Introduction
Substantial epidemiological research has sought to identify and quantify the extensive functional, social and economic consequences of psychiatric disorders. Global Burden of Disease research showed that in 2010 mental and substance use disorders accounted for 7.4% (6.2–8.6%) of all disability-adjusted life-years worldwide (Whiteford et al., Reference Whiteford, Degenhardt, Rehm, Baxter, Ferrari, Erskine, Charlson, Norman, Flaxman and Johns2013). Although studies quantifying the overall burden of mental disorders using macro-level indicators are critical, nuanced research is needed in tandem to demonstrate the social and relational consequences of mental health problems – particularly the most common mental health problems, depression and anxiety.
Studies have demonstrated the wide range of consequences when depression and anxiety begin early in life. This research shows that depression and anxiety experienced during adolescence or early adulthood can disrupt the achievement of normative milestones – including high school completion (Butterworth and Leach, Reference Butterworth and Leach2017 – psychological distress; Kessler et al., Reference Kessler, Foster, Saunders and Stang1995 – anxiety and depressive mood disorder) and gaining employment (Fergusson and Woodward, Reference Fergusson and Woodward2002 – major depression). Studies have also investigated the impact of early onset mental health disorders on the timing and stability of partner relationships (i.e. married or cohabiting) and childbearing (Forthofer et al., Reference Forthofer, Kessler, Story and Gotlib1996; Kessler et al., Reference Kessler, Berglund, Foster, Saunders, Stang and Walters1997, Reference Kessler, Walters and Forthofer1998). Retrospective (cross-sectional) data from the National Comorbidity Survey in the USA has shown that anxiety, depressive, conduct and substance use disorders are associated with early first marriage (Forthofer et al., Reference Forthofer, Kessler, Story and Gotlib1996), teenage parenthood (Kessler et al., Reference Kessler, Berglund, Foster, Saunders, Stang and Walters1997) and subsequent separation and divorce (Kessler et al., Reference Kessler, Walters and Forthofer1998). However, little prospective epidemiological research has specifically assessed the impacts of early adulthood depression and anxiety on the quality of future partner relationships. This is the primary focus of the current study.
Lower depression symptomology is associated with better relationship quality (Weissman, Reference Weissman1987; Dehle and Weiss, Reference Dehle and Weiss1998; Whisman, Reference Whisman1999; Kiecolt-Glaser and Wilson, Reference Kiecolt-Glaser and Wilson2017). Longitudinal research investigating the temporal association between depression and relationship quality has adopted both a causation perspective (i.e. relationship quality predicts poor mental health over time) and a selection perspective (i.e. poor mental health select individuals into poor quality relationships) (Kim and McKenry, Reference Kim and McKenry2002), and indicates that the links are bi-directional (Kiecolt-Glaser and Wilson, Reference Kiecolt-Glaser and Wilson2017). For example, Davila et al. (Reference Davila, Karney, Hall and Bradbury2003) showed a bidirectional relationship between marital satisfaction and depression symptoms over a 4-year period. Najman et al. (Reference Najman, Khatun, Mamun, Clavarino, Williams, Scott, O'Callaghan, Hayatbakhsh and Alati2014) followed 2971 women first interviewed during pregnancy over 21 years and observed a bidirectional association between poor marital quality and depression. Although depression has been the focus of this research, studies on anxiety similarly indicate that anxiety symptomology and/or disorder is associated with poorer relationship quality (see McLeod, Reference Mcleod1994; Whisman, Reference Whisman1999 and Leach et al., Reference Leach, Butterworth, Olesen and Mackinnon2013 for examples of large population based studies; see Dehle and Weiss, Reference Dehle and Weiss2002 and Zaider et al., Reference Zaider, Heimberg and Iida2010 for smaller couple-focused and qualitative studies).
Although there is substantial research investigating depression and anxiety and poor relationship quality over time, the extent to which experiences specifically in early adulthood (prior to engagement in married or cohabiting relationships) go on to influence future partner relationship quality remains relatively unexplored. Early adulthood is a critical and complex time of life. The transition to adulthood appears to be extending beyond adolescence – as young people struggle to negotiate education, carer and family formation goals (Settersten et al., Reference Settersten, Furstenberg and Rumbaut2008). Depression and anxiety at this time likely has adverse consequences for future relationships. In one of the only prospective studies available (n = 1700), diagnostic depression in adolescence predicted lower relationship quality in early adulthood for both women and men (Gotlib et al., Reference Gotlib, Lewinsohn and Seeley1998). However, this study is limited by a short follow-up period (only until mid-20s), and the impacts of anxiety were not considered.
