on this topic, not even in the UK (see for example https://www.mrc.ac.uk/research/initiatives/lifelong-health-wellbeing/), nor can one research endeavour on its own change the state of knowledge. All research is incremental and cumulative, and the NDA built on existing knowledge and, in turn, has prompted further investigations. It is highlighted here because it provides an unusually comprehensive multi-disciplinary data-base and its outputs are packaged specifically for policy and lay audiences, and are easily accessed (http://www.newdynamics.group.shef.ac.uk/). The central theme of this article concerns the need for a new life-course-oriented social policy on ageing and, therefore, only the pertinent NDA findings are mentioned. These are augmented by references to pre- or parallel research, such as that on physical exercise, and by subsequent work on, for example, calorific restriction (http://mopact.group.shef.ac.uk/).
The overall picture of ageing that emerges from the mass of evidence generated by the NDA Programme and other relevant UK and international research is completely at odds with the static one that dominates both popular and policy discourses, which tends to homogenise old age and older people and restrict ‘ageing’ to the post-pension age phase of the life course. The evidence reveals instead a dynamic process of more or less continuous change in both ageing and the meaning of later life. Six dimensions of this new dynamics of ageing may be delineated. First of all, there is the longevity revolution mentioned previously. The transformational nature of this change – an average gain in life expectancy of 2 years in every 10 – has far-reaching consequences in all spheres of society and requires as yet unrealised adjustments to perceptions of what ‘old age’ is. Secondly there is improved health and functioning at older ages although caution must be exercised on this issue because of structural variation according to age, gender and social class. For example, while healthy life expectancy (HLE) at birth has risen more than life expectancy (LE) in the first decade of the 21st century, representing a compression of morbidity (ONS, 2014; Jagger, Reference Jagger2015), increases in HLE for those aged 65 and 85 are not keeping pace with improvements in LE. In other words health improvements are occurring disproportionately at younger ages. Nonetheless, as Figure 3 shows, HLE at older ages is rising even if this is not at the same rate as for LE. The social class gradients for HLE and LE, however, remain steeply in favour of the managerial and professional classes (Marmot Review Team, 2010; Marmot, Reference Marmot2015). Reduced HLE is also linked to low incomes, BME status and area deprivation (Jagger, Reference Jagger2015). Across Europe, too, material deprivation is significantly associated with HLE for both men and women (Fouweather et al., Reference Fouweather, Gillies, Wohland, Van Oyen, Nusselder, Robine, Cambios and Jagger2015).
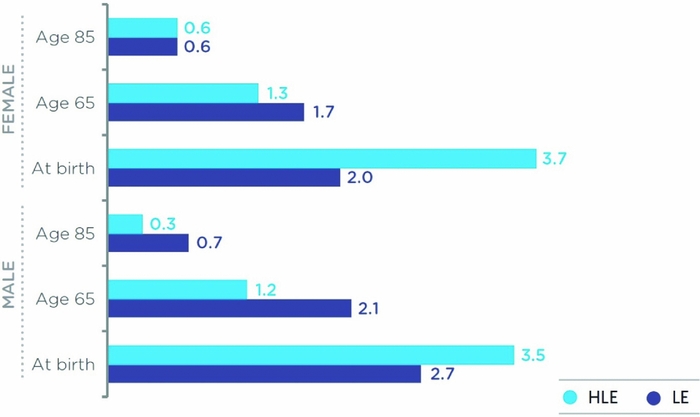
Figure 3 Life Expectancy (LE) and Healthy Life Expectancy (HLE) at different ages, UK, 2002–02 to 2009–11.
Thirdly, although poverty and low incomes are persistent in old age, in the UK pensioners are no longer the dominant group at the bottom of the income distribution (IFS, 2015; Belfield et al., Reference Belfield, Cribb, Hood and Joyce2016). Fourthly, due to a combination of policy changes (pension age increases and equalisation), financial necessity and personal preference, people are working longer (ONS, 2012). In particular the numbers working beyond state pension ages have risen significantly in recent years and this is projected to continue (ONS, 2013). Fifthly social and cultural shifts have accompanied the demographic changes, including the rise of anti-ageing procedures and therapies (Gilleard and Higgs, Reference Gilleard and Higgs2000) and the growth of the ‘silver consumer’ market in sectors such as tourism (Potratz et al., Reference Potratz, Gross, Hilbert, Walker and Naegele2009). Finally the scientific world has not been static in the face of these remarkable socio-demographic transitions. Of particular note is the now widespread acceptance of the importance of multi-disciplinarity to an understanding of ageing and later life. The NDA Programme may be seen as one substantial expression of this acceptance by UK research funders and the relevant academic disciplines, but it is by no means the only one (Hennessy and Walker, Reference Hennessy and Walker2011).
