Background
At the end of 2019, the new coronavirus disease 2019 (COVID-19) was discovered in Wuhan, China, and quickly evolved into a serious epidemic outbreak (Lu et al., Reference Lu, Stratton and Tang2020). After that, COVID-19 spread rapidly around the world, becoming a public health emergency. According to the World Health Organization (Reference OrganizationOrganization), more than 61 million people worldwide have been infected with COVID-19 by 30 November 2020, and more than 1.4 million people have died.
As the epicenter of the COVID-19 pandemic in China, Wuhan was heavily burdened on the city's medical system. In order to solve the problem of insufficient beds in the designated hospitals and accelerate the admission of patients, many Fangcang shelter hospitals (FSHs) had been opened (Chen et al., Reference Chen, Zhang, Yang, Wang, Zhai, Bärnighausen and Wang2020) since 5 February 2020 in Wuhan. FSHs were temporary medical facilities that converted from public venues, such as stadiums and exhibition halls, to isolate and care for patients with mild or moderate symptoms of COVID-19. A total of more than 12 000 confirmed COVID-19 patients had been treated in FSHs (Shu et al., Reference Shu, Ji, Chen and Feng2020), which played a crucial role in the prevention and treatment of COVID-19 (Zhou et al., Reference Zhou, Wang, Wang, Cheke, Xiao and Tang2020; Wang et al., Reference Wang, Gao, Song, Huang, Wang, Wu, Yuan, Li, Cheng and Cheng2020a, Reference Wang, Tang, Yang, Ma, Bai, Cai, Ma, Zhao, Wang and Liu2020b).
COVID-19 had caused mental health impacts on both the patients and the medical health workers. The patients with confirmed or suspected COVID-19 experienced fear of the consequences of infection, and also boredom, loneliness, and anger (Xiang et al., Reference Xiang, Yang, Li, Zhang, Zhang, Cheung and Ng2020) in their quarantine. The frontline medical workers were also heavily pressured by risk of infection, inadequate protection, overwork, lack of contact with their families, and exhaustion (Kang et al., Reference Kang, Li, Hu, Chen, Yang, Yang, Wang, Hu, Lai, Ma, Chen, Guan, Wang, Ma and Liu2020a). A cross-sectional study (Kang et al., Reference Kang, Ma, Chen, Yang, Wang, Li, Yao, Bai, Cai, Xiang Yang, Hu, Zhang, Wang, Ma and Liu2020b) of 994 medical workers in Wuhan found that about 63% of them had mental health problems.
Since the FSHs are greatly different from the designated hospitals on patient populations and environments, it is necessary to explore the mental health status of the patients and staff in FSHs. The previous quantitative studies (Dai et al., Reference Dai, Wang, Jiang, Li, Wang, Wu, Jia, Liu, An and Cheng2020; Gu et al., Reference Gu, Zhu, Xu, Xi and Xu2020; Li et al., Reference Li, Yang, Zhang, Wang, Wang, Dong, Wang, Wei, Li and Zhang2020) focused on psychological symptoms of the participants, but did not include their experiences, feelings, needs, or the effects of some external factors. Therefore, in the study, mental health needs are defined as all self-reported thoughts and needs that may be related to mental health. Qualitative design is adopted to explore various mental health needs of the COVID-19 patients and the staff with different occupations in the FSH, so as to develop recommendations for the mental health service, FSH management, and policy making.
Method
Study design, setting, and participants
Qualitative research can improve the description and explanation of complex, real-world phenomena such as mental health needs (Bradley et al., Reference Bradley, Curry and Devers2007). In this study, semi-structured interviews were conducted and reported following the consolidated criteria for reporting qualitative research (COREQ) standards (Tong et al., Reference Tong, Sainsbury and Craig2007).