The current used four time-points of data (spanning 12 years) from an Australian population-based cohort study to investigate the consequences of depression and generalised anxiety during early adulthood (prior to first marriage or cohabiting relationship) for both: (a) future relationship status and (b) future relationship quality. We control for a range of potential confounders associated with depression and/or anxiety including gender (McLean et al., Reference McLean, Asnaani, Litz and Hofmann2011; Salk et al., Reference Salk, Hyde and Abramson2017), age (Jorm, Reference Jorm2000), education (Butterworth and Leach, Reference Butterworth and Leach2017), employment (Paul and Moser, Reference Paul and Moser2009), financial hardship (Kiely et al., Reference Kiely, Leach, Olesen and Butterworth2015), alcohol use (Rodgers et al., Reference Rodgers, Korten, Jorm, Jacomb, Christensen and Henderson2000), smoking (Lasser et al., Reference Lasser, Boyd, Woolhandler, Himmelstein, McCormick and Bor2000) and physical functioning (Ohrnberger et al., Reference Ohrnberger, Fichera and Sutton2017). The main analyses explore the impact of baseline anxiety and depression on future relationship quality using all time-points where data are available. Supplementary analyses are also conducted to confirm the impacts on relationship quality in the ‘first’ relationship entered to omit the effects of multiple relationships.
Methods
Participants and procedure
Data were from four time-points of the Personality and Total Health (PATH) Through Life project, a large community-based cohort study based at The Australian National University that measures physical health, mental health, cognitive and personality characteristics across the lifespan. Initially, potential participants were selected at random from the electoral rolls of Canberra ACT and Queanbeyan NSW Australia, within three age cohorts: 20–24 years, 40–44 years and 60–64 years. Follow-up data have been collected at approximately four yearly intervals and to date, four waves of data have been collected (see Anstey et al., Reference Anstey, Christensen, Butterworth, Easteal, Mackinnon, Jacomb, Maxwell, Rodgers, Windsor and Cherbuin2011).
The current paper focuses on the youngest 20s cohort. In this cohort, 2404 respondents (48.3% male) completed the baseline assessment (February 1999–April 2000) representing 58.6% of the invited population. For the baseline and follow-up data collection at wave 2 (m = 4.10 years later in April 2003–June 2004) and wave 3 (m = 3.97 years later in April 2007–April 2008), respondents were interviewed by a trained interviewer. Participants completed self-report measures and the interviewer additionally administered face-to-face physical and cognitive tests. For wave 4 follow-up (m = 4.06 years later in May 2011–May 2012), all participants were invited to complete the self-report measures online, and a randomly selected subsample of 580 participated in a face-to-face interview with additional physical and cognitive tests. All data used in the current study were from the self-reported measures at each wave.
The sample was initially restricted to 1592 participants (54.6% male) who at baseline (aged 20–24) had never married, did not live with a partner and did not have children. The first set of analyses examined the effect of baseline generalised anxiety and depression levels on future relationship status – comparing those who never reported entering a relationship (n = 449) with those who entered a relationship at follow-up (n = 1143). The 1030 participants who reported being in a relationship at one of the follow-up periods were included in a second set of analyses focused on relationship quality (wave 2: n = 612, wave 3: n = 809, wave 4: n = 576; 1997 observations). Table 1 shows the number of participants who reported their first relationship at each wave, continued to report not being in a relationship, reported multiple relationships and dropped-out of the study. There was little item-missing data (<1% on any variable). Therefore, no data imputation was conducted.
Table 1. Partner relationship status over the three follow-up waves (time-points of data collection)
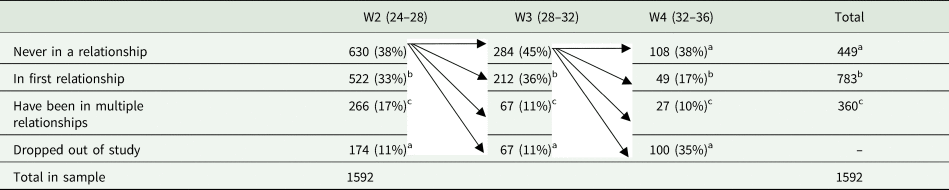
Note: At W1, everyone in the sample was not in a partner relationship and had never been married.
a 449 recorded as ‘never in a relationship’ at the last time they were interviewed (i.e. they may have subsequently dropped out of the study).
b 783 recorded as in their first relationship at one of the three follow-up time-points.
c 360 recorded as having been in multiple relationships at the time of interview.