Two critical components of this new science of ageing are the combination of biological and social science insights into the ageing process and the centrality of the life course (Walker, Reference Walker2014). The bio-gerontological consensus on human ageing is that it is the result of cumulative wear and tear on the body. Summarising drastically, two sets of factors are involved and interact with each other – intrinsic (genetic) and extrinsic (environmental) – although the exact damage-causing processes are not yet fully understood (López-Otin et al., Reference López-Otin, Blasco, Partridge, Serrano and Kroemer2013; Gems and Partridge, Reference Gems and Partridge2013). For this present purpose, however, what matters most is that there is no dispute about the fact that the environmental factors far outweigh the genetic ones in this biological ageing process, probably by as much as four or five to one. For example, in studies of monozygous twins, only 20 per cent of the variance in longevity has been attributed to inherited genes (Steves et al., 2012). The consensus furthermore rejects the idea of an ‘ageing gene’, that human beings are programmed to live for a fixed period of time or to age in a certain way (Kirkwood, Reference Kirkwood2005, Reference Kirkwood2008). The key environmental adult risk factors are two-fold. On the one hand there are behavioural factors such as poor diet, tobacco use, lack of physical activity, and alcohol consumption. On the other hand there are structural risk factors such as deprivation and low socio-economic status, food poverty, excess sugar in food and work-related stress (Kirkwood and Austad, Reference Kirkwood and Austad2000). These risk factors inflict damage on the human body and mind, for example by raising blood pressure, and often result in the non-communicable diseases, or chronic conditions, that are associated with loss of function in later life, or biological ageing. These chronic conditions, sometimes referred to as the ‘geriatric giants’, include coronary heart disease (CHD), stroke and diabetes, which either truncate lives prematurely or result in disabilities requiring treatment and/or care. For example high blood pressure is a main risk factor for cardiovascular diseases, especially stroke and CHD (Downton-Hill, Nishida and James, Reference Darnton-Hill, Nishida and James2004).
The life course has been pin-pointed as central to an understanding of the causes and human consequences of ageing because none of the above biological and environmental interactions occur exclusively in old age (Figure 4). In fact they are all longer term, some life long, and have major effects before the onset of conventionally defined old age (i.e. pension ages). This is chiefly why a social policy aimed at preventing later life disability, such as active ageing, must adopt a life-course orientation (see below). Essential scientific evidence about the associations between social and environmental factors in early and mid-life and loss of functional capacity in later life has been produced by national and international analyses of longitudinal data-sets. For example, an association between childhood deprivation and high systolic blood pressure in early old age was highlighted by an analysis of the 1937/39 Boyd Orr cohort (Blane et al., Reference Blane, Higgs, Hyde and Wiggins2004).
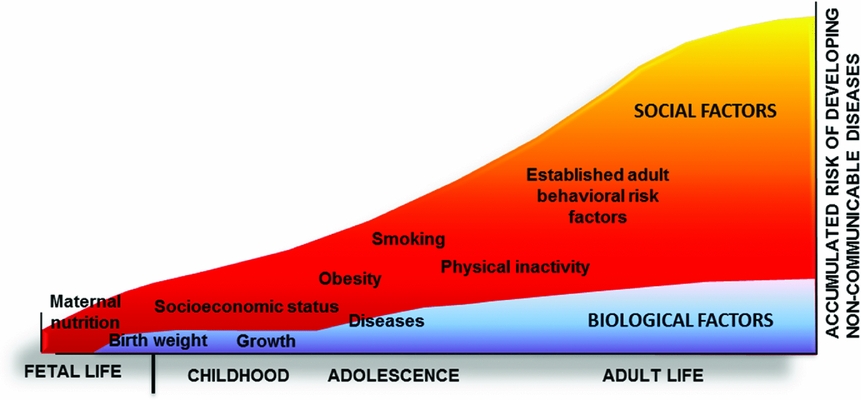
Figure 4 Cumulative risk factors for the development of non-communicable diseases across the life course
One of the most thorough investigations of the relationship between early life conditions and later life outcomes was undertaken by Kuh (Kuh et al., Reference Kuh2012) and her colleagues as part of the NDA Programme. A total of nine UK life-course cohorts were used to study the determinants of healthy ageing. Systematic reviews and meta-analysis found, on the one hand, no consistent evidence of associations between later life capability and a range of common genetic markers (the telomere maintenance gene TERT, a genotype related to athletic status ACTN3, genetic variants on the growth hormone and genetic markers of bone and joint health). On the other hand, clear associations were revealed between low socio-economic status and area deprivation in childhood and lowered levels of functioning in old age. For example, birth weight is positively related to grip strength in old age (and in adult life). Similar associations were found between living in deprived areas in mid-life and lower later-life functional capacity. Those living in deprived areas in mid-life had lower levels of physical capacity in later life. Associations were also found between childhood education and cognition in old age (Kuh et al., Reference Kuh, Cooper, Hardy, Richards and Ben-Shlomo2014a).
