Introduction
During pregnancy, the imperative to stop smoking becomes more urgent due to toxic products of tobacco being highly detrimental to both mother and child (Hofhuis, de Jongste, & Merkus, Reference Hofhuis, de Jongste and Merkus2003). Smoking is the most important remediable risk factor for poor perinatal outcomes for babies and can have long-reaching effects into adulthood (Hofhuis et al., Reference Hofhuis, de Jongste and Merkus2003). Public health messages around smoking in pregnancy mostly take a foetal-centric approach, based on the assumption that if women know about harms for their baby, then they will be automatically motivated to stop smoking (Wigginton & Lafrance, Reference Wigginton and Lafrance2014). However, some pregnant women experience considerable stigma from continuing to smoke (Wigginton & Lee, Reference Wigginton and Lee2013).
Tobacco smoking is the major contributor to the gap in health equality experienced by Aboriginal people in Australia (Vos, Barker, Begg, Stanley, & Lopez, Reference Vos, Barker, Begg, Stanley and Lopez2009). The perception of health risks from smoking for Aboriginal women need to be understood within the context of multiple disadvantages and intergenerational trauma that Aboriginal women may experience. These factors include colonisation, dispossession, racism, and forced removal of children (Brady, Reference Brady2002; Thomas, Briggs, Anderson, & Cunningham, Reference Thomas, Briggs, Anderson and Cunningham2008). Wide-reaching impacts include the legacy of an increased prevalence of tobacco smoking (Brady, Reference Brady2002); currently, 43% are among Aboriginal pregnant women (Australian Institute of Health & Welfare, 2018).
Aboriginal people are more likely to want to quit smoking than the general population but are less likely to succeed (Nicholson et al., Reference Nicholson, Borland, Davey, Stevens and Thomas2015). Sociocultural experiences contribute to the relative difficulty of Aboriginal women quitting smoking in pregnancy (Gould, Bittoun, & Clarke, Reference Gould, Bittoun and Clarke2015a). Challenges include social norms of smoking, family, partner and peer influences, limited knowledge about the health effects, cravings and stress when trying to stop or reduce smoking, and low awareness about and use of pharmacotherapy (Bovill et al., Reference Bovill, Gruppetta, Cadet-James, Clarke, Bonevski and Gould2018; Gould, Bovill, Cadet-James, Clarke, & Bonevski, Reference Gould, Bovill, Cadet-James, Clarke and Bonevski2016a; Gould, Munn, Watters, McEwen, & Clough, Reference Gould, Munn, Watters, McEwen and Clough2013b). On the positive side, significant life events are highly salient and predictors for Aboriginal people when quitting smoking (Bond, Brough, Spurling, & Hayman, Reference Bond, Brough, Spurling and Hayman2012). Pregnancy is an opportunity to encourage positive change where a sense of a ‘protector role’ is expressed by Aboriginal women (Gould et al., Reference Gould, Munn, Avuri, Hoff, Cadet-James, McEwen and Clough2013a).
Although smoking in pregnancy and passive smoking are acknowledged by Aboriginal women as harmful for babies and children, responses to existing anti-tobacco messages can be unpredictable, as many Aboriginal women find messages too threatening and not in accordance with their lived experience (Gould et al., Reference Gould, Munn, Avuri, Hoff, Cadet-James, McEwen and Clough2013a). The harms for the baby in utero may be less tangible, with inaccurate information often portrayed both in the media and by health providers (Gould, Cadet-James, & Clough, Reference Gould, Cadet-James and Clough2016b). Health providers deliver inconsistent messages: while many may advise quitting, some recommend cutting down (Bovill et al., Reference Bovill, Gruppetta, Cadet-James, Clarke, Bonevski and Gould2018). In an international review, potential risks of abruptly quitting smoking were reported by women and health providers: these included a perception that quitting could be too stressful for the mother and potentially harmful for a baby (Kumar et al., Reference Kumar, Stevenson, Jobling, Gribbins, Bar-Zeev and Gould2019).
