Background
Academic–community relationships can support the design and conduct of research responsive to local needs and priorities and build lasting change through education and increased research capacity. In this article, we will describe how we developed and implemented a Community Research Liaison Model (CLRM), a community-engaged research (CEnR) approach to respond to rural needs in Oregon and build sustained capacity for CEnR and data-driven solutions to local health issues. The CLRM is a joint effort led by our National Clinical and Translational Science-funded Clinical and Translational Research Institute and National Cancer Institute-funded comprehensive cancer institute.
CEnR (and the closely related Community-Based Participatory Research; CBPR) emerged in the 1940s and has evolved over time across fields such as psychology, sociology, public health, and social work [Reference Wallerstein1]. Central to CEnR is the role of communities as partners and active participants in all aspects of knowledge creation through research activity [Reference Israel, Schulz, Parker and Becker2]. The social justice movement was instrumental in informing the principles around CEnR, viewing lived experiences, historical harm, and social structures as important factors for community wellness and health promotion [Reference Wallerstein1]. CEnR has become increasingly used for translational and implementation sciences aiming to take research “from bench to practice,” a shift is in part due to national funding priorities [Reference Eder, Mickey and Funes3]. Multiple frameworks guiding community-engaged implementation and adaptation of evidence-based interventions have been suggested since 1967, with over 50 added since the turn of the millinum [Reference Pinto, Park (Ethan), Miles and Ong4]. Finally, CEnR has been suggested for supporting advocacy and equitable health policy work by providing a frame for centering multiple and diverse voices [Reference Wright, Olomi and DePrince5]. When health research aims to make a sustainable impact, practice and policy change may often be an end goal.
Part of ensuring better health is including community values, processes, and lived experience as contextual factors for understanding health risks and barriers to health promotion [Reference Gilbert, Laroche, Wallace, Parker and Curry6]. Long-term changes have far more viable prospects when the community defines the problem, contributes knowledge, receives training, and participates in and co-structures research activities [Reference Lantz, Viruell-Fuentes, Israel, Softley and Guzman7,Reference Wallerstein, Oetzel and Sanchez-Youngman8].
In this article, we describe the structures and processes that guide our work applying CEnR in Oregon, and how it may be replicated across other regions. We also provide examples specific to local communities in Oregon as a reflection of the research and health promotion resulting from our process.
Model Development
The inception of our model was guided by the principles of community engagement and an acknowledgement that all communities have existing community-based organizations involved in health promotion efforts [9]. The institutional support from a large academic entity facilitated the development and continues to be the backbone for the day-to-day operations of what has become a formal model for CEnR in Oregon.
To develop our model, we followed a multi-phase process with continuous iterations and lessons-learned sessions to design and implement an effective community engagement model that could be replicated. Our work began with a pilot in the three largely rural counties of Central Oregon. We hired a community engagement specialist, a member of the local community, to examine community research engagement feasibility and readiness. The specialist implemented an adapted version of the Interactive Systems Framework (ISF) [Reference Wandersman, Duffy and Flaspohler10], a research-to-practice framework embracing community engagement. We chose the ISF because there are several notable examples in the literature where this framework was used to guide research to practice to community engagement activities [Reference Firesheets, Francis, Barnum and Rolf11–Reference Fernández, Melvin and Leeman13]. Importantly, the ISF recognizes that a top-down approach to community engagement implementation is suboptimal [Reference Pinto, Park (Ethan), Miles and Ong4,Reference Wandersman, Duffy and Flaspohler10]. Key stakeholders and community partnerships are integral to an effective, long-lasting approach to community engagement. Our adaptation of the ISF began by developing the Community Research Engagement Assessment (CREA) to explore community motivation.