There is robust evidence that those in better socio-economic circumstances in childhood as well as adulthood have better [physical] capability at older ages. (Kuh et al., Reference Kuh2012: 1)
In scientific terms this research suggests that socio-economic factors leave biological imprints on later-life physical development. One of the key policy findings from this research is that action to reduce deprivation in early and mid-life is likely to improve health and functional capacity in old age. Furthermore policies aimed at improving both living standards and early years education are likely to increase later-life cognition. In a nutshell, social policy is far more important than genetics in determining the nature of old age and the extent of inequalities in its experience. It is the dominant influence among the environmental factors driving ageing and, therefore, it holds the promise of an alternative scenario in which the ageing process is modified.
Ageism and structural lag
Even this very brief outline of the far-reaching policy implications of a sample of recent ageing research should be sufficient to suggest the possibility for social action aimed at limiting the scale of age-associated chronic conditions and, thereby, improving the prospects for both ageing individuals and the exchequer. So, why is the policy world apparently impervious to such evidence? Two main influences appear to be at work. Firstly, there is deeply ingrained ageism, which continuously bedevils attempts to discuss this issue rationally (McEwan, Reference McEwan1990; Macnicol, Reference Macnicol2006). This dismal reduction holds that ageing is old age and, usually by definition, this represents a ‘burden’ on society. Some scientific legitimacy is afforded to this forlorn and hopeless scenario by so-called ‘dependency ratios’, which arbitrarily allocate age groups to the categories of the productive and dependent, regardless of the actual contributions being made by them (Walker, Reference Walker and Taylor1990a). The relentless amplification of this burden narrative by the mass media, especially the print media, hardly requires mention. Perhaps because of media credulity there is no shortage of commentators wanting to contribute to this narrative (Wallace, Reference Wallace2001; Hawker, Reference Hawker2010; Willets, Reference Willets2010). In this context it is difficult to debate the implications of population ageing in an open and dispassionate way. This is despite a long line of research which has demolished the burden of ageing thesis by, for example, exposing its failure to acknowledge the formal and informal contributions of older people (Walker, 1980). Also exposed has been the vacuity of the prediction of generational war over resources that surfaces and re-surfaces with great regularity whenever the ageing issue hits the headlines (Macnicol, Reference Macnicol2006; Walker, Reference Walker and Taylor1990a).
Secondly there is the problem of ‘structural lag’. More than two decades ago the distinguished sociologist of ageing, Matilda White Riley, commented on the failure of social structures, roles and norms to keep pace with demographic changes (Riley, Reference Riley1994; Riley et al., Reference Riley, Kahn and Foner1994). This lag is essentially passive institutional inertia, or active resistance to change, on the part of bureaucracies and bureau-professionals. In the context of very rapid socio-demographic change, such as the longevity revolution, a major mismatch develops between existing policies and institutional assumptions and structures, and those that would be more appropriate or ‘optimal’ in the new circumstances. The failure of many employers and labour market institutions to adapt to workforce ageing is an example of this structural lag (Walker, Reference Walker1997; Taylor and Walker, Reference Taylor and Walker1998). In practice, and in the absence of major oppositional vested interests, it seems to take institutions and policies at least 20 years to catch-up with major socio-demographic changes, so the absence of a concerted strategy on ageing should, perhaps, not be surprising. The first barrier to change, age discrimination, may also contribute to the structural lag. The short-term electoral cycle mind-set of British governments is also likely to militate against the long-term perspective required by the ageing challenge. This is especially the case when the proposed actions require immediate additional resources to invest in future health improvements (Coote, Reference Coote2015).
