Introduction
There is a consensus that diversity in ecology may result in the variation in obstetric morbidity pattern owing to the trade off between energy spent on maternal survival and/or reproduction as well as the quality-quantity continuum between present and future reproduction (Stearns, Reference Stearns2000; Bielby et al., Reference Bielby, Mace, Bininda-Emonds, Cardillo, Gittleman, Jones, Orme and Purvis2007). The state of pregnancy and child birth is a stretch of intense vulnerability and incurs reproductive cost (Bunevicius et al., Reference Bunevicius, Kusminskas, Bunevicius, Nadisauskiene, Jureniene and Pop2009; Schetter, Reference Schetter2011). This reproductive cost becomes steeper if the ecological conditions are sufficiently perilous and unfavourable (Mulder, Reference Mulder, Smith and Winterhalder1992).
Obstetric morbidity, which is one of the prime causes of global maternal death, annually accounts 27 million episodes of direct complications (Graham et al., Reference Graham, Woodd, Byass, Filippi, Gon, Virgo, Chou, Hounton, Lozano, Pattinson and Singh2016); the estimate escalates when indirect complications and long-term sequel are added (Filippi et al., Reference Filippi, Chou, Ronsmans, Graham, Say, Black, Walker and Temmerman2016). The leading causes of severe maternal morbidity or the “near miss” pregnancy are haemorrhage, infection, hypertensive disorders (pre-eclampsia/eclampsia) and prolonged or obstructed labour (Khan et al., Reference Khan, Wojdyla, Say, Gülmezoglu and Look2006; Saxena, Reference Saxena2010; Kassebaum et al., Reference Kassebaum, Bertozzi-Villa, Coggeshall, Shackelford, Steiner, Heuton, Gonzalez-Medina, Barber, Huynh and Dicker2014; Khanam et al., Reference Khanam, Baqui, Syed, Harrison, Begum, Quaiyum, Saha and Ahmed2018). Besides, other morbidities like severe abdominal pain, convulsions, vericose vein, fluid retention, preterm labour, early rupture of membrane and retained placenta may also arise during different stages of pregnancy (Kaur and Kaur, Reference Kaur and Kaur2012; Dutta, Reference Dutta2014; WHO, 2017).
The obstetric transition model based on World Health Organization Multicountry Survey on Maternal and Newborn Health 2010–2012 (WHO MCS) illustrated that India stands in stage III where maternal mortality is still high (MMR 299–50 maternal deaths per 100 000 live births) (Souza et al., Reference Souza, Tunçalp, Vogel, Bohren, Widmer, Oladapo, Say, Gülmezoglu and Temmerman2014). In recent years there has been a decline in maternal mortality rate in this country (Ministry of Home Affairs, Government of India, 2020). So, research and surveillance programmes have shifted their focus on various indices of severe maternal morbidity or “near miss” to capture preciously the life-threatening obstetric conditions that could potentially result in maternal death (Sousa et al., Reference Sousa, Cecatti, Hardy and Serruya2008; Kayem et al., Reference Kayem, Kurinczuk, Lewis, Golightly, Brocklehurst and Knight2011; Urquia et al., Reference Urquia, Wanigaratne, Ray and Joseph2017b).
The cascade of obstetric complications to a great extent is governed within socio-ecological matrix. The interplay of multiple factors (socioeconomic status, religious belief, undernourishment and quality and availability of and accessibility to essential maternal health services) (Zanur et al., Reference Zanur, Loh and Med2006; WHO, 2016; Azuh et al., Reference Azuh, Azuh, Iweala, Adeloye, Akanbi and Mordi2017) affect maternal and child health outcomes, including pregnancies that are “too early, too late, too many, and too close” (Choolani and Ratnam, Reference Choolani and Ratnam1995). Migration, i.e., the exodus of people from one region to another, may lead populations to certain new socio-ecological challenges like in occupational pursuits and stress, nutrition, health care services and so forth. The new socio-ecological challenges could bring variation in reproductive outcome, including obstetric outcomes (Goldstein and Goldstein, Reference Goldstein and Goldstein1983; Little and Leslie, Reference Little, Leslie, Lasker and Mascie-Taylor1993; Nørredam, Reference Nørredam2015). Literature shows that there is a consistent trend for poorer pregnancy outcomes amongst migrant compared to the natives (Kusuma et al., Reference Kusuma, Kumari, Pandav and Gupta2010a, Reference Kusuma, Kumari and Kaushal2013b; Hayes et al., Reference Hayes, Enohumah and McCaul2011; Singh et al., Reference Singh, Rai and Singh2012; Heaman et al., Reference Heaman, Bayrampour, Kingston, Blondel, Gissler, Roth, Alexander and Gagnon2013). For example, a large scale global study elucidated that immigrants were consistently at higher risk of severe maternal morbidity than sedentes (Urquia et al., Reference Urquia, Glazier, Mortensen, Nybo-Andersen, Small, Davey, Rööst and Essén2015a, Reference Urquia, Wanigaratne, Ray and Joseph2017b). A couple of sedente-migrant comparative studies from India showed that Oraon populations living in three different ecologies differed significantly in terms of fertility, maternal health and infant mortality (Mahinder, Reference Mahinder1988; Ghosh and Chakraborty, Reference Ghosh and Chakraborty1997). But other studies showed a reverse trend (Jacquemyn et al., Reference Jacquemyn, Benjahia, Martens, Yuksel, Van Egmond and Temmerman2012; Sudhinaraset et al., Reference Sudhinaraset, Diamond-Smith, Thet and Aung2016).