The face-to-face interviews were carried out in the EastWest Lake Fangcang Shelter Hospital. The interviewer (CWL), who worked in the hospital as a member of the Psychological Assistance Team from JiangSu, obtained permission for interviews from the management. The EastWest Lake Fangcang Shelter Hospital was one of the first three FSHs built in Wuhan and began to accept COVID-19 patients, mainly of mild symptoms, from 7 February 2020. There were 1440 beds, three wards, and several departments including medical, nursing, pharmacy, and radiology. The highest number of patients in the hospital was 1434 and the total number including all the staff was more than 3000 (Reference RadioRadio). The medical workers in the hospital were mainly from the assistance teams of Xinjiang, Ningxia, Guangdong, and Fujian.
The confirmed COVID-19 patients and the staff that aged more than 18 years and stayed more than 1 week in the hospital received our verbal invitation. And the individuals who responded to our invitation formed a convenience sample. They were asked to talk about their experience in the FSH after giving the informed consents. All the interviews took place in independent spaces.
Data collection
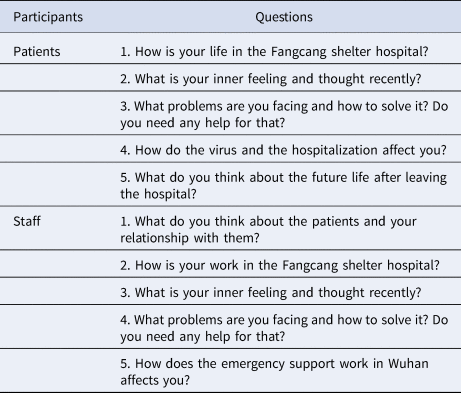
The semi-structured interview outlines (Table 1) were completed and modified under the guidance of specialists in infectious diseases, psychiatry and psychology. We then conducted pre-interviews and make several adjustments to the problem descriptions.
Table 1. Semi-structured interview outlines
According to arrangement of the hospital, the interviews were carried out on 7 March 2020, the day before the hospital was officially closed. The participants reconfirmed the informed consents, including their permission of recording and transcribing the interviews, and then filled out a short survey of demographic, physical, and mental information before the conversations.
Although the interviews were semi-structured, the method of grounded theory (Corbin and Strauss, Reference Corbin and Strauss1990), a qualitative approach that could help finding out structural patterns from human experience, was fully applied in the process. According to grounded theory, all meaningful issues emerging in the previous interviews should be incorporated into the current one, and specific regularities and patterns should be found and verified. In every interview, we tried to validate previous findings and looked for new relevant factors. The conversations continued until the interviewer found no new meaningful viewpoints emerging.
A total of 19 interviews were completed, with 23 participants (10 patients and 13 staff). All the 10 patients and six staff were interviewed individually, and the rest seven staff were interviewed in 2–3 persons. They worked together in the hospital. In the interviews, they complemented and contrasted the answers of one another.
Data analysis
The audio recordings were transcribed verbatim and checked for accuracy. All the thoughts, emotions, and demands of the participants in the 19 completed interviews were included in the data analysis.
The analysis was also based on grounded theory (Corbin and Strauss, Reference Corbin and Strauss1990). Using the method of open coding, three researchers (JL, CWL, and QYW), including the interviewer, openly identified the data into concepts with practical meanings, and then compared, combined, and classified the concepts to generate codes. A structured codebook was developed as dataset of the inductive codes. In the coding seminars of the research team, the codebook was supplemented and modified until no new codes were proposed. The thematic analysis was then performed using the similar comparative analytic process used to produce codes, which was a key component of grounded theory. The generated themes and subthemes were reviewed and examined for rigor before making a list. We made connections to the themes, and all the connections were repeatedly verified, so that a theoretical framework was finally established.
The results of transcription and coding were checked and confirmed by the participants. No qualitative software was used.