As the social policy profession is an integral part of the national policy community, consideration of the operation of structural lag may require a little self-examination: what have we done to mitigate its effects? Not enough I think, and some of our approaches and techniques may actually reinforce it. For example, our projections, such as on the future need for long-term care, are commonly merely extrapolations which follow the tenet of neo-classical economics ceteris paribus (other things being equal). But, as demonstrated above, this assumption is not tenable in the context of rapid socio-demographic transition. Another example is the social policy profession's tendency to favour specific, sometime narrow, age group specialisms: children, older people and so on. A glance at any introductory text on social policy shows that this habit is still ingrained. There may indeed be a good case for it but where is the overall focus on ageing? The consequences of this professional neglect are, first, social policy has not occupied the central role it should have in responding to demographic change and, second, as intimated, there is no social policy on ageing, one consequence of which is the absence of a strategic response to the challenges presented by population ageing.
Despite these potential barriers to social policy action, the failure is still surprising. The sheer scale of chronic diseases associated primarily with later life appears to constitute an imperative which should prompt urgent policy initiatives. Nearly half (46 per cent) of the so-called global ‘burden of disease’ consists of these chronic conditions and this proportion is projected to rise to 57 per cent by 2020 (Haagsma et al., Reference Haagsma2015; Murray and Lopez, 1996; WHO, 2002a). As well as Exchequer costs there are huge personal costs for those affected unnecessarily, or unnecessarily severely, and their carers. As noted these costs fall very unevenly on the population, for example in terms of social class, income, gender and geographical location. As well as the ageist assumption that later life and disability go hand in hand, there is a sense of hopelessness about the inevitable downward course of ageing. Even where examples abound of fit and healthy nonagenarians, such as David Attenborough and Queen Elizabeth II, this is attributed popularly to luck rather than wealth or class. This commonly translates into stoicism among older people such as ‘what can you expect at my age?’.
Towards a social policy on ageing
Evidence from the major NDA Programme of research alongside other UK and international evidence suggests that it is possible to modify the ageing process at earlier stages of the life course so that the outcomes in old age are less restricting both physically and mentally. In other words, ageing is inevitable but also malleable. In policy terms, measures aimed at modifying the impact of various risk factors and, thereby, reducing the prevalence and severity of chronic conditions, have a high likelihood of extending healthy life expectancy. What sort of measures are required? In the short term various initiatives might be taken to attempt to mitigate the growth of later-life disability and encourage more healthy lifestyles. For example higher taxes could be levied on tobacco and alcohol and new taxes introduced on saturated fat in foods and sugar in soft drinks and confectionary. The relatively modest levy on the sugar content of soft drinks proposed by the UK Government for introduction in April 2018 could reduce obesity among adults and children by 144,000 per year and prevent 19,000 cases of obesity (Briggs et al., Reference Briggs, Mytton, Kehlbacher, Tiffin, Elhussein and Rayner2016). Smoking-related disabilities are estimated to drive £760 million p.a. in social care costs alone (All Party Parliamentary Group on Smoking and Health, 2017) and a levy on tobacco manufacturers to fund measures to reduce smoking prevalence is needed urgently, especially as government cuts to local authority spending are leading to the curtailment of smoking cessation services.
A national programme of physical exercise is urgently required and would be expected to have a significant impact providing that it was tailored to specific populations (see below). For example, the active have a 33–50 per cent lower risk of developing Type 2 diabetes than the inactive; and the moderately active have a 20 per cent lower risk of stroke incidence than the inactive (Chief Medical Officer, 2004, 2014; Kuh et al., Reference Kuh, Karunananthan, Bergma and Cooper2014b). The physically active are generally healthier and live longer than the sedentary. Prolonged periods of inactivity are associated with heightened risk of cardiovascular disease, cancer and diabetes (Pate et al., Reference Pate1995). There is also evidence that physical exercise has a beneficial effect on cognition, as well as other protective effects on health (Lees and Hopkins, Reference Lees and Hopkins2013). Put differently, major physical and mental health risks and substantial health and social care costs are the products of inactivity. Despite the fact that an increasing number of countries have national physical activity plans there is no sign of a global improvement in activity levels (The Lancet, 2016). Critically, regular activity can diminish the increased mortality risks associated with prolonged sitting.
