Crossref Citations
This article has been cited by the following publications. This list is generated based on data provided by
Crossref.
Barber, Helena
Kelly, Cambre N.
Nelson, Kaitlin
and
Gall, Ken
2021.
Compressive anisotropy of sheet and strut based porous Ti–6Al–4V scaffolds.
Journal of the Mechanical Behavior of Biomedical Materials,
Vol. 115,
Issue. ,
p.
104243.
Beloshenko, Victor
Beygelzimer, Yan
Chishko, Vyacheslav
Savchenko, Bogdan
Sova, Nadiya
Verbylo, Dmytro
Voznyak, Andrei
and
Vozniak, Iurii
2021.
Mechanical Properties of Flexible TPU-Based 3D Printed Lattice Structures: Role of Lattice Cut Direction and Architecture.
Polymers,
Vol. 13,
Issue. 17,
p.
2986.
Deering, Joseph
Presas, Alexandre
Yu, Bosco
Valentin, David
Heiss, Christian
Bosbach, Wolfram A.
and
Grandfield, Kathryn
2021.
Implant resonance and the mechanostat theory: Applications of therapeutic ultrasound for porous metallic scaffolds.
Materials Science and Engineering: C,
Vol. 125,
Issue. ,
p.
112070.
Kelly, Cambre N.
Kahra, C.
Maier, Hans J.
and
Gall, Ken
2021.
Processing, structure, and properties of additively manufactured titanium scaffolds with gyroid-sheet architecture.
Additive Manufacturing,
Vol. 41,
Issue. ,
p.
101916.
Nelson, Kaitlin
Kelly, Cambre N.
and
Gall, Ken
2022.
Effect of stress state on the mechanical behavior of 3D printed porous Ti6Al4V scaffolds produced by laser powder bed fusion.
Materials Science and Engineering: B,
Vol. 286,
Issue. ,
p.
116013.
Hou, Chenjin
Liu, Yitong
Xu, Wei
Lu, Xin
Guo, Lijia
Liu, Yi
Tian, Shiwei
Liu, Bowen
Zhang, Jiazhen
and
Wen, Cuie
2022.
Additive manufacturing of functionally graded porous titanium scaffolds for dental applications.
Biomaterials Advances,
Vol. 139,
Issue. ,
p.
213018.
Peloquin, Jacob
Kirillova, Alina
Rudin, Cynthia
Brinson, L.C.
and
Gall, Ken
2023.
Prediction of tensile performance for 3D printed photopolymer gyroid lattices using structural porosity, base material properties, and machine learning.
Materials & Design,
Vol. 232,
Issue. ,
p.
112126.
DEPBOYLU, Fatma Nur
POYRAZ, Özgür
YASA, Evren
and
KORKUSUZ, Feza
2023.
Lazer-Toz Yatağında Füzyon ile Üretilen Ti6Al4V Gyroid Yapıların Basma Dayanımlarının Nümerik Modellenmesi.
Afyon Kocatepe University Journal of Sciences and Engineering,
Vol. 23,
Issue. 1,
p.
270.
Dastani, Kia
Movahhedy, Mohammad R.
Yu, Hongyu
Khodaygan, Saeed
Zhang, Lei
and
Wang, Michael Yu
2023.
Effect of geometric deviations on the strength of additively manufactured ultralight periodic shell-based lattices.
Engineering Failure Analysis,
Vol. 150,
Issue. ,
p.
107328.
Suryawanshi, Chetana Madhukar
Sagar, Samrat
Bhallamudi, Ravi
and
Mishra, Sushil
2023.
Effective design and mechanical response of Gyroid lattice scaffold for orthopedic implants.
Manufacturing Letters,
Vol. 35,
Issue. ,
p.
493.
Khrapov, Dmitriy
Paveleva, Aleksandra
Kozadayeva, Maria
Evsevleev, Sergei
Mishurova, Tatiana
Bruno, Giovanni
Surmenev, Roman
Koptyug, Andrey
and
Surmeneva, Maria
2023.
Trapped powder removal from sheet-based porous structures based on triply periodic minimal surfaces fabricated by electron beam powder bed fusion.
Materials Science and Engineering: A,
Vol. 862,
Issue. ,
p.
144479.
Hitchon, Sydney
Soltanmohammadi, Pendar
Milner, Jaques S.