The ISF is based on the equation: R=MC2 (Readiness = Motivation × General Capacity and Intervention-Specific Capacity), where readiness refers to the extent to which the region is willing and able to implement, participate in, and direct CEnR and use data to drive decision-making [Reference Dymnicki, Wandersman, Osher, Grigorescu and Huang14]. The CREA assessed community motivation (i.e., local champions and leadership), general capacity (i.e., community infrastructure and resources), and intervention capacity (i.e., adoption of research-based practices and data-driven decision-making). We collected data through key informant interviews, gleaning information about the region, the general capacity of organizations that focus on improving health and conducting research, and the capacity within the community/organization for using data to inform decisions and conduct research. We assessed motivation for building research capacity, academic partnerships, and the idea of a research advisory. We also gathered community perceptions of our academic institution to understand the level of recognition and trust the institution carried in the community. We interviewed leaders across several sectors including government, education, business, health and human services, community advocacy, and bioscience/biotechnology as part of the assessment.
Through the assessment, we identified gaps, current efforts, and opportunities where community-based organizations could be supported by resources, including academic expertise, research services, funding opportunities, technical assistance, and training. Further, the community engagement specialist identified champions and leaders in the community to be part of an advisory group to assure efforts are aligned with community needs and priorities.
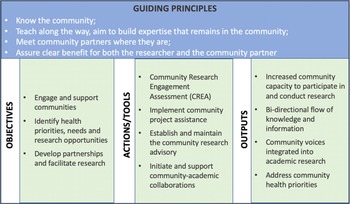
Using results from the CREA, and informed by the ISF and initial efforts of the community engagement specialist, we created a new conceptual framework to guide our formal model. Our conceptual framework specifies the guiding principles, objectives, actions to facilitate the objectives (i.e., capacity, motivations, and partners), and outputs (Fig. 1). Our conceptual framework fits within the ISF but lays out the specific steps and tools we identified as useful to understand local needs and moving to action. The CREA continues to be an important part of actions used to engage with communities, but other actions and assessment tools have been added.

Fig. 1. Community-engaged research conceptual framework.
Building on the success of the initial community engagement specialist in Central Oregon, we moved toward expanding this model to other rural regions in our state and the engagement specialist role was renamed “Community Research Liaison” (CRL). The model which we use today is therefore known as the CRLM.
The Community Research Liaisons
The CRLs are the lynchpin of our CRLM. CRLs are embedded in their community and work with community partners following a consistent yet flexible approach to identify and respond to the health-related needs of their region. The CRLs are full-time employees hired from their community. They have a bachelor degree or higher and a background in public health, community organizing or nonprofit work, as well as strong interpersonal and communication skills. Liaisons often have only minimal prior experience with academia or research, but have a deep connection to their local community. They develop and maintain relationships with local partners, allowing for a bidirectional exchange of ideas and support. The CRLs will be assessing trust in their community, but do not yet have pre-post assessments.
CRLs promote collaborations between community and academic researchers and facilitate research-based practices and data-driven decision-making. The result is increased capacity in a community’s ability to participate in, and conduct, research activities.
The CRLM builds upon the science or implementation of CEnR through a novel long-term relationship building approach. The CRL is embedded in the community in which they live and work. The literature suggests that effective CEnR is built over time [Reference Holzer, Ellis and Merritt15,Reference Wilkins16]. This approach facilitates relationship building and trust through proximal exchanges where trust is established through successive collaborations and partnership opportunities.
Community Research Hub
To provide support and assist in maintaining fidelity to the CRLM, our CRL team is supported by a coordinating center, the Community Research Hub (The Hub). The Hub is a centralized office strategically located in the center of the state and is funded in part by its university affiliation, and in part by projects. The Hub employs a dedicated community research program manager that leads the liaison team and supports the liaisons by connecting regional partners to academic and other resources. The Hub provides resources, technical assistance, and guidance in support of the liaison activities to facilitate CEnR. Further, The Hub supports the community research program manager to identify areas of possible common interests across CRL sites and to leverage resources to efficiently address needs that have been identified across multiple regions.