Measures
Depression and anxiety were measured at all waves using the Goldberg Depression and Anxiety Scales (Goldberg et al., Reference Goldberg, Bridges, Duncan-Jones and Grayson1988). Each scale contains nine symptom-related items (yes = 1; no = 0) summed to yield scale scores ranging from 0 to 9. The scales have been found to effectively detect elevated levels of depression and generalised anxiety in community samples (Mackinnon et al., Reference Mackinnon, Christensen, Jorm, Henderson, Scott and Korten1994; Kiely and Butterworth, Reference Kiely and Butterworth2015). Although the correlation between the two Goldberg Scales is high (r = 0.71, p < 0.001 in this sample), a two factor model with separate depression and anxiety dimensions is supported (Christensen et al., Reference Christensen, Jorm, Mackinnon, Korten, Jacomb, Henderson and Rodgers1999). Both scales have good internal reliability in the PATH sample (depression: α = 0.81; anxiety α = 0.78). Both scales were rescaled to aid in interpretation of the regression coefficients – such that a one-point increase on the scales represents the difference between the 25th and the 75th percentiles on the distribution (i.e. a score of ‘0’ represents (low) scores on the 25th percentile and a score of ‘1’ represents (high) scores on the 75th percentile). Binary scores representing likely depression and generalised anxiety disorder diagnosis were also calculated based on validated cut-points assessed against the CIDI (i.e. a score of ⩾5 on the depression scale and ⩾7 on the anxiety scale (Kiely and Butterworth, Reference Kiely and Butterworth2015)) to describe the proportion of the sample with likely depression and/or generalised anxiety disorder, and in supplementary analyses exploring the impact of comorbidity.
Relationship status was assessed at each wave using an item that asked: are you currently in a relationship with someone? Responses were: 1 – ‘Yes, living with the person you are married to’, 2 – ‘Yes, living with a partner (but not married to them)’, 3 – ‘Yes, in a relationship with someone but not living with them’ and 4 – ‘No, not in a relationship with anyone’. This item was recoded to represent a binary indicator of relationship status where 1 represented ‘in a marriage/cohabiting relationship’ (i.e. responses 1 or 2) and 0 represented ‘not in a marriage/cohabiting relationship’ (i.e. responses 3 or 4). An item also asked at each wave ‘How many times have you been married or lived with a partner?’ A measure of partner relationship status over the follow-up period was created where 1 represented ‘observed in first marriage/cohabiting relationship’, 0 represented ‘never observed in a marriage/cohabiting relationship’, and 2 represented ‘observed in multiple marriages/cohabiting relationships’.
Social support and conflict within the partner relationship were assessed using items developed and validated by Schuster et al. (Reference Schuster, Kessler and Aseltine1990). Perceived positive support was assessed using five items, including ‘How often does your partner understand the way you feel about things?’ Negative interactions or conflict were assessed using five items, including ‘How often do you have an unpleasant disagreement with your partner?’ Possible responses for both sets of items were: 0 – ‘Never’, 1 – ‘Rarely’, 2 – ‘Sometimes’ and 3 – ‘Often’. The conflict items did not ask about physical conflict, but instead focused on disagreement and tension. Total scale scores ranged from 0 to 15. Scale scores were standardised to provide z-scores to assist with interpretation. Preliminary factor analyses confirmed the existence of two separate factors representing support and conflict. Measures of relationship support and conflict experienced in the first marriage or de facto relationship observed were also constructed (i.e. data were recorded only once for participants in the first relationship entered and was then censored).