Results
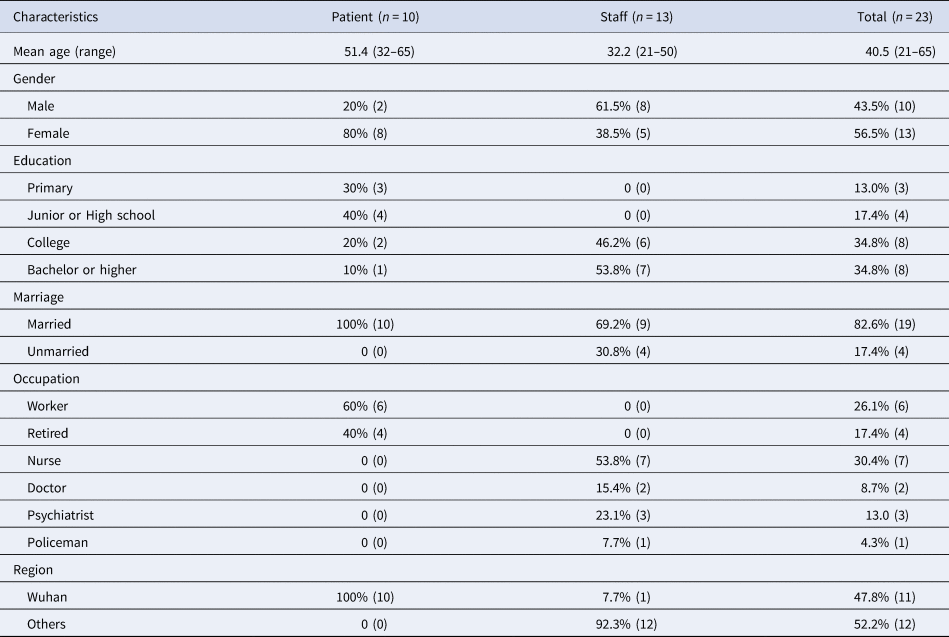
The demographic characteristics of the 23 participants are shown in Table 2. The average age of the patients was 51.4 years. About 80% of them were women, and all of them were Wuhan natives. Meanwhile, the average age of the staff was 32.2 years, with different professions including nurse, doctor, psychiatrist, and policeman. About 38.5% of them were women, and only 7.7% of them were Wuhan natives.
Table 2. Demographic characteristics of the participants
The semi-structured interviews brought three perspectives, including self-reported needs of the patients and the staff, as well as the patient needs from the staff's perspectives. Exemplary quotes were used to illustrate the four themes and night subthemes (Table 3) that developed from the analysis. A thematic framework (Fig. 1) was established to summarize the themes and describe the relationship among them.

Fig. 1. Theoretical framework.
Table 3. Exemplary quotes supporting themes and subthemes

Basic needs
This theme included the largest number of codes related to survival, health, and life.
‘I can only sleep for two or three hours here. I don't have enough energy during the day and I feel my body uncomfortable’. —Participant 7
Quality of life was a common need of the patients and staff. Due to the gathering people and facility conditions of the hospital, many patients had sleeping problems, including difficulty in falling asleep, reduced sleep duration, and irregular sleep pattern. The staff also reported sleeping problems. Many of them had taken sleeping pills for that, and some took the pills frequently or even every day. Another concern was the inadequate daily necessities in the hospital. Many materials had to be purchased outside, which usually took a long time. Besides, some patients, especially elderly ones, required some life care like helping them moving heavy things or finding someone.
‘When I first came here, I was worried that cross-infection would happen between so many people… Now I have no symptoms or other health problems’. — Participant 4
Disease recovery was another basic need for the patients. In addition to their current health, they also reported concerns on their transfer, quarantine, and subsequent treatment. Many patients had the worry that the cross-infection among people would affect their recovery, while those who did not meet the discharge criteria worried to be transferred to the designated hospital with severe pneumonia patients. Meanwhile, discharged patients would have to be quarantined in community for 14 days that might be too long for some of them. Other patients also focused on their subsequent treatments, recurrences, and sequelae.
‘I was afraid to put on and take off the protective gowns by myself at first… Now it's no more a problem because there are specialized staff responsible for guiding and helping us’. — Participant 16
Working in the FSH was a great challenge for all the staff, with work and prevention support one of their basic needs. One problem that troubled many staff was putting on and taking off protective gowns, so the hospital arranged responsible staff to guide and help them. They also reported that they were not so adapted to their work in the protective gowns at the beginning, as it was difficult to talk or perform medical operations. As to the current working hours, most staff thought them appropriate, while some of them worked heavily when the FSH was newly established.