Another example is the recent evidence on the beneficial effects of long-term calorie restriction, with adequate intake of nutrients, which decreases the risk of developing most age-associated chronic conditions, including Type-2 diabetes, hypertension, cardiovascular diseases and cancer (Fontana and Partridge, Reference Fontana and Partridge2015). Indeed significant health benefits flow from even a five per cent weight loss by obese people resulting in lowered risks for diabetes and heart disease (Magkos et al., Reference Magkos2016). A further example is the need for health professionals to understand the effects of ageing on the body's immune system, especially the reduction in the number of antibody-producing cells in the bone marrow (Pritz et al., Reference Pritz, Lair, Ban, Keller, Weinberger, Krismer and Grubeck-Loebenstein2015). This means that protection from infectious diseases, which cause an estimated one-third of mortality above the age of 65, is less than at younger ages and, as a consequence, older people require more frequent vaccination. A final example is the operation of mental stimulation to not only improve brain function but also provide protection from cognitive decline – in a similar way to physical exercise helping to prevent loss of bone and muscle mass (Bertozzi et al., Reference Bertozzi, Tosti and Fontana2016).
Practical questions abound, of course, about any such programmes aimed at physical activity, weight loss and cognitive stimulation. To be effective, such initiatives must be well-funded and sponsored nationally. Space precludes too much detail but, for example, a programme on physical activity could comprise national activity guidelines, leave the car at home days, more cycle lanes, gym or swimming bath ‘social prescriptions’ from GPs, multi-generational park runs and so on. As with the longer term comprehensive strategy set out below, there is a risk of stigma being associated with non-participation. This can be minimised by setting the inclusion bar low and not applying any formal sanctions. Regular television and social media exposure would also assist in gaining wide acceptance.
In the longer term it is essential to match the scale of the ageing challenge with an ambitious and comprehensive response. The leading global contender for this role is the idea of ‘active ageing’ (WHO, 2002, 2005a). Although the concept of active ageing is contested and often expanded to ‘active and healthy ageing’ by international agencies (EU, 2012; WHO, 2015a), it remains the most widely accepted strategy on ageing (Walker and Maltby, Reference Walker and Maltby2012) and was integral to the 2002 Madrid International Plan of Action on Ageing (UN, 2002). According to the WHO (2002: 3):
Active ageing is the process of optimising opportunities for health, participation and security in order to enhance quality of life as people age.
This pivotal definition may be mildly criticised for placing too great an emphasis on health and not being sufficiently policy oriented. To counter these objections, while retaining the key life-course focus, an alternative policy-oriented definition has been proffered:
Active ageing should be a comprehensive strategy to maximise participation and well-being as people age. It should operate simultaneously at the individual (lifestyle), organisational (management) and societal (policy) levels and at all stages of life course (Walker, Reference Walker2009: 90).
The life-course focus at the core of the active ageing concept is often overlooked in practice and old age only is spotlighted. In addition, seven fundamental principles support the implementation of this internationally policy-oriented definition of active ageing. First ‘active’ should embrace all activities that contribute to both physical and mental wellbeing. This is necessary to counteract the common stereotypes of hyper-active pensioners as the epitome of active aging. Equally important are activities intended to maintain or regain mental capacity – such as the ‘five ways to wellbeing’ (Government Office for Science, 2008; NEF, 2008). Second, the life-course perspective is essential to recognise that chronic conditions and capabilities in later life are invariably the outcomes of earlier life social and economic status and exposure to risk factors. To reiterate, the evidence from cohort meta-analyses is that childhood circumstances greatly influence the prospects for active ageing in later life (Kuh et al., Reference Kuh, Karunananthan, Bergma and Cooper2014b). Third, a preventative approach is crucial. Thus the explicit goal of a social policy on ageing should be to prevent as many as possible of the chronic conditions that can blight or curtail later life. In this regard it is vital to address not only the low priority allocated to prevention in health and social care but also the neglect of secondary interventions among those already suffering from ill-health or disability (Pope and Tarlov, Reference Pope and Tarlov1991). Fourth, a comprehensive strategy on active ageing must employ all possible policy levers, upstream primary prevention and downstream secondary prevention and rehabilitation as well as spanning all Whitehall and local government departments. Fifth, active ageing should not exclude any age group, as the common stereotype does with the very old and frail. In fact there is evidence that even minor exercises can improve both physical functioning and mental wellbeing (Grönstedt et al., Reference Grönstedt, Fraudin, Berglund and Helbostad2013). Sixth, in public health terms, top-down exhortations or abstract codes of behaviour are unlikely to work for the many. Instead what is required is an empowerment approach, which seeks to engage different groups of citizens in a dialogue about ageing and the avoidable risk factors, as a counterpart to preventative or remedial actions. This is not easy or straightforward, especially in view of the vested interests involved, and is a non-starter without the political will to get it underway and support it. Finally it is essential to account for inequality and cultural diversity. For example gender differences in the application of active ageing are substantial (Foster and Walker, Reference Foster and Walker2013). Furthermore some forms of activity may be less acceptable or prohibited in certain cultures and so flexibility in implementation is essential.