The Community Research Liaison Model
The CRLM has four actions or “tools” which CRLs and academic researchers use to move from objectives to outputs within communities (Fig. 1). We outline these actions below, describing how they support community involvement in research activities. Action 1 (CREA) determines the community’s readiness to engage in research. Depending on the findings from the assessment, the remaining three actions may be carried out, or only a subset of actions.
CRL Model Action 1. Community Research Engagement Assessment
An important first step in establishing the role of a CRL within the community is the completion of a CREA. As described above in the description of the Central Oregon pilot, the CREA is a community-based tool to understand specific community capacity and readiness to engage in research. The assessment can be led by CRLs and community members. The CREA is based on interviews with key partners or leaders in the community identified based on their role in health care, education, the public sector, and other industry or business unique to the particular region. The interviews follow the same format as the Central Oregon pilot. The findings are used to guide development and priorities of a community advisory group, to identify needs that may be addressed through new partnerships, and to learn about beliefs, knowledge, and resources within the community that may inform the CRL’s work.
CRL Model Action 2. Community Project Assistance
To facilitate consistent community engagement and support, all CRLs have implemented a common approach for community-based organizations to receive research technical assistance, training, and explore funding opportunities. This approach, the community project assistance program, is where community–academic partnerships often develop and where needs are identified. CRLs conduct standardized consults with community-based organizations and groups to better understand their research and data needs. Consultation notes are reviewed weekly with The Hub leadership team to identify opportunities for connecting the organization with the appropriate resources, technical assistance, and academic collaborators. After a connection is made, CRLs continue to serve as facilitators, bridging the gap between community and academia, and building the capacity of community organizations to participate in and conduct CEnR.
CRL Model Action 3. Support Community Research Advisory
CRLs also coordinate and facilitate a community research advisory. The purpose of developing a research advisory is to bring local and regional community leaders together with academic partners to collaborate, network and build local capacity for research and data-driven decision-making to improve health and wellness in the community. The advisories most often identify, develop, and champion larger cross-sector projects. Each advisory has a slightly different structure to meet the unique needs and priorities of the community and is comprised of community leaders who represent the diversity and interests in each region. The model of engagement is based on collaboration and shared leadership and ensures the community is an active part of the research process and provides input on priorities for engagement.
CRL Model Action 4. Develop Community–Academic Collaborations
Through the community project assistance and community research advisories, the CRLs facilitate community and academic connections. The CRLs understand and are able to communicate their community’s health priorities to academic researchers and conversely, the researcher’s objectives and strategy to the community. CRLs foster these relationships by facilitating consistent bidirectional communication, creating opportunities for discussion, framing relevant questions and concepts, identifying funding opportunities, and drafting scopes of work or protocols.
Results
The CRLM is now fully implemented in one urban and four rural areas in Oregon that include the North Coast (3 counties), the South Coast (2 counties), Southern Oregon (2 counties), and the Columbia River Gorge (4 counties) and continues in the three counties of Central Oregon. A CRL has also recently been hired to work with the four counties of Northeast Oregon.
The success of the initial Central Oregon pilot is seen in Fig. 2. The CRL began supporting projects in 2017, and the number of projects has grown each year. As the CRL model was initiated in each additional region, projects in those areas have also increased. Overall, since 2017, the liaison team has engaged with communities on nearly 300 community projects.

Fig. 2. Number of projects by year and region.
Projects have a strong focus on rural areas (44 projects), reach diverse populations (6 with tribes, 5 with Hispanic or Latino organizations), and different age ranges (26 with youth/children, 7 with older adults). CRLs facilitate CEnR supported by a range of team members, including data analysts, student workers and interns, project managers, and researchers from the Community Research Hub. Multiple services are provided for a project and can range from assistance with literature searches, to quantitative and qualitative data collection, data analysis, interpretation and presentation, program evaluation, and survey design interpretation and presentation.
At the inception of the CRLM, most projects were pro-bono in an effort to build trust and demonstrate the value of partnership. Over time, more projects have been funded by contracts and grants, coming both from the community and researchers.