Women's responses to health messages while pregnant may depend on their relative perceptions of the threat from smoking and their perceived efficacy for quitting (Gould, Bovill, Chiu, Bonevski, & Oldmeadow, Reference Gould, Bovill, Chiu, Bonevski and Oldmeadow2017). The Extended Parallel Process Model (EPPM) predicts that according to various combinations of high or low threat and high and low efficacy, individuals respond differently to health messages (Figure 1) (Witte, Reference Witte1994). When a threat is perceived as high, people conduct an efficacy evaluation. Those with high threat perceptions combined with high efficacy perceptions are more likely to act consistently with reducing the threat (called danger control) for example, by attempting to quit smoking. Conversely, those with low efficacy perceptions are more likely to exhibit fear control and avoid or deny the message, thus continue smoking.
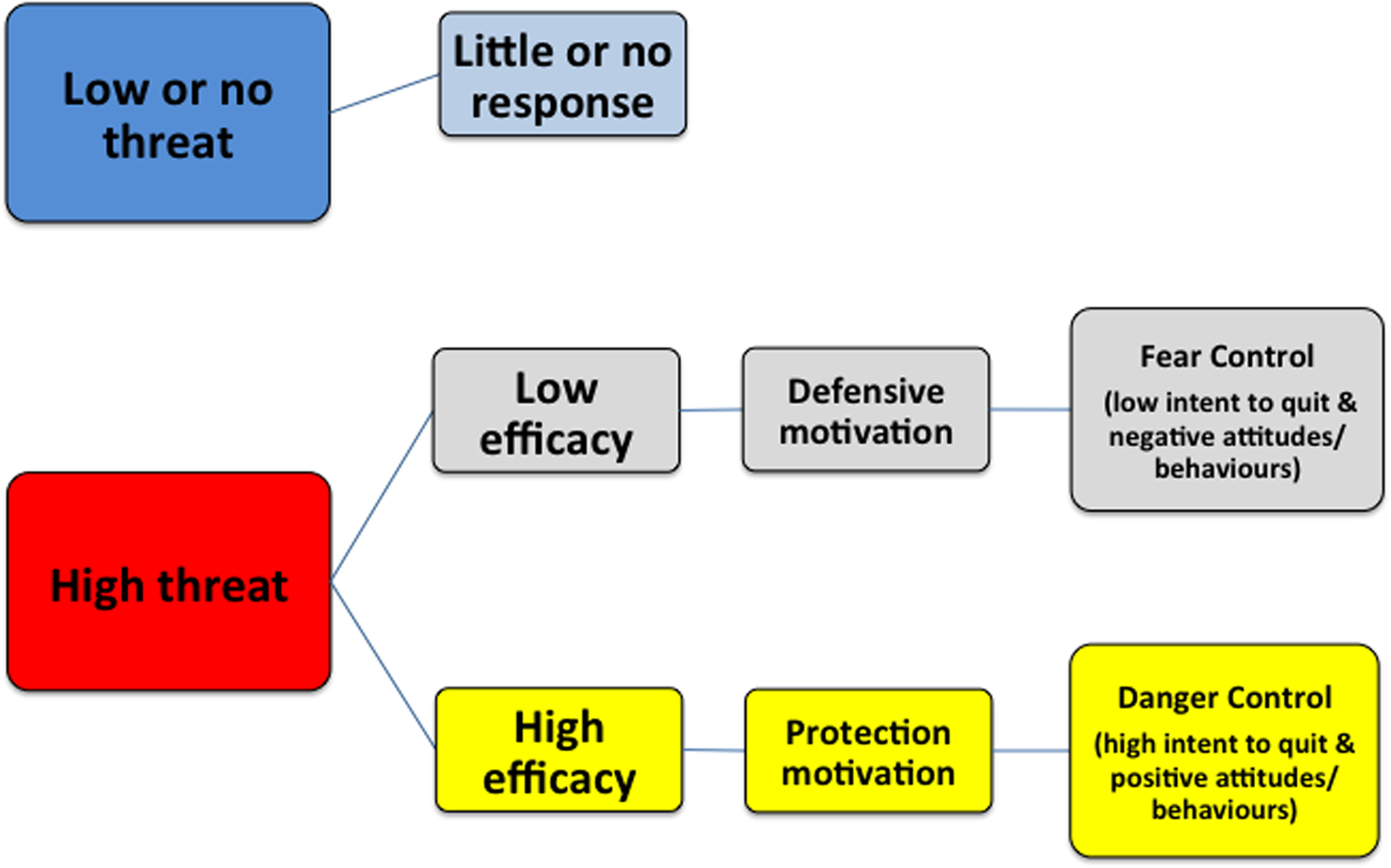
Fig. 1. The extended parallel process model and expected responses to threat and efficacy levels (reproduced with permissions from authors) (Gould et al., Reference Gould, Watt, Cadet-James and Clough2015b).