Covariates
Socio-economic covariates included gender, age, years of education and employment status. A measure of financial hardship was generated based on one item: ‘Have you or your family had to go without things you really needed in the last year because you were short of money?’ Respondents were classified as having financial hardship (1) if they responded ‘yes, often’ or ‘yes, sometimes’ to this item (v. ‘no’). A binary measure of current smoking was included, as was the alcohol use disorders identifications test (AUDIT) (Saunders et al., Reference Saunders, Aasland, Babor, De la Fuente and Grant1993). Participants were classified into one of three alcohol use categories based on the National Health and Medical Research Council (2001) guidelines: (a) non-drinkers or occasional drinkers (⩽monthly), (b) moderate drinkers (<28 standard drinks per week for men and <14 for women) or (c) hazardous or harmful drinkers (⩾28 drinks per week for men and ⩾14 for women) (NHMRC, 2001). Given the comorbidity between mental and physical health problems, the short-from physical health summary (SF-12) was also included as measure of physical functioning (Ware et al., Reference Ware, Kosinski and Keller1996). A variable representing whether each participant dropped out of the study was also constructed (0, 1).
Statistical analyses
Descriptive statistics for the baseline analysis sample were initially calculated. A series of logistic regression models were used to examine the association between baseline levels of depression and anxiety (at age 20–24) and odds of subsequently entering (or not entering) a partner relationship during the study period (12 years). These models adjusted for attrition (i.e. ‘dropped-out’ v. ‘never dropped-out’ of the study), given attrition was significantly associated with never being in a relationship (χ 2 = 177.53, p < 0.001).
Analyses used the full panel of data (four waves) in random effects models to examine the effect of baseline mental health on future relationship support and conflict at the follow-ups. The analyses adjusted for all covariates across the three-time points (i.e. time varying), including the wave at which data were recorded. In a final model, the analyses included a variable representing current (or follow-up) depression and anxiety symptom levels to further ascertain the independent contribution of baseline mental health. Potential gender differences were evaluated by the inclusion of an interaction term, however as this term was not significantly associated with either relationship status at follow-up, or levels of relationship support or conflict, all models included both men and women. Although the social support and conflict measures (outcomes) were skewed (with respondents more likely to report high levels of social support and low levels of conflict), no transformations were undertaken in the main analyses as the large sample size was sufficiently robust to violations of normality (Lumley et al., Reference Lumley, Diehr, Emerson and Chen2002). For all tests significance was set at p < 0.05. Data were analysed using STATA SE version 15.
A series of supplementary analyses were used to aid in the interpretation of the findings and to test their robustness. First, analyses examined the impact of baseline depression and anxiety on levels of partner support and conflict experienced in the first marriage or cohabiting relationship recorded at follow-up to omit the potential influence of multiple relationships (i.e. outcome data were recorded in the first relationship entered and was then censored). These models adjusted for the time-point at which the first relationship was entered. Second, the relationship quality outcomes were transformed to explore improving the skewed distribution. Final analyses assessed the impact of comorbidity (experiencing depression or anxiety concurrently) in association with subsequent relationship quality.
Results
Descriptive analyses – characteristics of the sample
The average depression score at baseline for the full sample was 2.6 for males and 3.0 for females, and the average anxiety score was 3.2 for males and 4.3 for females. Using the validated cut-points for the Goldberg scales at baseline (age 20–24), 22% of men and 26% of women were categorised as having clinically significant depression, 15% of men and 23% of women were categorised as having clinically significant generalised anxiety. Considering comorbidity, 10% of men and 14% of women scored highly for both depression and generalised anxiety.
Table 2 shows the sample baseline characteristics and mean differences for baseline depression and anxiety levels. Greater depression was significantly associated with being female, fewer years of education, being unemployed (compared to working full-time), financial hardship, harmful alcohol use, smoking, lower physical functioning and never entering a partner relationship over the study period. Greater anxiety was significantly associated with being female, fewer years of education, working part-time or not being in the labour force (compared to working full-time), financial hardship, smoking and lower physical functioning. Both baseline depression and anxiety were significantly associated with lower relationship support and greater relationship conflict recorded at follow-up.
