Crossref Citations
This article has been cited by the following publications. This list is generated based on data provided by
Crossref.
Luo, You-Ran
Zhang, Li
Chen, Cheng
Sun, Dong-Yuan
Wu, Peng
Wang, Yue
Liao, Yun-Mao
Cao, Xiao-Yan
Cheng, Cheng-Kung
Tang, Zi-Qing
and
Liang, Xing
2018.
The delayed degradation mechanism and mechanical properties of β-TCP filler in poly(lactide-co-glycolide)/beta-tricalcium phosphate composite suture anchors during short-time degradation in vivo.
Journal of Materials Research,
Vol. 33,
Issue. 24,
p.
4278.
Banerjee, Dishary
and
Bose, Susmita
2019.
Effects of polymer chemistry, concentration, and pH on doxorubicin release kinetics from hydroxyapatite-PCL-PLGA composite.
Journal of Materials Research,
Vol. 34,
Issue. 10,
p.
1692.
Basu, Subhadip
and
Basu, Bikramjit
2019.
Unravelling Doped Biphasic Calcium Phosphate: Synthesis to Application.
ACS Applied Bio Materials,
Vol. 2,
Issue. 12,
p.
5263.
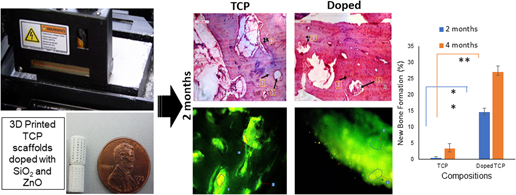
Fielding, Gary A.
Sarkar, Naboneeta
Vahabzadeh, Sahar
and
Bose, Susmita
2019.
Regulation of Osteogenic Markers at Late Stage of Osteoblast Differentiation in Silicon and Zinc Doped Porous TCP.
Journal of Functional Biomaterials,
Vol. 10,
Issue. 4,
p.
48.
Meininger, Susanne
Vorndran, Elke
Castilho, Miguel
Fernandes, Paulo Rui
and
Gbureck, Uwe
2019.
New Developments in Tissue Engineering and Regeneration.
Vol. 51,
Issue. ,
p.
51.
Lowe, Baboucarr
Ottensmeyer, Mark P.
Xu, Chun
He, Yan
Ye, Qingsong
and
Troulis, Maria J.
2019.
The Regenerative Applicability of Bioactive Glass and Beta-Tricalcium Phosphate in Bone Tissue Engineering: A Transformation Perspective.
Journal of Functional Biomaterials,
Vol. 10,
Issue. 1,
p.
16.
Thilakan, Jaya
Mishra, Ruchi
Goel, Sudhir K.
and
Arya, Neha
2019.
Biomaterials in Orthopaedics and Bone Regeneration.
p.
175.
Zhao, Yingchun
Hou, Yue
Li, Zhaoyu
Wang, Ziyu
and
Yan, Xinxin
2020.
Powder-Based 3D Printed Porous Structure and Its Application as Bone Scaffold.
Frontiers in Materials,
Vol. 7,
Issue. ,
Zhou, Tianyuan
Zhang, Le
Yao, Qing
Ma, Yuelong
Hou, Chen
Sun, Bingheng
Shao, Cen
Gao, Pan
and
Chen, Hao
2020.
SLA 3D printing of high quality spine shaped β-TCP bioceramics for the hard tissue repair applications.
Ceramics International,
Vol. 46,
Issue. 6,
p.
7609.
Jensen, Martin Bonde
Slots, Casper
Ditzel, Nicholas
Kolstrup, Stefanie
Kassem, Moustapha
Thygesen, Torben
and
Andersen, Morten Østergaard
2020.
Treating mouse skull defects with 3D‐printed fatty acid and tricalcium phosphate implants.
Journal of Tissue Engineering and Regenerative Medicine,
Vol. 14,
Issue. 12,
p.
1858.
Haleem, Abid
Javaid, Mohd
Khan, Rizwan Hasan
and
Suman, Rajiv
2020.
3D printing applications in bone tissue engineering.
Journal of Clinical Orthopaedics and Trauma,
Vol. 11,
Issue. ,
p.
S118.
Shuai, Cijun
Yu, Li
Feng, Pei
Gao, Chengde
and
Peng, Shuping
2020.
Interfacial reinforcement in bioceramic/biopolymer composite bone scaffold: The role of coupling agent.
Colloids and Surfaces B: Biointerfaces,
Vol. 193,
Issue. ,
p.
111083.
BONATTI, Amedeo F.
CHIESA, Irene
MICALIZZI, Simone
VOZZI, Giovanni
and
DE MARIA, Carmelo
2021.
Bioprinting for bone tissue engineering.
Minerva Orthopedics,
Vol. 72,
Issue. 4,
Bahraminasab, Marjan
Janmohammadi, Mahsa
Arab, Samaneh
Talebi, Athar
Nooshabadi, Vajihe Taghdiri
Koohsarian, Parisa
and
Nourbakhsh, Mohammad Sadegh
2021.
Bone Scaffolds: An Incorporation of Biomaterials, Cells, and Biofactors.
ACS Biomaterials Science & Engineering,
Vol. 7,
Issue. 12,
p.
5397.
Najafloo, Raziyeh
Baheiraei, Nafiseh
and
Imani, Rana
2021.
Synthesis and characterization of collagen/calcium phosphate scaffolds incorporating antibacterial agent for bone tissue engineering application.
Journal of Bioactive and Compatible Polymers,
Vol. 36,
Issue. 1,
p.
29.
Herber, Valentin
Okutan, Begüm
Antonoglou, Georgios
Sommer, Nicole G.
and
Payer, Michael
2021.
Bioresorbable Magnesium-Based Alloys as Novel Biomaterials in Oral Bone Regeneration: General Review and Clinical Perspectives.
Journal of Clinical Medicine,
Vol. 10,
Issue. 9,
p.
1842.
Wang, Niyou
Thameem Dheen, S.
Fuh, Jerry Ying Hsi
and
Senthil Kumar, A.
2021.
A review of multi-functional ceramic nanoparticles in 3D printed bone tissue engineering.
Bioprinting,
Vol. 23,
Issue. ,
p.
e00146.
Leeflang, M.A.
Bobbert, F.S.L.
and
Zadpoor, A.A.
2021.
Additive manufacturing of non-assembly deployable mechanisms for the treatment of large bony defects.
Additive Manufacturing,
Vol. 46,
Issue. ,
p.
102194.
Lu, Haiping
Zhou, Yinghong
Ma, Yaping
Xiao, Lan
Ji, Wenjun
Zhang, Yi
and
Wang, Xin
2021.
Current Application of Beta-Tricalcium Phosphate in Bone Repair and Its Mechanism to Regulate Osteogenesis.
Frontiers in Materials,
Vol. 8,
Issue. ,
Ahlhelm, Matthias
Latorre, Sergio H.
Mayr, Hermann O.
Storch, Christiane
Freytag, Christian
Werner, David
Schwarzer-Fischer, Eric
and
Seidenstücker, Michael
2021.
Mechanically Stable β-TCP Structural Hybrid Scaffolds for Potential Bone Replacement.
Journal of Composites Science,
Vol. 5,
Issue. 10,
p.
281.