In India, during late 19th and early 20th century, employment opportunity in tea industries in the Terai (foot hills of the Himalayan Mountain) region resulted in a large scale migration of the tribal populations (mostly Oraon) from their ancestral place Chota Nagpur plateau region (Central India) (Chaudhury and Varma, Reference Chaudhury and Varma2002; Sarkar, Reference Sarkar2013). Now it’s been over 150 years that the migrated Oraon populations left behind their aboriginal group and inhabiting to the new ecology (Terai) almost over four generations.
We hypothesized that women of same ethnic group, living in contrasting socio-ecological niche are likely to have differential obstetric morbidities. Under this backdrop, precisely we asked in our research whether, the obstetric morbidities at three stages: ante and intrapartum and postpartum, and their concomitants differed significantly between sedente and migrant Oraon populations.
Materials and methods
Study area and participants
We conducted this study among a group of Oroan (indigenous) populations inhabiting (a) Ranchi district of Chota Nagpur plateau region, of the state of Jharkand and (b) Jalpaiguri district of Dooars-Terai region, of the state of West Bengal. Ranchi, the capital city of Jharkhand, is the home of more than one third (1042016) of the state’s total tribal population (Census, 2011a). In contrast, district Jalpaiguri, situated at the foothills of the Himalaya Mountains, rank second in respect to West Bengal’s total tribal populations (731704) (Census, 2011b).
The Chota Nagpur Plateau of India is the original abode of the Oraons whose substantial economy is based on settled agriculture. During the colonial period, owing to Colonial land policies and political pressure, the predecessors of this group of Oraons migrated to the district of Jalpaiguri and joined the tea industry as labour force (Chaudhury and Varma, Reference Chaudhury and Varma2002; Sarkar, Reference Sarkar2013). In this study, the Oraon populations inhabiting Ranchi district was considered as the ‘sedente’ group and those lives in Jalpaiguri district as the ‘migrant’ group.
Based upon the numerical dominance of Oraon tribal populations, we considered five Gram Panchayets (GPs) (rural administrative units) under Mandar Community Development Block of Ranchi district and three Gram Panchayets (GPs) under Mal Community Development Block of Jalpaiguri district as our study areas.
403 Oraon participants [203 sedente and 200 migrants] were identified by a door to door survey from the selected GPs of the two districts. The criteria of selection of the participants were: women aged between 15 and 49 years, who were in wedlock at and had at least one child within the last two years from the time of interview. The participation in the study was voluntary in nature.
Data types
We used semi structured schedules to collect information about socio-demographic profile and obstetric morbidity of the participants.
Socio-demographic data included ages of the participants at the time of first conception and first and last child birth (in years), religion, occupational and educational status of the participants and that of their spouses, household size and household assets. Occupational status was categorized into primary [agriculture for sedentes and wage earners in tea industry for migrants] and secondary [working as wage earners in brick kiln, masonry activities, 100 days of wage employment under Mahatma Gandhi National Rural Employment Guarantee Act, 2005 (Ministry of Rural Development, Government of India, 2013)]. Educational status was categorized based on the school system in India: lower primary (completed one to four years of formal education), upper primary (completed five to eight years of formal education), and secondary (completed nine to ten years of formal education). We formulated four groups based on the completion of formal education: non-literate (never received any formal education and/or could sign), up to upper primary level, up to secondary level and above secondary level. The majority of the Oraons (including our sedente participants) living in the Chota Nagpur region reported to follow their traditional belief system and keeps religious faith on sacred grove called Sarna. We considered their religious affiliation as Sarnaism. Few of them reported to have embraced Christianity (due to the influence of Christian Missionaries) and other Hinduism. The migrant Oraons living in Jalpaiguri district do not have traditional sacred grove (Sarna) in their habitat. So, majority embraced Hinduism (owing to their contact with the local Hindu populations) and an appreciable section Christianity.
Data on reproductive variables included parity, reproductive wastage, birth spacing between the last two live births and duration of exclusive breast feeding of the last child. For the purpose of this study we considered 20 ante and intrapartum morbidities (clubbed into one category) and 9 postpartum morbidities. The domain specific list of morbidities is provided in Box 1. All the obstetric morbidities were ascertained following (1) the guidelines recommended for (a) Auxiliary Nurse Midwife (ANM)/Lady Health visitor (LHV) [Ministry of Health and Family Welfare, Government of India (MOHFW, GoI), 2010] and (b) Accredited Social Health Activist (ASHA) worker under National Rural Health Mission (NRHM) [GoI, 2005], (2) the Mother-Child Protection (MCP) card [MOHFW and Ministry of Women and Child Development (MWCD), GoI, 2018], and (3) from the symptom list used in a couple of Indian studies (Mukhopadhyay et al., Reference Mukhopadhyay, Ray Subha, Mukhopadhyay and Bhatia2002; Mukherjee and Dasgupta, Reference Mukherjee and Dasgupta2014). Reporting of antepartum morbidities such as anaemia, hypertension, diabetes, jaundice, malaria and tuberculosis by the participants were cross checked from the documentation of health record on MCP.