Case Studies
The selected case studies (Perinatal Care Coordination example and Table 1) provide context for the types of projects and relationships facilitated by the CRLM. The CRLM facilitates community engagement and support through the actions and tools outlined in our conceptual framework (i.e., CREA, Community Project Assistance, Community Research Advisory, and Community–Academic Collaborations) and follow a consistent approach to community engagement through these actions and tools. The impact of this work is particularly notable when CRLs identify areas of shared need across regions and are able to connect partners across the state or use work in one region to inform projects elsewhere.
The selected case studies vary in focus and scope, but all address local priorities and health needs and follow the CRLM starting with Action 1 followed by various combinations of Actions 2, 3, and 4.
Perinatal Care Coordination, a Case Study
Central Oregon’s Perinatal Care Coordination (PCC) is a community-developed and public health-led cross-sector partnership to assist pregnant and postpartum individuals in Central Oregon’s three rural counties to access health insurance, perinatal care, nutritional services, behavioral health services, and other referrals with ease and dignity. PCC’s objectives include 1) decrease incidence of low birth weight in Central Oregon; 2) increase timely perinatal care initiation; 3) increase eligible referrals to community-based resources, WIC, and behavioral health services; and 4) solicit provider and community partner feedback on the implementation process and sustainability of the program.
Objectives. Through prior completion of the CREA (Action 1), the CRL was aware of a group that met regularly to address perinatal care and began attending, listening, and getting to know the group participants and their work. While attending, the CRL also worked to accomplish a second objective of identifying health priorities, needs, and research opportunities. The CRL identified a need when the PCC program shared that to sustain funding and expand program reach, it was necessary to evaluate the program and demonstrate intervention efficacy. The PCC team needed technical assistance to develop and implement an evaluation.
Actions. The CRL shared information about the Community Project Assistance Program (Action 2) with the community group, who expressed interest in collaborating. The CRL conducted a consult to obtain necessary information and to determine how The Hub could best support the project. A doctoral student and her mentors, who had interest and expertise in maternal and child health, were identified as potential academic collaborators. The CRL initiated a collaboration between the researchers and the PCC team by making introductions, scheduling meetings, and facilitating conversations to plan program evaluation and means to transition the model into other sites (Action 4).
Outputs. Through this process, CRLs developed a new partnership, and the community partners increased their capacity to participate in and conduct research. The work began by discussing the necessary components to create evidence for an intervention and conduct a research project. The academic–community team worked together to design a research protocol and began to identify potential funding. A Ph.D. student led the work with help from academic mentors and an undergraduate intern. They identified an evaluation framework, submitted three grants, and secured $30,000 in partial funding to begin the project. They have successfully completed planned evaluation activities and designed a handbook to aid transition of the intervention into other regions.
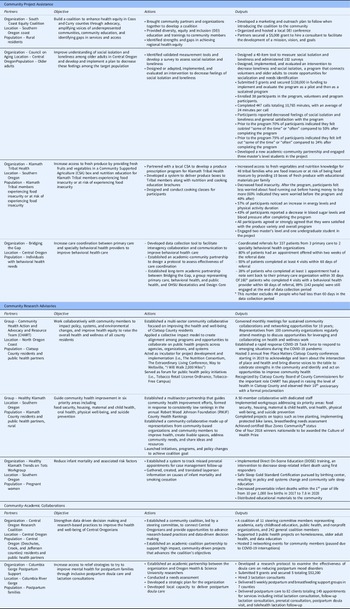
Table 1 Description
The case studies in Table 1 are organized by the CRL actions and tools: community project assistance, community research advisories, and community–academic collaborations. While distinct, CRL actions are interrelated. Outputs from one action could inform another action, or two actions might run in parallel and supplement each other. For example, health needs identified through a CREA (Action 1) lead to areas addressed through the community project assistance program (Action 2), and/or informs priorities for community research advisories (Action 3). Within each Action category, Table 1 presents projects by: Partners, Objectives, Actions, and Outputs.