Table 2. Descriptive statistics, including mean differences and correlations with levels of depression and anxiety at baseline (aged 20–24) (n = 1592)
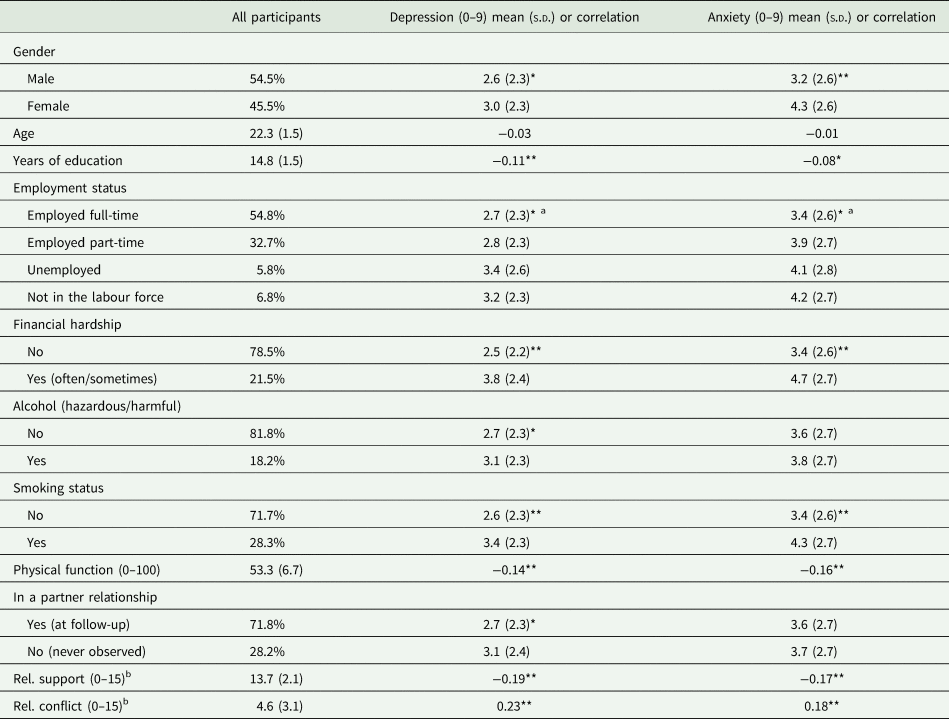
Note: *p < 0.05. **p < 0.001 notes that this variable is significantly associated with baseline depression or anxiety.
a Post-hoc comparisons (Sidak test) for each level within the ANOVA showed that those who were unemployed had significantly higher depression that those who were employed full-time, and that those who were employed part-time or not in the labour force had significantly higher anxiety than those employed full-time.
b Reported only for participants who reported being in a cohabiting relationship in at least one of the follow-up study waves and reported relationship quality data (n = 1030). All covariates taken at baseline, except relationship status and relationship support which use follow-up data.
Relationship status – findings for baseline depression and anxiety
Results of the logistic regression analyses examining baseline depression and anxiety levels in association with entry (v. never entry) into a partner relationship are shown in Table 3. The initial model (1) shows that baseline depression was significantly associated with lower odds of entering a relationship (odds ratio (OR): 0.78, confidence interval (CI): 0.63–0.93). This association remained significant after adjusting for baseline socio-demographic factors, physical functioning and substance use (model 2) (OR: 0.79, CI: 0.64–0.98). All models for baseline anxiety show that levels were not significantly associated with odds of entering a relationship.
Table 3. Baseline depression and anxiety predicting odds of ever being (v. never being) in a partner relationship (n = 1592)
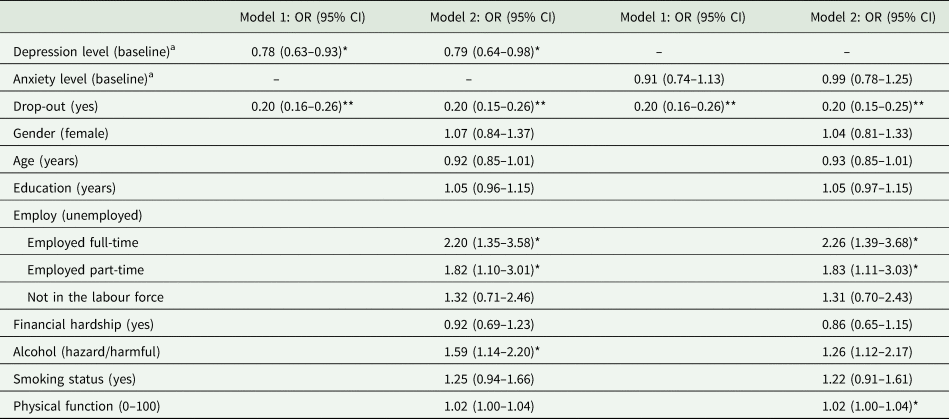
Note: Logistic regression. *p < 0.05. **p < 0.001.
a The scale scores for depression and anxiety have been rescaled such that a one-point increase on the scales represents the difference between the 25th and the 75th percentiles on the distribution.