Holdsworth, David
and
Willing, Ryan
2024.
Porous versus solid shoulder implants in humeri of different bone densities: A finite element analysis.
Journal of Orthopaedic Research,
Mathey, Elizabeth
Heimbrook, Amanda
Carpenter, R. D.
Kelly, Cambre N.
and
Gall, Ken
2024.
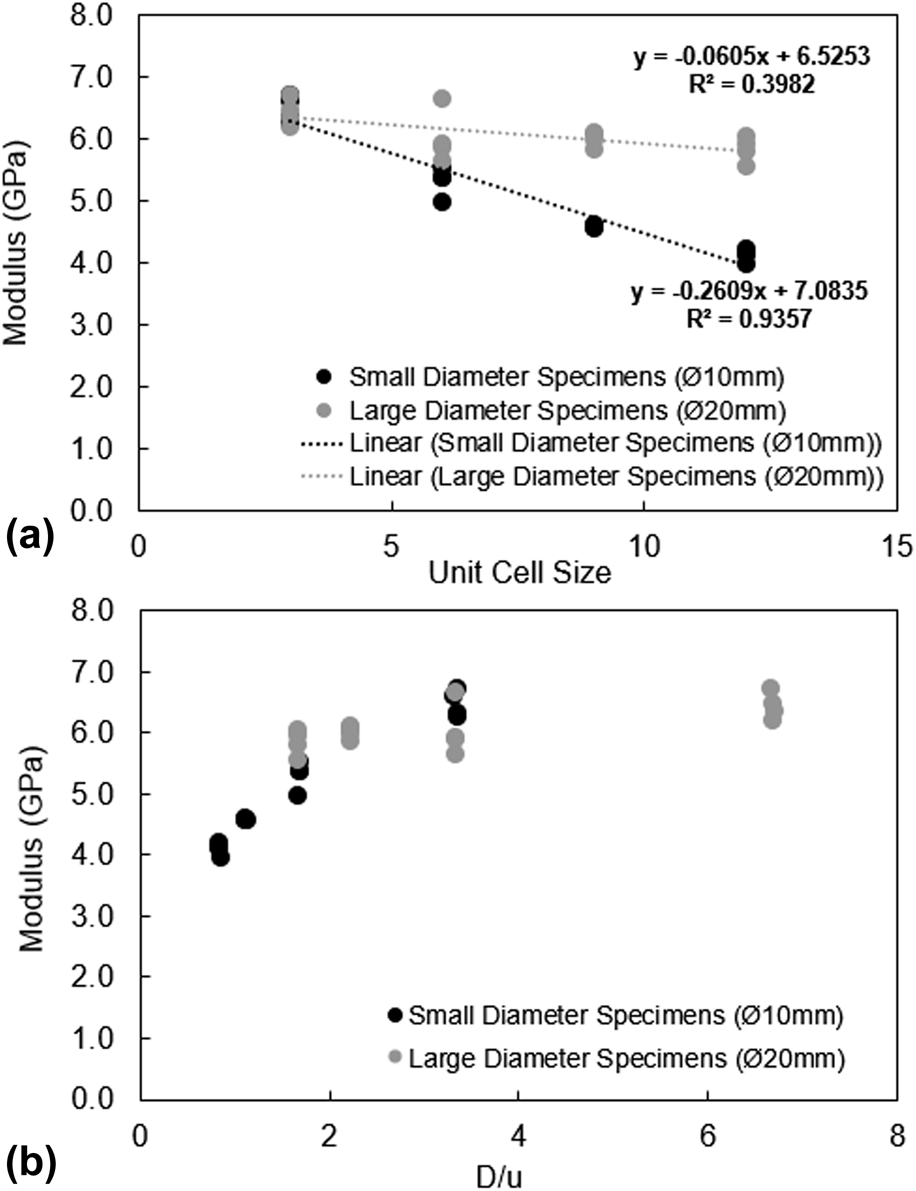
Finite element modeling of the free boundary effect on gyroid additively manufactured samples.
Computer Methods in Biomechanics and Biomedical Engineering,
p.
1.
López-Barroso, Juventino
Flores-Hernández, Cynthia Graciela
Martínez-Hernández, Ana Laura
Martínez-Barrera, Gonzalo
and
Velasco-Santos, Carlos
2024.
Advanced Composites.
p.
121.