The transformative nature of what is being proposed here, as well as the inadequacy of the present life-course-segmented policy approach, can be illustrated by imagining some of the key periodised components of an active ageing strategy (see Figure 4):
-
• Foetal health: nutrition, antenatal care, prevention of substance misuse, maternity grants/leave, paternity leave.
-
• Early years: poverty prevention, universal nursery education, sure start activities in deprived areas, providing nursery education on ageing and health.
-
• Childhood and adolescence: maximising life chances for the many, preparation for life-long learning, understanding ageing and ageism, education on healthy diets and wellbeing.
-
• Mid-life: continuous education/training, age management techniques to reduce the potentially damaging aspects of work on health and well-being, active engagement in community life, guidance and support on healthy consumption, flexible retirement.
-
• Later life: supports to maintain health/autonomy, engaging in new activities, continuous learning, taking up opportunities for community involvement, resisting the narrative of decline and dependency e.g. by using technology, primary care geared to prevention of chronic conditions eg. by means of specialist outreach workers and volunteers.
The underlying objective of this strategy can be demonstrated with reference to a typical life course (Figure 5). Physical activity peaks in early adult life and then declines during middle and later life, at vastly different rates due mainly to variable exposure to risk factors; thus the variations in capacity within cohorts are larger than those between cohorts (Kirkwood, Reference Kirkwood2008). The cumulative impact of physical or mental injuries and/or chronic conditions is that a person's functional capacity declines until it crosses the disability threshold. The idea of the active ageing strategy is to attempt to slow or prevent the decline in functional capacity and thereby enable people to enjoy disability-free extended lives for as long as possible. Figure 5 shows the path of physical capacity but some aspects of cognitive ability also follow a similar one.
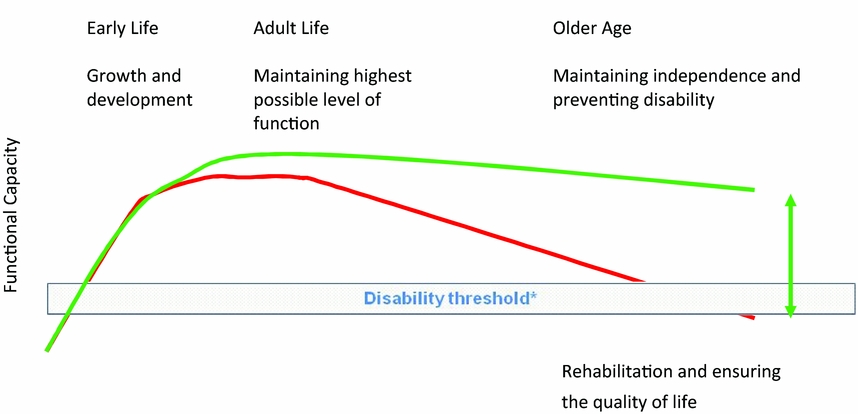
Figure 5 Functional capacity and age
Such a transformation from segmented age-group specialisms to an overall life-course approach would, of course, not be easy. Simply contemplating the seismic shift in health services, from acute sickness to prevention and rehabilitation, is sufficient to convey the scale and depth of the necessary changes. The alternative, however, is to proceed as now and tacitly accept the present extent of preventable life-restricting conditions and their human injuries and social and economic costs.