Relationship quality (support and conflict) – findings for baseline depression
Results of the linear mixed model examining baseline depression levels in association with follow-up partner support and conflict are shown in Table 4. The first series of models predicted relationship support. The initial models (1 and 2) showed that baseline depression was significantly associated with lower partner support at follow-up – this was the case after adjusting for time-varying covariates. This effect continued to be significant once current levels of depression (at follow-up) were accounted for (model 3, B: −0.16, CI: −0.25 to −0.06). The second series of models in Table 4 predicted the level of conflict in partner relationships. The initial models (1 and 2) showed that higher baseline depression was significantly associated with higher relationship conflict at follow-up after adjusting for covariates. Models 3 showed that baseline depression continued to predict relationship conflict after adjusting for current levels of depression (model 3, B: 0.30, CI: 0.21–0.40).
Table 4. Baseline depression predicting relationship quality and conflict at all (3) follow-up waves
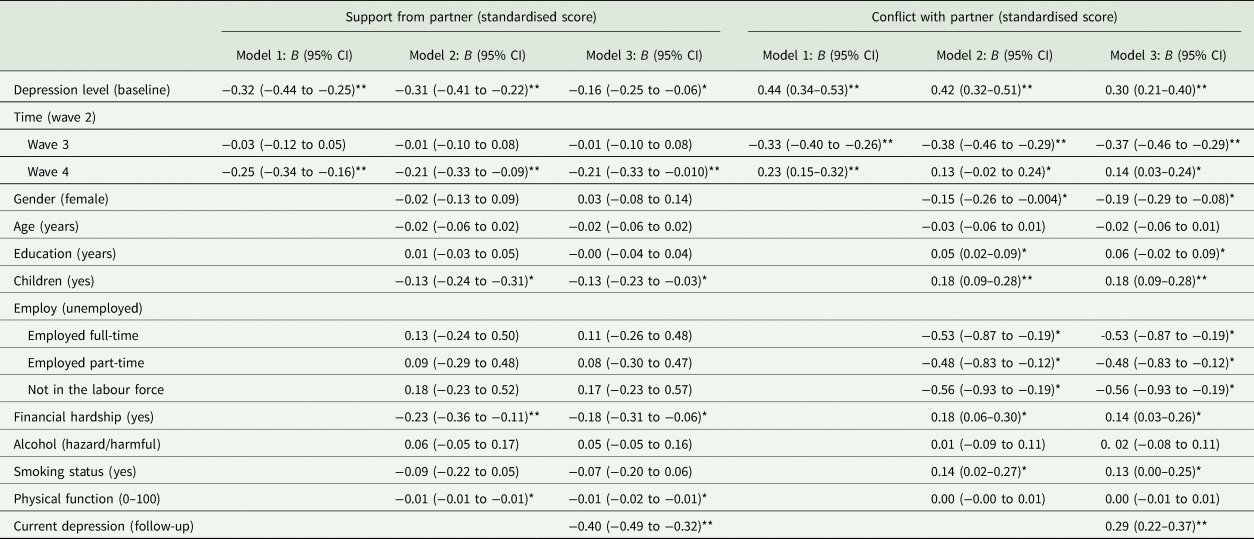
Note: Linear regression. *p < 0.05. **p < 0.001. All covariates are time-varying. The scale scores for baseline and follow-up depression have been rescaled such that a one-point increase on the scales represents the difference between the 25th and the 75th percentiles on the distribution.
No. of observations: Model 1: 1997, Model 2: 1921, Model 3: 1920.
Relationship quality (support and conflict) – findings for baseline anxiety
Results of the linear mixed model examining baseline anxiety levels in association with levels of subsequent partner support and conflict are shown in Table 5. The initial models (1 and 2) showed that baseline anxiety was significantly associated with lower partner support after adjusting for covariates. The final model showed that higher levels of baseline anxiety continued to be associated with lower partner support (B: −0.15, CI: −0.26 to −0.05), after adjusting for follow-up anxiety. The second series of models in Table 5 predicted relationship conflict. The initial models (1 and 2) showed that higher baseline anxiety was significantly associated with higher relationship conflict after covariate adjustment. The final model showed that higher baseline anxiety continued to be associated with higher subsequent conflict after adjusting for follow-up anxiety (B: 0.19, CI: 0.09–0.30).