Information and communication
‘No one came to us or talked to us, telling us where we should go today. I did not know that until I asked them myself today’. — Participant 8
The interviewed patients thought it very necessary for them to obtain some important information in advance from the hospital, such as the arrangement of discharge or transfer, so that they had enough time to prepare. But sometimes the information might be sent quite late or even wrongly.
‘We received doubts from one patient time and again… He repeatedly doubted the air, disinfection, etiology, and other professional things, and he never understood or accepted our explanations’. — Participant 19
Communication was a critical element in hospitalization. Most of the patients had got enough communication, care, and assistance from the staff, while two of them thought that their doctor or nurse were sometimes impatient to them. For the staff, communicating with patients was part of their work, but sometimes they had to be pestered or doubted frequently by some of them, that took them a lot of time to deal with. Moreover, the rapid increase of patients and the lack of staff in the early stage of the hospital had caused difficulty in patient management.
Emotional needs
This theme included all the emotions and related behaviors of the participants.
‘I didn't know how I got infected… To tell the truth, I had some negative thoughts about this disease. I felt there no way for me’. — Participant 2
Both the patients and staff had to deal with their bad emotions. As for the patients, the emotions included anxiety, depression, stigma, and worry. The first two were often described as ‘irritable’ or ‘hopeless’, and occurred in the early stage of infection. The stigma was the feeling of shameful or guilty for the disease, while the worry was mainly about their families, especially those who were also infected, and children or elderly people who lacked care. For the staff, anxiety, fear for infection, and stress from work were the most common negative emotions. These emotions were often hidden and only a few of them asked for help from their psychological or psychiatric colleagues.
‘Positive guidance will be very helpful here. For example, our colleagues from the Xinjiang medical team organized folk dances, as reported on CCTV News’. — Group of Participants 20, 21, 22
Emotional intervention and rehabilitation, on the other hand, were the attemption to improve positive emotions. From the experience of the interviewed staff, emotional outbreaks might happen on some relatively fragile patients, that could cause conflicts or even violence. They suggested that more attention and care should be paid on the emotional states of the patients, so as to detect those outbreaks from the beginning and prevent them from causing conflicts. Positive emotional promotion might also be effective for the psychological rehabilitation of the patients, especially those mild patients who got few medical treatments from the hospital.
Social support
‘I worked in a landscaping enterprise and I'm not sure they would allow me returning to my used position’. — Participant 1
Returning to normal life and work was a great desire for the patients, although they thought the process not easy. Many of them were not optimistic that their employers and colleagues, communities, and neighbors would treat them in normal manners. They believed returning to work would be even harder than returning to community life for them, as the employers might make them long-term off work or even unemployment. They noted that relevant policies should be made and implemented to protect their rights of work and life, and also eliminate the discrimination.
‘When I came here, I brought the blanket myself. My families also brought blankets to their isolated places. After returning home, we will have no blankets to sleep on’. — Participant 6
The need of financial and life support was not mentioned by the interviewed patients but by the staff. They told us that the hospitalization was costly and many patients with mild symptoms would refuse to be hospitalized at their own expense, so the financial support from the government greatly improved the centralized isolation and prevention of the infectious disease. They also reported life support necessary for the patients, including the supplies, facilities, and logistics from the society.
External factors
‘The lights are too bright here at night, a major reason why many people can't fall asleep’. — Participant 4
In addition to the above internal needs, we also found some external factors, including hospital facilities and management, psychological support and intervention, social acceptance and support, as well as policy making and implement. In a closed place for centralized isolation like the FSH, internal needs of the individuals were regulated by these external factors, and eventually affected their mental health. For example, many participants believed the too-bright light in the hospital night was a main reason of their sleeping problems. This defect in quality of life made effect on their mental health.
Discussion
To our knowledge, this is the first qualitative study on mental health needs of the COVID-19 patients and the staff in FSHs during the pandemic of Wuhan. The present study reports the perspectives of the participants to fill the research gap of mental health needs. We also try to find objective requirements which are connected with many aspects of mental health work from the subjective results. These findings may provide a theoretical basis for other makeshift hospitals or temporary isolation places during COVID-19.