Box 1. List of obstetric morbidities

a bleeding from the genital tract at any time after the 22nd week of pregnancy and before the birth of the baby (WHO, 2008)
b profuse, thin, homogenous yellow, white or grey vaginal discharge accompanied with a unpleasant fishy odour
c haemoglobin concentration of less than 11 g/dl (WHO, 2001)
d the new-onset of hypertension that occurred at or after 20 weeks’ gestation with systolic blood pressure ≥140 mmHg and/or a diastolic blood pressure ≥90 mmHg [WHO, 2018; Centers for Disease Control and Prevention (CDC), 2020]
e gestational diabetes (a fasting plasma glucose level >126 mg/dl (7.0 mmol/l) or a casual plasma glucose >200 mg/dl (11.1 mmol/l) (CDC, 2019)
f when spontaneous membrane leakage was reported at least one hour before onset of labour (Caughey et al., Reference Caughey, Robinson and Norwitz2008; Kayiga et al., Reference Kayiga, Lester, Amuge, Byamugisha and Autry2018)
g onset of regular, rhythmical painful contractions accompanied by cervical dilation where labour is longer than 12 hours (WHO, 2008)
h excessive bleeding following delivery of the placenta up to 24 hours (American College of Obstetricians and Gynecologists, 2014); assessed through participants’ recall based on the diagnosis by their health practitioners (You and Zahn, Reference You and Zahn2006).
i all postpartum haemorrhage between 24 hours after delivery and 6 weeks, (WHO, 2008); assessment based on participants’ perception.
Data on utilisation of maternal health services (for the last child) included complete coverage of four recommended antenatal cares (ANCs) [like periodic measuring of body weight, blood pressure and respiratory rate, checking for pallor and oedema and performing abdominal examination (to determine the height of the fundus of the uterus and the foetal position) carrying out diagnostic investigations like haemoglobin estimation and urine tests, administration of two doses of tetanus toxoid injection, providing at least 100 iron folic acid (IFA) tablets, and counselling and advising about diet (nutrition), place of delivery, family planning, in taking rest, monitoring danger signs of obstetric complications, signs of labour, and providing information about the Janani Suraksha Yojana (JSY) programme (safe motherhood intervention under the NRHM [GoI, 2005] to reduce maternal and neo natal mortality by promoting institutional delivery among the poor pregnant women) or any other incentives offered by the state], availing of the first post natal care (PNC) within 24 hours of delivery [first PNC included monitoring of blood pressure, pulse rate, temperature and respiratory rate, checking the presence of pallor, abdominal examination for uterine contraction, examining the vulva and perineum, monitoring vaginal bleeding, examining the breasts for any lumps or tenderness, and managing and counselling on hygiene practice, breastfeeding, nutrition, contraception, IFA supplementation and danger signs of postpartum complications], 48 hours of stay under medical facilities after delivery, coverage of four recommended PNCs [2nd to 4th PNCs included monitoring of blood pressure, pulse rate, temperature, checking for pallor, examining abdomen, breast, vulva and perineum; diagnosis for danger postpartum complications by asking the mother questions like duration of vaginal bleeding after delivery, vaginal discharge with foul-smelling, history of fever, incidence of swelling (engorgement) and/or tenderness of the breast, pain or problem while passing urine; and counselling on post-partum depression (if any), nutrition, rest and contraception] [MOHFW, GoI, 2010], place and mode of delivery including incident of episiotomy (incision made in the perineum to facilitate child delivery).
We considered antepartum period between conception to prior to the initiation of 1st stage of labour; intrapartum period as beginning of the 1st stage of labour to delivery of placenta; and postpartum period as about an hour after the delivery of the placenta to six weeks after birth (WHO, 1998; WHO, 2018).
The entire data was collected by one of the authors (JT) during the period November 2017 to February 2019.
Statistical analyses
Descriptive statistics were used to compare the distribution of socio-demographic, reproductive and health care variables between sedentes and migrants. The distribution patterns of continuous variables were checked using the Kolmogorov-Smirnov test. Data on household size, age of the participants at the time of last childbirth and ages at first conception and first delivery showed skewed distribution; therefore, the median values along with its lower and upper limits were estimated for these variables. Other socio-demographic, reproductive and maternal health care variables were presented in frequency and percentage values. Bivariate statistics such as independent sample t-test, Mann-Whitney U, chi square and Fisher’s exact test were used to compare sedentes and migrants with respect to their socio-demographic, reproductive, maternal health care services and obstetric variables.
Wealth Index (WI) was derived using principal component analysis (PCA) based on the criteria of National Family and Health Survey-4, 2015-16 [International Institute for Population Sciences (IIPS) and ICF, 2017] by considering the following household characteristics and assets: household electrification, drinking water source; type of toilet facility; type of flooring; material of exterior walls; type of roofing; number of household members per sleeping room; cooking fuel; house ownership; land ownership, livestock ownership; ownership of a bank or post-office account; and ownership of a mattress, a pressure cooker, a chair, a cot/bed, a table, an electric fan, a radio, a television, a sewing machine, a mobile phone, a computer, a refrigerator, a watch or clock, a bicycle, a motorcycle or scooter, an animal-drawn cart, a car, a water pump, a thresher, and a tractor. We applied principal component analysis with variables related to household characteristics and assets. The first principal component explains the largest proportion of the total variance, and thus was considered as WI to represent the household’s wealth (Hjelm et al., Reference Hjelm, Mathiassen, Miller and Wadhwa2017). WI was categorized into ‘Lower’ [ ≤ -0.92 (25th percentile)], ‘Middle’ [-0.93 to 1.03 (26th to 74th percentile)], and ‘Higher’ [≥ 1.04 (75th percentile)] based on their respective quartile values.
We estimated the burden of obstetric morbidity of each participant by assigning a score of 1 for experiencing a particular morbidity and a score of 0 for not experiencing a particular morbidity. Thus, the scores for ante and intrapartum morbidities morbidity varied between 0 and 20 and for postpartum morbidity between 0 and 9.
The association between ante and intrapartum morbidities morbidity types and among postpartum morbidity types were analyzed using chi-squared statistics and Cramer’s V was used to measure the strength of the association [weak: >0.05; moderate: >0.10; strong: >0.15; very strong: >0.25] (Zdravkovic et al., Reference Zdravkovic, Osinova, Brull, Prielipp, Simões and Berger-Estilita2020).
Categorical Principal Component Analysis (CATPCA)
We used CATPCA that transformed the large number of correlated socio-demographic, reproductive and maternal health care variables to reduced number of uncorrelated components (PCs). This dimensional reduction method uses “optimal scaling” which generates optimal quantification for categorical variables (Meulman et al. Reference Meulman, Van der Kooij, Heiser and Kaplan2004; van Wietmarschen et al., Reference van Wietmarschen, Reijmers, van der Kooij, Schroën, Heng, Hankemeier, Meulman and van der Greef2011). The percentage of variance (VAF) accounted for each individual component and total component was derived. Criteria like eigen values (reveals how much variance can be explained by its associated eigenvector), component loadings (reflects correlations between quantified variable and its respective component) and value of Cronbach alpha (measures the reliability and internal consistency of a set of data) have been considered for determining the number of components to be selected (Linting et al., Reference Linting, Meulman, Groenen and Koojj2007; Nery et al., Reference Nery, Lidia and Freire2019). Components with eigen values ≥1 (Linting et al., Reference Linting, Meulman, Groenen and Koojj2007; Linting and van der Kooij, Reference Linting and van der Kooij2012), Cronbach’s alpha ≥0.60 (Zhang, Reference Zhang2016), and factor loading ≥0.40 (Maskey et al., Reference Maskey, Jiangang and NGUYEN2018) have been considered for subsequent analysis. The object scores obtained from the four components were used in the subsequent analysis.
We excluded reproductive wastage from the final CATPCA due to its loading less than 0.40.
Multivariate analyses
We applied Poisson regression analysis to find out the risk indicators of ante and intrapartum and postpartum morbidity scores independently (dependent variables). The ante and intrapartum scores showed over-dispersion due to the greater value of the variance than the mean (α >0); and the postpartum score showed under dispersion due to greater value of the mean than the variance (α <0). In order to overcome the dispersed nature of the data distribution, we used generalized Poisson regression (Melliana et al., Reference Melliana, Setyorini and Eko2013; Muluneh et al., Reference Muluneh, Zewotir and Yayeh2016) that can accommodate both over and under dispersion.
Before applying the generalized Poisson regression, we checked whether both the dependent variables (ante and intrapartum morbidities scores and postpartum scores) followed Poisson distribution. The probability function of the generalized Poisson model is presented by
Where y =1, 2,….n and
![]() ${\mu _i} = {\mu _{i\;}}\left( {{x_i}} \right) = exp\left( {{x_i}\beta } \right)$
, where
${\mu _i} = {\mu _{i\;}}\left( {{x_i}} \right) = exp\left( {{x_i}\beta } \right)$
, where
![]() ${x_i}$
is a (k-1) dimensional vector of explanatory variables, and
${x_i}$
is a (k-1) dimensional vector of explanatory variables, and
![]() $\beta $
is a k-dimensional vector of regression parameters. The mean and variance of the generalized Poisson model are given by the following formulae (Famoye, Reference Famoye1993; Wei et al., Reference Wei, Xue and Wang2018)
$\beta $
is a k-dimensional vector of regression parameters. The mean and variance of the generalized Poisson model are given by the following formulae (Famoye, Reference Famoye1993; Wei et al., Reference Wei, Xue and Wang2018)
The four components (PC1 to PC4) derived from CATPCA were used as independent determinants of ante and intrapartum morbidities. For postpartum morbidities, along with the derived scores of CATPCA (PC1 to PC4), variables like place and mode of delivery, timing of receiving the first PNC, duration of stay in the hospital after delivery and number of PNCs coverage were also included as independent determinants. Collinearity for each independent variable was found to be within the range of their respective conditional index, variance inflation factor (VIF>10) and tolerance value (<0.1).
The analyses of the data were done using the Statistical Package for Social Sciences version18.0 (SPSS Inc., Chicago IL, USA). A p-value less than equal to 0.05 (two-tailed) was considered statistically significant.
Results
Both the ante and intrapartum and postpartum morbidity scores were significantly (p ≤ 0.001) higher among the migrants than that of their respective sedente counterparts.
While majority of the sedentes followed their indigenous religion, i.e., Sarnaism, majority of the migrants followed Hinduism and a few of them followed Christianity. The primary occupational pursuit of the sedente participants and that of their spouses was agriculture, but majority of them remain engaged in other secondary occupational pursuits like wage earning. Majority of the migrant participants were wage earners in tea industry, but most of their spouses were engaged in other wage earning pursuits as secondary occupation. Significantly (p ≤ 0.001) more number of migrant participants and their spouses were non literate, belonged to low wealth status and had smaller household size compared to their sedente counterparts.
The reproductive status showed significant (p ≤ 0.05) early ages at first conception, delivery and last child birth, higher parity and shorter birth interval among the sedentes compared to their migrant counterparts. Reproductive wastage and duration of exclusive breastfeeding did not show any significant associations with migration status.
Complete coverage of ANCs and IFA course, incidence of institutional delivery with and without episiotomy and with caesarean delivery, availing of the first PNC within 24 hours, longer stay in the hospital after delivery and more coverage of PNCs were significantly (p ≤ 0.01) higher among the migrant participants compared to their sedente counterpart (Table 1).
Table 1. Distribution of the participants according to socio-demographic, reproductive and maternal health care variables

† 75 sedente and 100 migrant participants’ had singleton birth.