Table 5. Baseline anxiety predicting relationship quality and conflict at all (3) follow-up waves
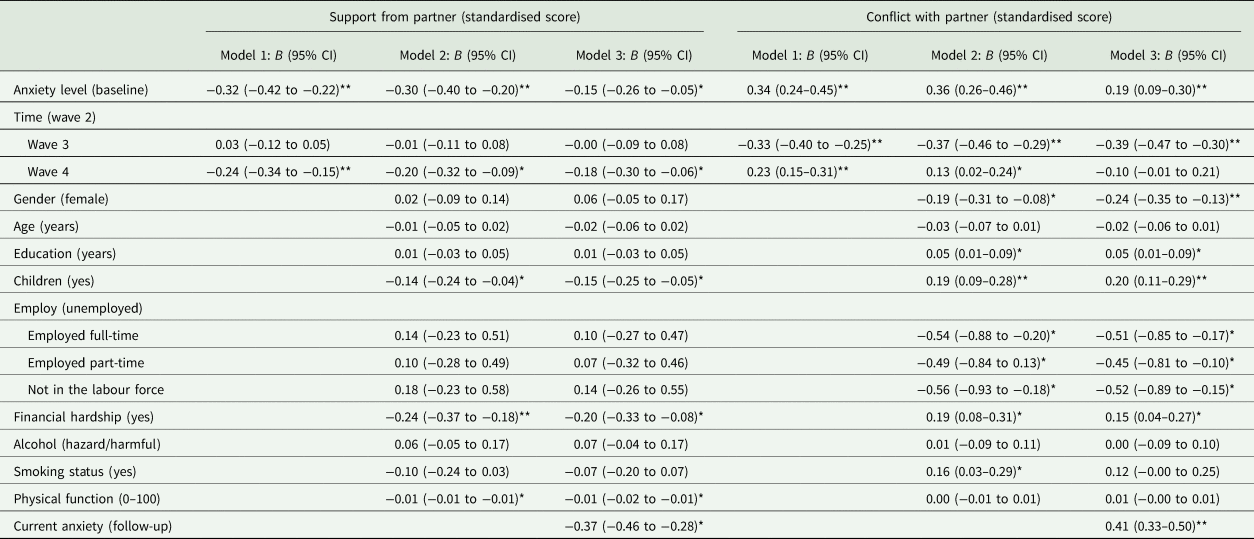
Note: Linear regression. *p < 0.05. **p < 0.001. All covariates are time-varying. The scale scores for baseline and follow-up anxiety have been rescaled such that a one-point increase on the scales represents the difference between the 25th and the 75th percentiles on the distribution.
No. of observations: Model 1: 1997, Model 2: 1921, Model 3: 1920.
Supplementary analyses
Supplementary analyses were conducted as outlined in the ‘Statistical analyses’ section. All additional analyses essentially mirrored those found in the main analyses. See online Supplementary section and tables for further details.
Discussion
The current prospective study found that higher depression in early adulthood was associated with a greater likelihood of remaining unpartnered in the future. In addition, for those who did find a partner, depression and anxiety in early adulthood predicted lower relationship support and more conflict. These associations remained significant after adjusting for a range of time-varying socio-economic factors, health behaviours and depression/anxiety levels at follow-up. The enduring association after adjusting for follow-up mental health suggests that past experiences of depression and anxiety matter above and beyond the impact of concurrent mental health problems (which are already known to substantially impact on relationship quality), supporting a greater focus on prevention and early intervention (Jorm, Reference Jorm2014). These findings add to the body of research demonstrating that depression and anxiety in early adulthood have important personal and social costs, not only for the individuals experiencing poor mental health, but also their partners.
Existing epidemiological research exploring early onset depression and anxiety in relation to partner relationships has focused on the consequences for early marriage and teenage parenting (Forthofer et al., Reference Forthofer, Kessler, Story and Gotlib1996; Kessler et al., Reference Kessler, Berglund, Foster, Saunders, Stang and Walters1997; Gotlib et al., Reference Gotlib, Lewinsohn and Seeley1998), and also subsequent separation and divorce (Kessler et al., Reference Kessler, