Crossref Citations
This article has been cited by the following publications. This list is generated based on data provided by
Crossref.
Gorbunova, Marina
Lemkina, Larisa
and
Nechaev, Anton
2021.
Guanidinium and Phosphonium Scaffolds Loaded with Silver Nanoparticles: Synthesis, Characterization, In Vitro Assessment of the Antibacterial Potential and Toxicity.
Journal of Inorganic and Organometallic Polymers and Materials,
Vol. 31,
Issue. 5,
p.
2218.
Korolev, Dmitry
Shumilo, Michael
Shulmeyster, Galina
Krutikov, Alexander
Golovkin, Alexey
Mishanin, Alexander
Gorshkov, Andrew
Spiridonova, Anna
Domorad, Anna
Krasichkov, Alexander
and
Galagudza, Michael
2021.
Hemolytic Activity, Cytotoxicity, and Antimicrobial Effects of Human Albumin- and Polysorbate-80-Coated Silver Nanoparticles.
Nanomaterials,
Vol. 11,
Issue. 6,
p.
1484.
Tiwari, Atul K.
Mishra, Anupa
Pandey, Govind
Gupta, Munesh K.
and
Pandey, Prem C.
2022.
Nanotechnology: A Potential Weapon to Fight against COVID‐19.
Particle & Particle Systems Characterization,
Vol. 39,
Issue. 1,
Mahboubi, Arash
Moghimi, Hamid Reza
Mortazavi, Seyedeh Maryam
Gorji-bahri, Gilar
and
Gandomkarzadeh, Marzieh
2022.
Emerging Nanomaterials and Nano-Based Drug Delivery Approaches to Combat Antimicrobial Resistance.
p.
57.
Tiwari, Atul Kumar
Gupta, Munesh Kumar
Pandey, Govind
Tilak, Ragini
Narayan, Roger J.
and
Pandey, Prem C.
2022.
Size and Zeta Potential Clicked Germination Attenuation and Anti-Sporangiospores Activity of PEI-Functionalized Silver Nanoparticles against COVID-19 Associated Mucorales (Rhizopus arrhizus).
Nanomaterials,
Vol. 12,
Issue. 13,
p.
2235.
Tiwari, Atul Kumar
Gupta, Munesh Kumar
Pandey, Govind
Pandey, Shivangi
and
Pandey, Prem C.
2023.
Amine-Functionalized Silver Nanoparticles: A Potential Antiviral-Coating Material with Trap and Kill Efficiency to Combat Viral Dissemination (COVID-19).
Biomedical Materials & Devices,
Vol. 1,
Issue. 2,
p.
618.
Tiwari, Atul Kumar
Gupta, Munesh Kumar
Narayan, Roger J.
and
Pandey, Prem C.
2023.
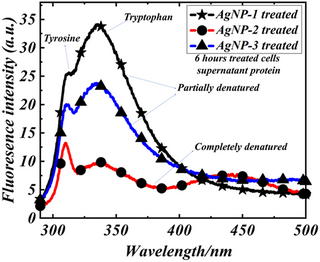
A whole cell fluorescence quenching-based approach for the investigation of polyethyleneimine functionalized silver nanoparticles interaction with Candida albicans.
Frontiers in Microbiology,
Vol. 14,
Issue. ,
Tiwari, Atul Kumar
Yadav, Hari Prakash
Gupta, Munesh Kumar
Narayan, Roger J.
and
Pandey, Prem C.
2023.
Synthesis of vancomycin functionalized fluorescent gold nanoparticles and selective sensing of mercury (II).
Frontiers in Chemistry,
Vol. 11,
Issue. ,
Tiwari, Atul Kumar
Gupta, Munesh Kumar
Yadav, Hari Prakash
Narayan, Roger J.
and
Pandey, Prem C.
2024.
Aggregation-Resistant, Turn-On-Off Fluorometric Sensing of Glutathione and Nickel (II) Using Vancomycin-Conjugated Gold Nanoparticles.
Biosensors,
Vol. 14,
Issue. 1,
p.
49.
Sarkar, Sourav
Moitra, Parikshit
and
Bhattacharya, Santanu
2024.
Structure–activity relationship of drug conjugated polymeric materials against uropathogenic bacteria colonization under in vitro and in vivo settings.
Journal of Materials Chemistry B,
Vol. 12,
Issue. 1,
p.
187.
Tiwari, Atul Kumar
Gupta, Munesh Kumar
Meena, Ramovatar
Pandey, Prem C.
and
Narayan, Roger J.
2024.
Molecular Weights of Polyethyleneimine-Dependent Physicochemical Tuning of Gold Nanoparticles and FRET-Based Turn-On Sensing of Polymyxin B.
Sensors,
Vol. 24,
Issue. 7,
p.
2169.