Table 1. Facilitating and building capacity for community-engaged research case studies

Discussion
Similar to other community programs dedicated to building capacity for CEnR [Reference Wallerstein17], our CRLM is based on the idea that community partnerships build research capacity at the community level and are the backbone for pursuing equitable solutions and better health for the communities we serve. Our model is unique in its use of CRLs to facilitate community–academic partnerships; this model has brought both successes and challenges over the years. An important aspect of the model is that community partners build and sustain their capacity to lead and conduct research, even after projects conclude. Partners build skills such as data literacy and identification of evaluation frameworks; these carry across time and projects as communities identify new or expanded needs. Understanding local, unique community contexts, both rural and urban, is a defining feature of our CRLM and is what leads us to build and continue to strengthen research capacity and community relationships. Another aspect of research capacity is the ability to identify and formulate research questions to move specific health promotion efforts faster and more effectively in the desired direction (like pursuing funding, or establishing the evidence base for new programs). Often, one project leads to the next as community members and partners find use and value in data-driven approaches (see Council on Aging in Table 1). As the CRLM continues to grow in capacity and reach (geographically and demographically), the lessons learned along the way are used for consistent reflection and improvement.
Lesson 1. The Value of Being Present
CRLs live within the communities that they serve, have deep roots in the social fabric, and understand customs, beliefs, and community processes. The consensus among CRLs is that trust and relationship building is a long-term endeavor and being embedded in their community is a fundamental feature of the model. To that end, CRLs have discovered the value of “participating beyond their own projects.” A key aspect of building strong relationships is attending meetings, public forums, or small group settings which are not required, expected, or necessarily relevant to current work. However, at times activities outside active projects have created tension between research agendas and timelines and the more elusive, long-term investment in building relationships. Liaisons sometimes struggle to quantify their work, but as stronger research advisories have been formed and communities have become more aware of the opportunities to collaborate with CRLs and The Hub, and therefore more active in requesting technical assistance, the value of their less quantifiable work has become more apparent.
Lesson 2. Communicating Expectations
CRLs also participate in health promotion, intervention design, and program maintenance. This role has led to the facilitation of new projects or inquiries but has also helped shape how communities have engaged with results and findings. CRLs are often well positioned to frame research results in a practical way that resonates with communities or local organizations. However, in facilitating community dissemination or engaging in new inquiries, CRLs have also found themselves grappling with the somewhat limited scope of research in comparison with community expectations. Although community inquiries can have a narrow scope of health promotion, much of the local interest is often rooted in social justice and structural changes. The negotiation between the scope of research, intervention design, and the community’s long-term goals is rarely in opposition, but CRLs have had to develop skills and language tools to more clearly communicate expectations bidirectionally between community and researchers.
CRLs and the formation of regional advisories are an effective strategy to increase research capacity and respond to community-identified population health priorities. The model consists of four distinct actions: 1) Assess Community Research Engagement Readiness; 2) Implement the Project Assistance Program; 3) Support Community Research Advisories; and 4) Develop Community-Academic Collaborations. The model has been implemented in six rural regions in Oregon. Community research capacity was bolstered by program evaluations, data collection and analyses, dissemination, and implementation research. Programmatic activities ranged from maternal and child health to social inclusion for older adults. As a result of implementing the CRLM, our institution has dramatically increased the number of successful academic–community collaborations, enhanced community capacity to address health-related concerns, and established lasting trusted relationships.
Acknowledgement
We would like to acknowledge the many community members who have worked closely with the community research liaisons over the past 6 years. Without these many individuals and their willingness to engage with our team, this story would not be possible.
We acknowledge the editorial assistance of the Oregon Clinical & Translational Research Institute, which is supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Award Number UL1TR002369.
Disclosures
Authors have disclosed that they do not have any financial conflicts of interest.