Some idea of the challenges and potential cost savings can be gleaned from Figure 6 showing the projected costs of care to 2045. Such projections are a familiar feature of social care policy and, when they are suitably steep, they invariable get picked up by the media and translated into banner headlines conveying unwarranted certainty, such as: ‘care costs to quadruple’. A social policy based on active ageing across the life course is required to ensure that these sorts of projections are not, in fact, realised. Thus, everyone who will be aged 85 or 90 in 2045 is alive now and in their mid-late 50s. The current policy approach is to do nothing or, at best, very little, to prevent disabling conditions from developing at earlier stages of the life course. Any action to mitigate the incidence of such conditions is largely a matter for individuals. Thus, in 2015–16, adult social services devoted just 6.6 per cent of their budget to prevention and this had been cut by 6 per cent compared to 2014–15 (ADASS, 2015). Imagine, however, if society as a whole prioritised sustaining activity and well-being through middle-age and into old age; the lives of millions of people could be transformed. There is a reasonable expectation, too, of accompanying cost savings or, at the very least, expenditure being postponed until late old age.
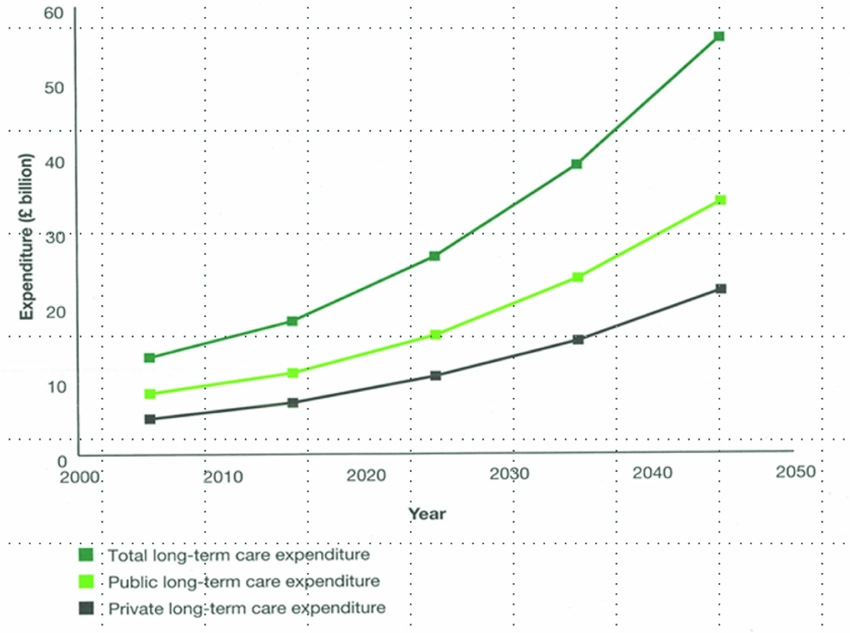
Figure 6 Projected long-term care costs, England.
If a strategy for active ageing promises such significant individual and social benefits, why have governments not seized upon it with enthusiasm? Some of the reasons have been touched on already, including the short-term political horizon and inherent ageism. In addition there are the various vested interests which prosper from the present status quo. These range from politicians and journalists, who so readily employ the rhetoric of the burden of old age, to commercial companies that make profits from unhealthy diets and lifestyles. The global obesity epidemic signals the power of these vested interests as well as the behavioural forces presently pulling in the opposite direction to the one proposed here (WHO, 2015b). Thus three-quarters of middle aged men and three-fifths of women are overweight or obese (Public Health England, 2016) as are two-fifths of children in England's most deprived areas and one-quarter in the most affluent ones (Royal College of Paediatrics and Child Health, 2017). Moreover it is predicted that, by 2025, one-third of all adults in Britain will be obese (Ezzati et al., Reference Ezzati2016) and, in 80 per cent of cases, Type 2 diabetes is linked to obesity and inactivity (National Cardiovascular Intelligence Network, 2016).
Perhaps most injurious to the social policy strategy proposed here, however, is the UK's presently dominant neo-liberal political-economic anti-welfare state paradigm that priorities individual entrepreneurial freedom, private property rights, free markets, and free trade (Harvey, Reference Harvey2005). How so? On the one hand neo-liberal-inspired austerity politics is making matters much worse, for example by increasing poverty and inequality (O'Hara, Reference O'Hara2014; Foster et al., Reference Foster, Haux, Brenton and Deeming2014). For example, the All Party Parliamentary Group on Health in All Policies (APPG, 2016) inquiry into child poverty and health concluded that the Welfare Reform and Work Bill 2015–16 would increase child poverty and directly worsen social, emotional and cognitive outcomes. In other words UK austerity policies since 2010 have deliberately exposed, rather than protected, some of the poorest groups while preserving those in the middle and upper sections of the income distribution (although not the very highest earners) (Hood and Johnson, Reference Hood and Johnson2016). On the other hand, the major barrier confronting a social policy on active ageing is that it would require a collective approach intended to mobilise a very wide range of societal resources and underpinned by a commitment to public welfare. This collectivism and belief in the public good is seriously problematic for fundamentalist neo-liberals, for whom individualism and commercialism are paramount (Harvey, Reference Harvey2005). Of course neo-liberalism has been the driving force behind global economic policies for more than two decades but its form and intensity of application is more severe in some countries than others. Thus the UK has taken a stronger anti-collectivist policy approach than some other Western European countries (Esping-Andersen, Reference Esping-Andersen1996).
This antagonism between neo-liberalism and collective public action was demonstrated extensively by 1980s Thatcherism (Farrall and Hay, Reference Farrall and Hay2014; Walker, Reference Walker1990b). Subsequent governments have also not introduced far-reaching public health reforms. This is presumably because the prevailing neo-liberal consensus, weak or strong depending on political leadership, contributes to what is at best a reluctance to tackle powerful vested interests in the business community, for instance with regard to the contribution of sugar to childhood obesity (Stuckler and Siegel, Reference Stuckler and Siegel2011). Thus, it is not that successive governments have openly opposed a life-course approach to ageing but, rather, if they have even contemplated it, the ideological and/or practical challenges of doing so have proved too daunting. When the power of major corporations that benefit from the status quo is factored into this mix the sheer scale of the challenge can be appreciated. Chronic diseases generate profits from expensive pharmaceutical and genetic medicines, as do the unhealthy food, tobacco and alcohol that contribute to many of them. The preventative policy orientation argued for here threatens those profits. As Stuckler and Siegel (Reference Stuckler and Siegel2011) argue, this is not a conspiracy; those corporations openly declare their opposition to the idea of any restrictions on their businesses.
As well as these structural barriers to radical change it should not be pretended that the concept of active ageing itself is problem-free. For instance there are ever present dangers of both coercion and stigmatisation of the inactive associated with it. Such an outcome would reflect a caricature of later-life activity, the heroic marathon-running pensioner, rather than the concept proposed herein which focuses on the whole life course and incudes mental as well as physical activity. There is also the constant association of ‘ageing’ with old age in popular discourses and, therefore, the risk that younger people will be alienated from a social policy on ageing. As mentioned previously, there is also the problem that activity is taken to mean only physical activity. Although it is important to recognise these inherent problems none of them need be insurmountable if the concept is defined comprehensively and the strategy is applied sensitively.
Conclusion
This article has advanced the case for a radical new strategy on ageing and argued that without it the scale of unnecessary disability will continue to grow unabated. It has drawn on the latest UK and international scientific evidence, which is overwhelming on several essential points such as the beneficial effects of physical exercise and calorie restriction, and continues to mount. This evidence demands an emphasis on the whole life course instead of only the later life segment of it. To summarise the key points. First, ageing is inevitable but it is also malleable. Second, while various risk factors occur at earlier stages of the life course, the resulting chronic conditions usually emerge in later life (Darnton-Hill et al., Reference Darnton-Hill, Nishida and James2004). Third, a new policy approach that is effective in changing social institutions and individual behaviour to reduce risks will have absolute benefits for both ageing people and populations. Fourth, there is a public health and moral imperative to maximise health, well-being and quality of life by, at best, avoiding, or at least delaying, preventable disabilities. Fifth, in political terms, these desirable outcomes depend on collective action. The lack of action is not due to scientific or technical barriers but political ones. Sixth, although the case is advanced in terms of UK policy and practice, it has global relevance. Finally, social policy is centrally located in this account, on the one hand, as one of the causes of age-associated chronic conditions and their unequal distribution and, on the other, as the best hope for their prevention.
Acknowledgments
This article started out as a plenary presentation to the 2014 SPA annual conference. I am grateful to participants for their helpful feedback and especially to Adrian Sinfield for his encouragement to publish it. The article draws on the New Dynamics of Ageing Programme and Mobilising the Potential of Active Ageing in Europe project. I am grateful to the ESRC and European Commission for funding (RES-339-34-3001 and 320333). Thanks also to Carmen Giefing-Kroell, Dan Holman and Sarah Howson for their help in the production of this article.