Data are given as mean ± standard error, (lower limit-upper limit); a t test; bMann Whitney U test; cFisher’s exact test; *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001.
The association between ante and intrapartum morbidities morbidity types (Annexure I) and postpartum morbidity types (Annexure II) were significant for overwhelming of the cases.
Categorical principal component analysis
The four-dimensional nonlinear CATPCA analysis is presented in Table 2. The first four independent dimensions (components) were selected based on their respective eigen values (>1). The variance of each component is presented in order of magnitude; component 1 explained 24.05% of the variance (Cronbach’s α = 0.85), component 2 explained 18.59% (Cronbach’s α = 0.76), component 3 explained 15.48% (Cronbach’s α = 0.75), component 4 explained 9.46% (Cronbach’s α = 0.66). The total variance was 67.58%.
Table 2. Results of Categorical Principal Component (CATPCA) analysis of socio-demographic, reproductive and maternal healthcare variables

Each of the variables used in the CATPCA generated a corresponding coefficient representing the relationship of that variable with its corresponding principal component. The components with larger variances are more desirable because they provide more information in explaining variation in the data. Component 1 was highly loaded with “religion and maternal health care” variable; components 2 and 3 with “socio-demographic and reproductive” variables; and component 4 with “socio-demographic and maternal health care” variables. CATPCA generates an object score against each participant for each component. Thus, the derived object scores from PC1 to PC4 were used as independent predictor in the subsequent Poisson regression analysis.
Multivariate analyses
Ante and intrapartum morbidities
It appears from Poisson regression that migrant participants were more likely (p ≤ 0.001) to have experienced ante and intrapartum morbidities than that of the sedentes. Result further shows that the participants who followed Christanity and Hinduism and completed IFA course [bearing PC1] were less likely (p ≤ 0.05) to have experienced ante and intrapartum morbidities, but the trend was reverse for those who followed ‘Sarnaism’ (due to negative loading with PC1). Participants who had higher ages at first conception, first delivery, and last child birth, who and their spouses were involved in both primary and secondary occupations [bearing PC2] were more likely (p ≤ 0.001) to have suffered from ante and intrapartum morbidities. On the contrary, participants and that of their spouses who had higher educational status, participants who had birth spacing for more than two years and breastfed the last weaned child for more than 6 months [bearing PC3], were less likely (p ≤ 0.01) to have experienced ante and intrapartum morbidities, but the trend was reverse for parity (due to negative loading with PC3). Higher wealth index, higher household size and the complete coverage of ANCs [bearing PC4] showed an inverse but near significant association (p = 0.06) with ante and intrapartum morbidities (Table 3, Fig 1A).
Table 3. Concomitants antepartum, intrapartum and postpartum scores: Results of Poisson regression
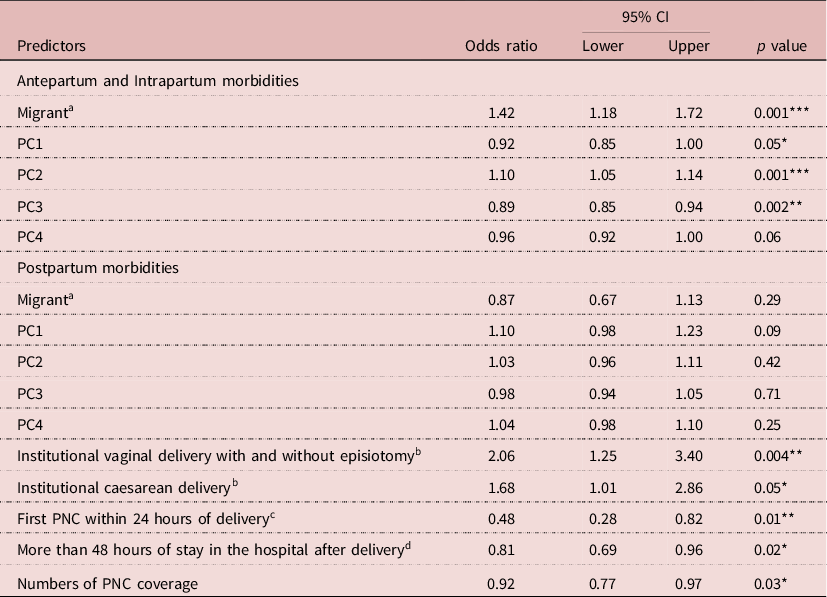
References: asedente, bhome delivery, cfirst PNC after 24 hours of delivery; dless than 48 hours of stay in the hospital after delivery.
*p ≤ 0.05, **p ≤ 0.01,***p ≤ 0.001.

Figure 1. A: Assessing antepartum and intrapartum morbidities based on socio-demographic, reproductive and maternal health care variables in a Poisson regression model (CI 95%). B: Assessing postpartum morbidities based on socio-demographic, reproductive and maternal health care variables in a Poisson regression model (CI 95%).
Postpartum morbidities
The same table (Table 3) shows that neither migration status nor any of the PCs could significantly predict postpartum morbidities. But variables that signify direct availing of maternal health care services during and after delivery significantly predicted postpartum morbidities. For example, participants who delivered their child in health institutions and had episiotomy during the vaginal birth and/or had caesarean delivery were more likely (p ≤ 0.05) to have experienced postpartum morbidities. On the contrary, participants who availed the first PNC within the 24 hours of delivery, stayed under medical supervision after delivery for more than 48 hours and had higher coverage of numbers of PNC were less likely (p ≤ 0.05) to have experienced postpartum morbidities (Fig 1B).
Discussion
Studies worldwide postulated that differential socio-ecological set up may bring variation to the maternal health of the migrant than their original population (Ellison, Reference Ellison2003; Mascie-Taylor and Little, Reference Mascie-Taylor and Little2004; Nørredam, Reference Nørredam2015). Our study observed that migrant participants were at the risk of experiencing majority of the obstetric morbidities compared to the sedentes.
Growing evidences suggest that unfavourable reproductive parameters could promote adverse maternal health outcome. For example, childbirth at a young age entails trade off between physiological development of the young mother and her reproduction; recurrent pregnancies predispose the mother to poor nutritional state at the expense to feed the children from her own share; shorter birth interval, i.e., less than 24 months (WHO, 2005) may cause nutritional and folate depletion, suboptimal lactation for the newborn, cervical insufficiency, infections and incomplete healing of uterus of the mother (Ellison, Reference Ellison2003; Teguete et al., Reference Teguete, Maiga and Leppert2012; Njoku et al., Reference Njoku, Abeshi and Emechebe2017). Together, these factors may lead to several maternal complications like haemorrhage, gestational anaemia, diabetes and hypertension, prolonged and obstructed labour, premature rupture of membranes and delivery, cephalopelvic disproportion, uterine inertia, and so forth (Klein, Reference Klein2005; Shechter et al., Reference Shechter, Levy, Wiznitzer, Zlotnik and Sheiner2010; Agrawal et al., Reference Agrawal, Agarwal and Das2011; Utting and Bewley, Reference Utting and Bewley2011; Mgaya et al., Reference Mgaya, Massawe, Kidanto and Mgaya2013). Multivariate analysis of our study shows advanced ages of first conception and delivery, shorter birth interval (PC2-3), and multi parity (due to the negative correlation with PC3) increased the risk of having ante and intrapartum morbidities. Interestingly, migrant participants despite having higher ages of first conception and first and last deliveries, higher birth spacing, and availing more maternal health care facilities compared to the sedentes, experienced more obstetric morbidities.
The Government of India (2005) and WHO (2015b) recommends four antenatal [within first three months, followed by in 4th-6th, 7th-8th and 9th month of pregnancy] and postnatal [within first 24 hours, followed by at 2-3 days, 6-7 days, and 6 weeks after delivery] visits that serve immediate beneficial purpose to a pregnant woman and the subsequent mother. Multivariate analysis of our study revealed similar trend by displaying reduced risk of experiencing higher rate of ante and intra and postpartum morbidities by those who had more coverage of ANCs or PNCs. But intriguingly, despite having significantly higher coverage of recommended number of ANCs and PNCs, migrants reported morbidities more frequently compared to the sedentes.
The Government of India (2005), based on the following criteria: institutional delivery, fertility and mortality rates, immunization, family size and income has divided the states of this country into two categories- low performing states (LPS), such as Jharkhand and high performing states (HPS), such as West Bengal. So, the likelihood of reporting of obstetric related morbidities (especially gestational anaemia, hypertension and diabetes, premature rupture of membrane and prolonged labour which are defined medically and are often detected by routine health screening during pregnancy) would be more for people living in HPS. This could be a reason why the migrants (living in HPS) of our study reported obstetric morbidities in higher frequencies compared to sedentes. The livelihood pattern of the migrants could be another reason behind higher reporting of obstetric morbidities.
In course of fieldwork among the migrants, the first author (JT) had the opportunity to closely interact with the participants and observe their everyday life. It appeared from these interactions that the life of the migrants is imbued with despair and uncertainty with their livelihood. Unlike the sedentes, majority of the only occupation of the migrant participants is wage earning in tea industry throughout the year. The daily wages received is miserably low; the permanent workers in the tea garden earn 3500 (INR) per month, and those who are engaged in plucking of tea leaves only during the months April to October earn around 2000 (INR) per month. Even during pregnancy, the nature of their job compel them to pluck tea leaves from the garden, carrying the load of basket filled with leaves (approximately of 20 kg weight) for prolonged hours of time and at the end of the day walking long distance carrying this load to the tea processing site. Since permanent workers entitled to two-three months’ maternity leave (duration varies between gardens) with deduction of half of their daily wage, and non-permanent workers have to leave employment altogether, the participants continue to work till their eighth to ninth month of pregnancy period and resume the work within couple of days after delivery to sustain their families.
Exclusive breastfeeding of the last weaned child was found to decrease the severity of ante and intrapartum morbidities in the subsequent pregnancy. Epidemiological studies suggest that during pregnancy, the placental hormones with anti-insulin effect increase the risk of cardiovascular and lipid metabolisms (Schwarz et al., Reference Schwarz, Brown, Creasman, Stuebe, McClure, Van Den Eeden and Thom2010; Dieterich et al., Reference Dieterich, Felice, O’Sullivan and Rasmussen2013). Conversely, lactation is associated with favourable metabolic changes in terms of insulin-sensitivity, lipid metabolism and blood pressure (Stuebe, Reference Stuebe2009). The “Reset Hypothesis” (Stuebe and Rich-Edwards, Reference Stuebe and Rich-Edwards2009) proposed that these favourable metabolic changes persist even after weaning and brings benefit for the subsequent pregnancy. Therefore, women, who breastfed the last weaned child for a longer duration were less likely to develop adverse metabolic risks like type 2 diabetes, hyperlipidemia and cardiovascular disease in their subsequent pregnancies (Schwarz et al., Reference Schwarz, Ray, Stuebe, Allison, Ness, Freiberg and Cauley2009; Natland et al., Reference Natland, Nilsen, Midthjell, Andersen and Forsmo2012; American College of Obstetricians and Gynecologists, 2016). For migrants, managing exclusive breastfeeding even for six months was difficult. Due to lack of the available maternity leave, they are compelled to wean their child early and join work leaving their children under the supervision of elderly family members and/or younger siblings. But, this is not the case for the agricultural sedentes.
Moreover, lack of proper housing facility, inadequate supply of clean drinking water, absence of proper sanitation facilities and high prevalence of undernourishment [record from MCP (MOHFW and MWCD, GoI, 2010)] are some of the major obstacles the migrants face towards leading a healthy life. MWCD, GoI, (1975) launched Integrated Child Development Services (ICDS) where food supplements of 600 calories of energy and 18-20gms of protein per day in the form of micronutrient fortified food and/or energy dense food as take home ration are given to the pregnant women and lactating mothers. Majority of the migrant participants reported that managing time to bring the cooked food from the ICDC centre and be attentive to their diet during pregnancy and lactation was not easy for them. Finishing household chores, feeding their family and children at the earliest to present in duty on time, several times resulted in skipping of breakfast or lunch or eat poor nutritious diet even during pregnancy.
The sedentes, in contrast are primarily dependent on agricultural practices, which provided them security in livelihood and a liberty to some extent to manage time in taking care of their health during pregnancy and postpartum phase. Since they are indigenous populations and settled in their own land, the government of the state provided them with concrete housing, sanitation facilities, safe drinking water and variety of seeds, fertilizers and agricultural equipments. They grow vegetables in their homestead land, which provides a steady supply of nutrient in their diet. Therefore, better socio-demographic indicators like higher educational (PC3) and wealth status and larger household size (PC4), which were significantly higher among the sedentes, might have reduced their risks of having ante and intrapartum morbidities compare to the migrants.
The effectiveness of health care does not depend solely on the number of available health institutions or the natal visits that are offering ANC or institutional delivery or PNC, but also on the quality of the health services being offered, strong referral services, adequate medical supplies, diagnostic supports and attitude and expertise of the health professional (WHO, 2015a). It was observed in course of field work that although there are a number of public health institutions in the area where the migrants live, yet the services available in these health institutions are inadequate.
The absenteeism of the health care providers in the health institutions, inadequacy in the supply of medicine [IFA, calcium and vitamin tablets] or defunct diagnostic instruments [instruments for measuring body weight and blood pressure or conducting serological tests like haemoglobin and blood glucose levels] were the frequently reported complains by the migrants against the available Government’s health facilities. As per the guidelines of the Ministry of Health, Government of India (MOHFW, GoI) (2012), health centres are supposed to remain open on all working days for providing out patients services, and out of the two appointed Auxiliary Nursing Midwifery (ANMs), one should always be available in the health sub-centre. But in reality many centres remain close for several days in a month along with frequent absenteeism of the health personnel.
The complete coverage of IFA supplementation (PC1) were found to reduce the risk of ante and intrapartum morbidities; but despite significantly more number of migrants availed the full coverage of the facilities compared to the sedentes, the former group experienced majority of the morbidities. The records of MCP card showed anaemia was much prevalent among the migrants during their pregnancy. National iron plus initiative (MOHFW, GoI, 2013) recommends iron folic acid supplementation [one IFA tablet] of 100mg elemental iron and 500μg of folic acid every day for at least 100 days of gestation followed by the same dose for 100 days postpartum for the non-anemic pregnant women. But for those who are anaemic [haemoglobin level <11 gm/dl or <7 gm/dl], two tablets per day or multiple dose of IFA supplementation are required, followed by monthly assessment of haemoglobin levels. It was reported that the health centres provide only 100 tablets even to the severe anaemic participants; and do not conduct diagnostic test for anaemia or provide IFA supplementation during the post partum period.
It was frequently reported by the migrants that there is delay in the arrival of ambulatory services and ASHA workers when they are in labour. As a consequence, many deliveries either took place in the home or on the way towards hospital. It is recommended that in emergency cases, ANMs are supposed to supervise home deliveries as skilled birth attendant and should arrive at the home within 30 minutes of onset of the labour [NRHM, (GoI, 2005)], but none of the home delivery was reported to have supervised by them. Most of the home deliveries of the migrants were performed by either traditional birth attendants or in some cases the family members. Even in some cases ASHA workers visited the participants first time a couple of days after delivery.
Since institutional deliveries and postpartum morbidities were significantly higher among the migrants than the sedentes, supposedly, the migrants would have lesser postpartum morbidity; but the trend is reverse in our study. The probable reasons could be the higher incidences of episiotomy in institutional delivery. The migrant participants reported that in the public health institutions, except caesarean section, almost all deliveries were performed by the nurses. And in most of the cases the nurses make perineal incisions or episiotomy which is not even recommended until necessary and is known to be the risk of many serious postpartum complications like perinial lacerations, perineal pain, wound site edema, genital tract hemorrhage, urinary and/or anal incontinence and dyspareunia, haematoma, chronic infections etc. (Gün et al., Reference Gün, Doğan and Özdamar2016; Fukami et al., Reference Fukami, Koga, Goto, Matsuoka, Tohyama, Yamamoto, Nakamura, Koyanagi, To and Kondo2019).
Into the bargain, the performance of the health personnel in many cases was not satisfactory. It was narrated by one of the migrant participants: “During my ANC visits, I got to know from ultrasonography (USG) report that I am pregnant for twins. When I was in labour my husband took me to a public health institution. But in a hurry, he forgot to carry my USG report. The ASHA worker who visited my home after the onset of my labour did not even remind me to carry the USG report to the hospital. A nurse performed the delivery of my child informed that I gave birth to a boy child. I promptly asked her about the other one. In reply she said that I carried a singleton pregnancy. She denied accepting the argument of me and of my husband that the USG report suggests twin pregnancy. She kept pushing and pressuring my abdomen repeatedly and later inserted her hand through my birth cannel and manually searched for the other undelivered child. When my husband started shouting at the nurse to stop this exercise, some other doctor then came around and finally helped in delivering my second child”(Source: Field data).
Majority of the postpartum morbidities considered in our study are theoretically associated with the ‘safety’ during delivery. Quality health services during postpartum period are likely to reduce the occurrence of intra- and postpartum morbidities. The initial 48 hours after childbirth are crucial for monitoring the health of the mother because majority of maternal deaths due to post-delivery complications like excessive bleeding, postpartum infections etc. occur during this period (WHO, 2015a). Many fatal complications cannot be predicted previously therefore professionally trained midwifery care is indispensable to handle such complications when they arise. Evidence suggests that the implementation of JSY resulted in a gigantic increase in institutional births (from 39% to 79%) and receiving first PNC within 48 hours after delivery (from 37% to 65%) between the periods 2005–06 to 2015–16 (IIPS, 2017). But these developments did not help in the decrease of maternal morbidities to the same extent. The sedente participants who underwent institutional delivery reported that except for caesarean births or in the case of serious complications, the hospital authority discharges a woman within a day or sometimes within hours after the delivery, unlike their migrant counterparts who remained under the medical supervision at least for 48 hours following the delivery. Thus, the likelihood of receiving quality PNC from health institutions is more among the migrants. The sedentes, on the other hand, who reported home deliveries in high frequency, are likely to have been visited by the ASHA workers with limited resources after delivery. Therefore, the migrants are supposedly less likely to experience postpartum morbidities compared to the sedentes; but reverse was the trend. Availability of medical facilities to provide comprehensive emergency care is insufficient in the public hospitals where the delivery of the migrants took place. It was frequently reported by the migrant participants that until they complain or sought for medical assistance, the nurses did do not attend. It was further reported that in most cases, ASHA workers escorts the pregnant migrant woman who is on labour only up to the public health centres. But as per the recommendations of GoI (2005), the ASHA workers are suppose to stay with the pregnant woman throughout the process of delivery and during the immediate post-partum period to ensure that the mother and the newborn are receiving medical attention by the medical officer and nurse at least twice a day. Moreover, in several cases if, ASHA visited the home for PNC, they don’t present in home because of not losing a day’s wage.
The maternal health services availed by the sedentes who lives in the LPS, are also not appreciable. Lack of sufficient public health centres with respect to the population size (MOHFW, GoI, 2012), inadequacy of quality infrastructure, including physical infrastructure, equipments, medicines and First Referral Units (FRU) for high risks obstetric complications, shortage of trained medical manpower, poor availability of treatment, and the uncooperative nature of health providers are the challenges which hinders the sedentes to avail a quality-based health facilities.
However, despite living in the high performing state, the inside stories of the tea garden workers, the migrants, were much vulnerable compared to the sedentes. Living in isolation and remote areas from mainstream of the state with the substantial economic hardship, meagre alternative means of livelihoods and burden of the recalcitrant nature of the plantation managements, make them more susceptible to maternal morbidities. Somehow they manage a couple of days to go for the ANCs, but for other maternal complications, which were much prevalent among them, they lack seeking health care, because cost of being sick is substantial: loss of wage. This is not to suggest that there is no action by the state government for the plantation workers, especially for the women. However, due to the lack of coordination between the government authorities and the tea garden managements, the approach to address women’s health remains typically piecemeal, episodic, and do not catalyse the agency of workers themselves to take a holistic actions to act on the social determinants of maternal health.
This study could be viewed under certain limitations. The bargain of inhabiting in the Sub-Himalayan region (habitat of the migrants) where malaria is endemic [malaria parasites severely known to cause red blood cell rupturing (barring heterozygous condition for sickle gene)] (Murthy et al., Reference Murthy, Sahay, Srinivasan, Upadhaya, Shantaram and Gayatri2000), plausibly made the migrants vulnerable to anaemia and its associated conditions like fever, fatigue and dizziness. On the contrary, living in regions where anaemia, malaria and other infectious conditions are not endemic, might have lessen the obstetric morbidies among the sedentes. More comprehensive study in the future could further elucidate this complex relationship. Since the study is based on self reported morbidities, assessment of morbidities like gestational anaemia, hypertension, and diabetes, premature rupture of membrane and prolonged labour through medical intervention would have provided more precise insights. Inclusion of data on nutrition of the pregnant women and lactating mothers and the perception of the health providers regarding lacuna of the availability and accessibility of the health services would have provided a better insight of the maternal adverse health complications.
There is paucity in research related to obstetric morbidities and its concomitants in the context of sedente-migrant. Therefore, there is a need for larger prospective research to address the complex relationship between contrasting socio-ecological context and maternal morbidities.
We conclude that the maternal obstetric morbidities and their concomitants differed between sedente and migrant Oraon populations owing to their living in differential socio-ecological contexts.
Data sharing statement
The study is based on the data collected for a doctoral dissertation. Since the doctoral dissertation is yet to be awarded, the authors would prefer not to share the data for public access.
Acknowledgements
We are indebted to all the study participants who have volunteered to participate in the study and wish to express our gratitude for their extend cooperation. We are thankful to the University Grants Commission, India [Ref no. 10985/(NET-DEC.2014)] for providing the financial support in conducting the research.
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.