Mental health needs
Basic needs of the patients and staff is one of our concerns. As temporary health facilities for the infectious disease, FSHs had complete infrastructure, adequate resource supply, systematic prevention, and management (Chen et al., Reference Chen, Zhang, Yang, Wang, Zhai, Bärnighausen and Wang2020). Quality of life of the participants, however, involved some overlooked details, such as necessity purchase and life care. Life care service stations and staff can be very helpful for that. Similarly, medical information service stations can also be helpful, not only for patients to eliminate the anxiety of unknown, but also for medical staff to relieve some work burden. The FSH also placed emphasis on the prevention support for the staff, so that ‘zero infection’ had been achieved (Zhang et al., Reference Zhang, Wang, Yu, Sun, Lei and Wu2020a) during the whole medical activities in COVID-19. The long working hours, however, had caused job stress (Zhan et al., Reference Zhan, Ma, Jian, Cao and Zhan2020) to the staff. More effort should be made by the hospital management to establish a complete work support system.
The emotional and psychological results are consistent with the previous researches (Bo et al., Reference Bo, Li, Yang, Wang, Zhang, Cheung, Wu and Xiang2020; Zhu et al., Reference Zhu, Xu, Wang, Liu, Wu, Li, Miao, Zhang, Yang, Sun, Zhu, Fan, Chen, Hu, Liu and Wang2020; Kang et al., Reference Kang, Li, Hu, Chen, Yang, Yang, Wang, Hu, Lai, Ma, Chen, Guan, Wang, Ma and Liu2020a; Li et al., Reference Li, Yang, Zhang, Wang, Wang, Dong, Wang, Wei, Li and Zhang2020; Zhang et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng, Min, Tian, Leng, Du, Chang, Yang, Li, Shangguan, Yan, Dong, Han, Wang, Cosci and Wang2020b). Due to social isolation, perceived danger, physical discomfort, fear of cross-infection, and uncertain future, patients with COVID-19 often experience anxiety, depression, stigma, worry, insomnia, and posttraumatic stress symptoms, which cause harm to their social functioning and quality of life, and even lead to mental disorders (Rogers et al., Reference Rogers, Chesney, Oliver, Pollak, Mcguire, Fusar-Poli, Zandi, Lewis and David2020). For these emotional and psychological problems, Mukhtar proposed a Health Belief Model (Mukhtar, Reference Mukhtar2020) that emotions and health-related behaviors of individuals could be predicted and explained by their perceived stress, coping strategies, and some external factors. Therefore, it is necessary to improve the mental health work. Unlike general health facilities, FSHs also served as social space that provided necessary emotional support and social participation (Chen et al., Reference Chen, Zhang, Yang, Wang, Zhai, Bärnighausen and Wang2020) to the patients. They supported one another and participated in social activities. For example, the EastWest Lake Fangcang Shelter Hospital where our interviews took place had been reported many times by the media (Reference NewsNews) for the group XinJiang folk dance. Other activities included watching TV and reading (Reference DailyDaily C).
The relationship between the COVID-19 patients and the medical workers was seldom reported in previous studies, but we found that both of them thought the relationship important. The patients needed care, patience, and assistance from the staff, while the staff needed to manage a large number of patients, as well as deal with some doubts and conflicts.
In addition to the internal relationship, the social relationships outside the hospital were also great concerns for the patients. COVID-19 patients suffer severe stigmatization, especially in the workplace (Dang et al., Reference Dang, Le, Le, Tran, Do, Phan, Nguyen, Pham, Ta, Nguyen, Van Duong, Hoang, Pham, Nguyen, Vu, Latkin, Ho and Ho2020). Returning to their normal work and community life is difficult for them, so that policies should be made to protect their rights. Financial support, especially medical costs, was another important need of the patients, as well as the key that many individuals afford to receive treatment in the FSH. The medical bills of confirmed inpatients in China were RMB23 000 per person (China TSCIOOTPSRO), most of which were paid by the government.
The theoretical framework established from our findings indicated that the external factors regulated internal needs and thus affected mental health, which was consistent with the previous model. It is the first time, to our knowledge, to be proposed in the mild COVID-19 patients in centralized isolation. We suggest that making measures on the external factors can indirectly improve mental health of the patients and staff, which reflects the importance of promoting hospital management and related policies.
Measures and recommendations
Some measures have been taken in the above aspects. The National Health Commission of China (China NHCOTPSRO) proposed that the confirmed COVID-19 patients and the frontline workers should be the major populations of psychological intervention. The Wuhan Municipal Government established psychological teams of professional psychologists and psychiatrists in the designated hospitals and FSHs, as well as online and telephone psychological service platforms (Liu et al., Reference Liu, Yang, Zhang, Xiang, Liu, Hu and Zhang2020). The WHO put forward measures (Reference OrganizationOrganization) to protect the physical and mental health of medical workers. Some psychological intervention measures (China NHCOTPSRO; Wang et al., Reference Wang, Tang, Yang, Ma, Bai, Cai, Ma, Zhao, Wang and Liu2020b) had been adopted in the FSHs.
On the basis, and from the findings of this study as well, we make some specific recommendations to the psychological and psychiatric workers, hospital management, policy making, and social institutions. For temporary hospitals or isolation places in the pandemics, our recommendations would be helpful to promote mental health of the patients and staff.
For psychological and psychiatric workers, different levels of psychological support, intervention, and drug therapies should be provided to the patients and also the frontline workers according to their different psychological conditions. In the FSHs, various ways of support would be helpful, including education exhibition boards. group activities of rehabilitation, face-to-face consultation, online psychological service, psychological TV programs, etc. In order to prevent posttraumatic stress, long-term psychological follow-up, treatment, and rehabilitation should also be provided to the patients and staff in need.
For hospital management, hospital facilities and services should be improved, including life service centers that collect all perspectives on the hospital life and provide life service and care, information service centers that inform the patients of their conditions, discharge, and transfer arrangements, and provide inquiry service of laboratory and imaging reports, as well as communication facilities that maintain the communication of the individuals in the hospital with their families, friends, and the society outside. Management should also be improved, including a uniform, fair and efficient system of patient management that could relieve the burden of work on the staff, as well as a complete union system that provides prevention and protection to the staff, and ensure their appropriate working hours with breaks.
In policy making, the establishment and operation of FSHs or similar temporary facilities should be support. Current and follow-up medical expenses support should be provided for the patients, and extra support for those with difficulties. Polices should be made to regulate and supervise the hospitals, social institutions and communities to protect the rights of all patients and staff. And for social institutions, employers, and communities should help the patients returning to their normal work and community life, while mass media and social institutions should enhance publicity to eliminate the stigmatization of the patients and frontline workers.
Limitations
The limitations of our work include that all the interviews were conducted by one interviewer. Our sample was also small. Future qualitative studies can be conducted in other countries and centralized isolation places to complement our findings. In addition, due to the qualitative method we use, this study cannot reflect the changes in mental health of the patients. Follow-up studies should be carried out in the future to find how the experiences in FSHs affect their long-term mental health. However, this study involves perspectives from the mild COVID-19 patients in centralized isolation and staff of different occupations. Our findings and recommendations are helpful to improve the management of makeshift hospitals or similar facilities so as to promote mental health of the patients and staff.
Conclusions
In conclusion, the study has found mental health needs of the COVID-19 patients and staff in the FSHs. We have also made recommendations to psychological workers, hospital management, policy making, and social institutions, as the basis for promoting mental health of the patients and staff in makeshift hospitals during the pandemic.
Acknowledgements
We thank all the experts who have guided our semi-structured interview outlines. We thank the headquarters of EastWeat Lake Fangcang Shelter Hospital, Wuhan for their permission and support to our interviews. We also thank all the participants for sharing their perspectives. Sincere thanks to everyone who has ever supported this study.
Financial support
This work was supported by the Shanghai Key Laboratory of Psychotic Disorders (13DZ2260500) and Shanghai Mental Health Center Clinical Research Center (CRC2018YB02).
Conflict of interest
The authors declare no conflict of interest.
Ethical standards
Ethical approval for this research was received from Shanghai Mental Health Center.