The Risk Behaviour Diagnosis (RBD) Scale, based on the EPPM, was initially developed to measure responses to a sexual health promotion campaign (Witte, Reference Witte1994; Witte, Meyer, & Martell, Reference Witte, Meyer and Martell2001). The RBD Scale is a valid and reliable measure of the responses to health messaging for quitting smoking among Aboriginal smokers of reproductive age (Gould, Watt, McEwen, Cadet-James, & Clough, Reference Gould, Watt, McEwen, Cadet-James and Clough2014). Four subscales include measures of perceived threat (susceptibility to and severity of smoking risks) and perceived efficacy (response efficacy and self-efficacy for quitting) (Gould, Watt, Cadet-James, & Clough, Reference Gould, Watt, Cadet-James and Clough2015b). The RBD Scale could have diagnostic potential to tailor health messages to respective levels of threat and efficacy perceptions and prevent messages potentially backfiring (Witte et al., Reference Witte, Meyer and Martell2001). Smokers with high threat-high efficacy perceptions may tolerate a threat-based message, but those with high threat-low efficacy perceptions are better off receiving an efficacy only message, to prevent them developing a fear control response (e.g., by denying or refuting the message or importance of quitting smoking).
In a small-scale study, Aboriginal women completing the RBD Scale, who were pregnant or recently pregnant, appeared to respond similarly to a more general cohort of Aboriginal men and women of reproductive age (Gould et al., Reference Gould, Watt, Cadet-James and Clough2015b). However, the RBD Scale has not been used serially to explore how Aboriginal smokers change over time, or with exposure to smoking cessation interventions.
This study aimed to explore pregnant Aboriginal women's responses to an adapted RBD Scale, over several time points during pregnancy. This pilot data may enable us at a future date to tailor an intervention to Aboriginal pregnant women who smoke. This study was conducted as a nested study with women who were participants recruited to a trial of a culturally responsive intervention called Indigenous Counselling and Nicotine (ICAN) QUIT in Pregnancy (Bar-Zeev et al., Reference Bar-Zeev, Bonevski, Bovill, Gruppetta, Oldmeadow, Palazzi and Gould2017; Gould et al., Reference Gould, Bovill, Pollock, Bonevski, Gruppetta, Atkins and Bar-Zeev2018).
Methods
Participants and setting
N = 22 pregnant women were recruited to ICAN QUIT in Pregnancy (20 were Aboriginal, and two were non-Aboriginal women pregnant with Aboriginal babies). ICAN QUIT in Pregnancy was a step-wedge trial in six Aboriginal Community Controlled Health Services (ACCHS) in three Australian states from November 2016 to September 2017. The trial protocol has been published (Bar-Zeev et al., Reference Bar-Zeev, Bonevski, Bovill, Gruppetta, Oldmeadow, Palazzi and Gould2017). The feasibility and acceptability outcomes as the primary aims of the study, and outcomes for the secondary aims (health provider demographics and outcomes, and women's demographics, nicotine dependence, medication use and smoking cessation outcomes) were reported elsewhere (Bar-Zeev et al., Reference Bar-Zeev, Bovill, Bonevski, Gruppetta, Oldmeadow, Palazzi and Gould2019; Bovill et al., Reference Bovill, Bar-Zeev, Bonevski, Gruppetta, Oldmeadow, Hall and Gould2020; Gould et al., Reference Gould, Bovill, Pollock, Bonevski, Gruppetta, Atkins and Bar-Zeev2018).
In a step-wedge design, ACCHS were randomised in three pairs to commence the study staggered by monthly intervals. Eligible ACCHS were required to have at least one general practitioner (GP), consult with Aboriginal and/or Torres Strait Islander pregnant women, have contact with 20 pregnant women who smoke per year, and recruit and follow-up patients for the study. In a pre-intervention phase, services could recruit women, conduct the surveys, and perform usual care. This usual care was followed by a month in which health provider training was planned, and followed by a post-training phase when women continued to be recruited, and both new recruits and existing participants were followed up (see Figure 2).

Fig. 2. Schema of Step-Wedge Cluster Randomised Design for ICAN QUIT in Pregnancy (reproduced with permissions from authors) (Bar-Zeev et al., Reference Bar-Zeev, Bonevski, Bovill, Gruppetta, Oldmeadow, Palazzi and Gould2017).
Eligible pregnant women were current smokers, up to or including 28-weeks' gestation, aged 16 years or over, Aboriginal or expecting an Aboriginal baby. Women did not need to intend to quit smoking to be in the study. A trained research facilitator recruited participants at each service ACCHS. The research facilitator was an existing staff member nominated by the service, who may or may not be also a health professional. The research facilitator's role was to engage with women, gain informed consent, administer surveys (including the RBD Scale as a nested study), take expired carbon monoxide (CO) readings with a hand-held Bedfont piCO baby meter, sensitively explain the CO results to the woman, and follow up participants.
A 56-item survey was administered at baseline which included the 20-item RBD Scale previously validated for face and content validity, cultural appropriateness, and feasibility and reliability among Aboriginal men and women of reproductive age and further explored for usability in pregnant Aboriginal women (supplementary file 1) (Gould et al., Reference Gould, Watt, Cadet-James and Clough2015b, Reference Gould, Bovill, Chiu, Bonevski and Oldmeadow2017). The survey included questions about levels of agreement with perceived susceptibility to threat and severity of the threat, and perceived response efficacy and self-efficacy for quitting. The threat questions were orientated towards the risk of smoking for a baby's health. Scales for fear control responses included statements about denial or avoidance of risks from smoking, and for protection responses statements included the desirability of pregnant women, partners and the adult Aboriginal community not to smoke tobacco. Additional questions included a 5-item scale for danger control (statements on intentions to quit or seeking help to quit), and a smoking characteristics survey. See supplementary file for all questions. Follow up surveys included additional questions on quit attempts, and smoking abstinence, administered at 4-weeks and 12-weeks post-baseline.
All women at recruitment and the 4-week and 12-week time points had their breath tested by the research facilitator for CO to confirm smoking or abstinence. Scores of ⩽6 parts per million signify abstinence from smoking (Maclaren et al., Reference Maclaren, Conigrave, Robertson, Ivers, Eades and Clough2010).
The intervention has been previously described in the protocol, but in brief comprised: (1) live interactive webinar training for all health providers who consult with pregnant women at the ACCHS for confirmation of pregnancy, antenatal care and/or routine care; these included GPs, midwives, Aboriginal Health Workers and other allied health professionals, (2) a treatment manual, a Flipchart to guide the consultation, a mouse pad with a treatment algorithm design, (3) booklets as an educational and motivational resource for the women, (4) a CO meter, (5) oral Nicotine Replacement Therapy (NRT) supplies to dispense on site. The training delivered to the health providers emphasised the need for supportive messages to be delivered during the consultation to build women's self-efficacy and response efficacy for quitting smoking. Similarly, these positive messages were included in the side of the Flipchart visible to the patients and the women's booklet. However, the importance of quitting completely in pregnancy was emphasised rather than cutting down. Two augmented reality videos in the booklet for pregnant women showed a female Aboriginal Obstetrician discussing the acute and chronic health risks for the baby and addressed myths about smoking and quitting during pregnancy in a non-confrontational style. The messages in the resources provided to the pregnant women participants were not individually tailored. Other videos in the booklet gave factual information on how to take NRT delivered by a Torres Strait Islander GP. Furthermore, peer-delivered videos were included about the common triggers for smoking and how to make a home smoke-free.
Analysis
All analyses were undertaken in SAS software version 9.4 (SAS Institute, Cary, North Carolina, USA) for this nested study. The outcomes and demographics were compared between collection time points using descriptive statistics. Means and medians values for the scales were calculated. The outcomes of the RBD subscales were cut at the median value. Participants that score higher or equal to the median were labelled as having a high score, and those that scored lower than the median were labelled as low. Thus, the subscales were recategorised into the following variables: total perceived threat (high vs low); total perceived efficacy (high vs low); protection responses (high vs low); fear control responses (high vs low); danger control responses (intentions to quit: high vs low).
A discriminating value is the difference between the total perceived efficacy scores and the total perceived threat scores (Witte et al., Reference Witte, Meyer and Martell2001). The EPPM theory proposes that by calculating the discriminating value one can ascertain whether the perceived threat is equal to or higher than perceived efficacy: if so, then a person may be in fear control rather than danger control. A discriminating value was calculated from the formula (sum of perceived efficacy) minus (sum of perceived threat) equals discriminating value, then categorised into positive (>0) or negative (<0) (Witte et al., Reference Witte, Meyer and Martell2001). Linear mixed modelling was used to assess the changes over time for the main outcomes of interest: total perceived efficacy, total perceived threat, total fear control and total protection responses. A compound symmetry structure was used to model the covariance between time points. Conditional means were reported to show the mean value of the outcomes at each time point, accounting for the inter-person correlation.
Taking into consideration the date of site training and therefore, the commencement of the intervention, a ‘pre’ and ‘post’ classification was assigned to each survey entry. Where individuals might have had multiple surveys collected before or after the site training, in these cases, the average score between their surveys was recorded. For example, if a woman had undergone the 4-week and 12-week survey in the post-training phase, these would be averaged for the post-phase calculation.
The study was approved by the following Human Research Ethics Committees (HREC): University of Newcastle HREC (#H-2015-0438). Aboriginal Health & Medical Research Council HREC (#1140/15). South Australia Aboriginal HREC (#04-16-652. Far North Queensland HREC (#16/QCH/34–1040)). Trial registration: Australian and New Zealand Clinical Trials Registry (ACTRN12616001603404).
Results
Table 1 illustrates the descriptive statistics for the RBD Scale and subscales and smoking behaviours at the different time-points. The table reports on percentages of women using the denominator of who were able to be followed up at each time point. The overall quit rate at 12-weeks (intention to treat analysis, so women lost to follow-up were considered as still smoking) was 3/22 (13.8%) (Gould et al., Reference Gould, Bovill, Pollock, Bonevski, Gruppetta, Atkins and Bar-Zeev2018). Table 1 shows the mean and mean difference from baseline as well as Cohen's D to provide a measure of standardised difference (0.2 small difference; 0.5 moderate difference; 0.8 large difference) (Cohen, Reference Cohen1988). The sign of the Cohen's D indicates the direction of the effect; most of the relationships the effects grew over time compared to the baseline.
Table 1. Smoking Behaviour and RBD Scale over the collection period

The mean perceived efficacy at baseline was 3.86 (95% CI: 3.62–4.1) reducing to 3.82 (95% CI: 3.56–4.08) and then to 3.64 (95% CI: 3.37–3.9) at 12-weeks. Similarly, the mean total perceived threat at baseline was 4.17 (95% CI: 3.94–4.41), this increased to 4.22 (95% CI: 3.97–4.47) at 4-weeks and then decreased to 4.08 (95% CI: 3.81–4.34) at 12-weeks. Both measures are observed to trend downwards over the course of the study with the largest mean difference occurring between 12-weeks and baseline, however, the data fails to support any statistically significant trend.
Table 2 shows the results by pre- and post-training of health providers at sites. The results suggest that total efficacy was 0.16 (95% CI: −0.49 to 0.17) units lower and the total threat score was 0.19 (95% CI: −0.36 to −0.02) units lower after the intervention date. Fear control responses of the women showed a large difference pre to post-training according to Cohen's D (0.85).
Table 2. RBD Scale over pre-post phases

Discussion
An adapted RBD Scale was serially administered to 22 pregnant women participating in the ICAN QUIT in Pregnancy trial as a nested study. The RBD Scale was analysed over three time points; baseline, 4-week follow-up and 12-week follow up. The results show a reduction in total threat and total efficacy over the course of the study when measured in collection stages and pre-post. According to the RBD theory, the women with a negative discriminating value (indicating their threat score was higher than their efficacy score) should then be in fear control. This was supported in the data with higher mean fear control response as the study progressed, while protection responses remained relatively flat. The data failed to indicate a significant difference in the trend which was also caused by the low sample size. However, the results support the RBD theory with an inverse relationship between perceived efficacy and fear control. While ideally, one would wish for efficacy to be higher post-intervention, in this case, there was a lower total perceived efficacy after the intervention coupled with higher fear control response. Due to the small numbers in the study, it was hard to determine if this was due to the intervention itself, or an effect of time.
The reduction of threat and efficacy seen at the 4-week and 12-week time point may alternately indicate a blunting effect (tuning out threat) over time. Blunting is a psychological coping style for a threat which involves distraction or avoidance (Miller, Reference Miller, Leo Montada, Filipp and Lerner2013). This potentially could be related to the work of quitting being hard, which could impact on the women's self-esteem and self-efficacy to some extent. Women may avoid or downplay the threat as a coping mechanism to suppress disturbing thoughts about their smoking and the threat to their baby, so balance their reduced perceived efficacy for quitting (or perception of their control over the situation). Women in general had a higher perceived threat than efficacy at baseline. This should be considered within the Australian context, where threat messages are highly evident, such as a very sick looking baby being portrayed as a graphic health warning on plain cigarette packs. Being anxious for a prolonged period of time is mentally exhausting and reducing the perception of threat may help conserve mental resources. Another consideration is that high levels of scepticism towards anti-smoking messages, which have been previously reported among Aboriginal people (Bond et al., Reference Bond, Brough, Spurling and Hayman2012), and by Aboriginal pregnant women who smoke (Gould et al., Reference Gould, Munn, Avuri, Hoff, Cadet-James, McEwen and Clough2013a). These attitudes would be reflected by the women in our study who had high levels of fear control. By not smoking stressors during pregnancy may become less manageable (Gould et al., Reference Gould, Bovill, Cadet-James, Clarke and Bonevski2016a). Aboriginal women are guided by the experiences of and relationships with maternal figures in their lives and if significant others have not had explicit health effects from smoking for themselves or baby, the possibilities for these may be denied (Gould et al., Reference Gould, Munn, Avuri, Hoff, Cadet-James, McEwen and Clough2013a, Reference Gould, Bovill, Cadet-James, Clarke and Bonevski2016a). Anti-smoking messages therefore may lack salience with women's lived experiences (Gould et al., Reference Gould, Munn, Avuri, Hoff, Cadet-James, McEwen and Clough2013a, Reference Gould, Cadet-James and Clough2016b). On the other hand, protection responses were high throughout the study. As the protection response scale was based on the levels of agreement with statements that included the responsibility of partners and Aboriginal people in general to not smoking around pregnant women, babies or indeed at all, the high protection response perhaps indicates views about a collective responsibility of Aboriginal people (including partners) around smoking in pregnancy and around children.
The only other studies of the RBD Scale in Aboriginal people were collected at a single time point: a small-scale study in pregnancy in N = 20 pregnant and recently pregnant Aboriginal women (Gould et al., Reference Gould, Bovill, Chiu, Bonevski and Oldmeadow2017), and a larger cross-sectional study using the RBD Scale with N = 121 Aboriginal smokers (male and female of reproductive age) (Gould et al., Reference Gould, Watt, Cadet-James and Clough2015b). Both studies indicated that Aboriginal people with high perceived efficacy and the high perceived threat had greater intentions to quit smoking than those with other RBD characteristics.
Health education and health messages for Aboriginal women could potentially be tailored by an individual's RBD Scale characteristics. The ICAN QUIT in Pregnancy training encouraged health providers to use efficacy messages but did not tailor health messages to the individual level of threat or efficacy. Tracking the RBD at various time points during pregnancy could facilitate timely and more appropriate messages, e.g. if efficacy or threat were seen to be waning. Practical support could be given on how to reduce anxiety and conserve mental resources during quit attempts to prevent blunting and avoid an increase in fear control responses or scepticism. The RBD Scale could be automated through an online format to deliver the most appropriately framed messages in real-time, e.g. through a mobile application using video, images or text.
Considering the broader implications of Aboriginal women assessing the risks of smoking in pregnancy, the sociocultural context remains vitally important and should be further explored through a qualitative inquiry. The personal responsibility that is placed on Aboriginal women to make the change to becoming a non-smoker, coupled with the moral imperative that stigmatises women who struggle to quit smoking, places an unfair burden on Aboriginal women when there are many barriers that are not being addressed. Broader barriers at a community and system-level include lack of accessible and culturally competent services for smoking cessation, inaccessibility of suitable forms of NRT, inconsistent and confusing messages from health providers and lack of training of health providers in this specialised area of maternal smoking (Gould, Reference Gould2014; Gould et al., Reference Gould, Cadet-James and Clough2016b). So far strategies have mostly focused on the pregnant woman herself, rather than involving the whole community and family contexts, including partners, to provide a supportive environment and share responsibility (Gould et al., Reference Gould, Bovill, Cadet-James, Clarke and Bonevski2016a). Aboriginal women also have expressed a belief that quitting is their own responsibility and they may be reluctant to go to health providers for advice or medications (Bovill et al., Reference Bovill, Gruppetta, Cadet-James, Clarke, Bonevski and Gould2018; Harris, Harris, Rae, & Chojenta, Reference Harris, Harris, Rae and Chojenta2019). Aboriginal women report being open to suggestions about community and Elder-based approaches (Bovill et al., Reference Bovill, Gruppetta, Cadet-James, Clarke, Bonevski and Gould2018). Partner and family approaches warrant urgent consideration. Stigma may induce emotional reactions that impair people from quitting smoking (Helweg-Larsen, Sorgen, & Pisinger, Reference Helweg-Larsen, Sorgen and Pisinger2019). Stigma requires more specific understanding in the Aboriginal context of maternal smoking; whether the experience of stigma could deter Aboriginal women who smoke from smoking cessation or from approaching health services in a timely way for antenatal care. The EPPM has previously been extended to include social threats such as stigma, as well as collective efficacy (Smith, Ferrara, & Witte, Reference Smith, Ferrara and Witte2007). This approach may be worthy of trial in this Aboriginal population.
Strengths and limitations
The strength of this study is that it is the first to use the RBD Scale over several time-points in an Aboriginal group of smokers and the first to use the RBD in a group of all-pregnant Aboriginal women involved in a smoking cessation pilot study. The data were collected face-to-face by a trusted member of staff at the woman's local ACCHS. It should be noted that some women were recruited prior to the services receiving the training intervention and resources, and some after the intervention, but the sample size was too small to make meaningful comparisons pre to post-intervention. Furthermore, we have no comparison data about how responses to the scale could change with gestation. The changes observed in scales might reflect the natural course of perceived threat and efficacy over the course of pregnancy. As the women were recruited over three states, some generalisation of findings may be theoretically possible. However, an overriding caution is that this was very preliminary data of RBD Scale use and threat and efficacy in pregnant Aboriginal women who smoke. As the women were recruited in the context of a trial about smoking cessation, the findings do not reflect Aboriginal women in the broader community. However, the data are nonetheless an important trial of the RBD Scale in this context, and worthy of use in a larger sample. Additionally, qualitative data from the women could have enriched the understanding of some of the constructs of the scale and women's responses to the intervention but was not feasible at the time. We would recommend this for future research.
Conclusion
In 22 women recruited to a smoking cessation intervention in ACCHS in three Australian states, an adapted RBD Scale including measures of perceived threat and perceived efficacy for smoking was collected and analysed at three time-points. A trend for reduction of threat and efficacy at 4-weeks and 12-weeks may suggest a blunting effect as a response to the threat or the natural course during pregnancy. Quitting is hard work, which could erode women's self-efficacy. A longitudinal study with a larger sample would clarify the use of the RBD Scale for smoking in pregnancy, and whether it could be a predictor for quitting. The RBD could have the potential for individual tailoring of health messages. Further research is required to understand risk perceptions and stigma in Aboriginal women who smoke and the potential for community and partner-based approaches.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/jsc.2020.27
Acknowledgements
The authors thank the Stakeholder and Consumer Aboriginal Advisory Panel for ICAN QUIT in Pregnancy, for advising on the components of this intervention. They also thank the Aboriginal communities who have contributed to the development and implementation of the ICAN QUIT in Pregnancy intervention. This includes staff and patients of Biripi Aboriginal Corporation, Tobwabba Aboriginal Medical Service, Pangula Mannamurna Aboriginal Corporation, Riverina Medical and Dental Aboriginal Corporation, Wuchopperen Health Service Ltd, and Tharawal Aboriginal Corporation.
Author contributions
GSG designed the study, was responsible for all aspects of the study and wrote the manuscript. SC conducted the statistical analysis overseen by CO; YBZ contributed to the study design and implementation. MB contributed to the study design, implementation, the interpretation of data and Aboriginal cultural competence of the study. All authors read and approved the final manuscript. The following collaborators are in the ICAN QUIT in Pregnancy Pilot Group: Gillian S Gould, Billie Bonevski, Peter O'Mara, Marilyn J Clarke, Chris Oldmeadow, Alan Clough, Kristin Carson, Jennifer Reath, Yael Bar-Zeev, Michelle Bovill, Katherine M Boydell, Ling Li Lim, Maree Gruppetta, Roger Smith, Yvonne Cadet-James, Renee Bittoun, Lou Atkin, Brett Cowling, Lisa Orcher.
Financial support
This work was funded by the New South Wales Ministry of Health, the Hunter Cancer Research Alliance, the National Health and Medical Research Council (fellowship to GSG APP1092085) and Cancer Institute New South Wales (Early Career Research Fellowships to GSG #15ECF/I-52). MB is supported by the University of Newcastle and Australian Heart Foundation Indigenous Scholarship (#101555). The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Conflict of interest
YBZ has received fees for lectures in the past (years 2012–2015, 2017–07.2019) from Pfizer Israel LTD and Novartis NCH (distributes smoking cessation pharmacotherapy in Israel). She has not received any fees from pharmaceutical companies in Australia. No other authors have competing interests to declare.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Data sharing statement
No data is publicly available.








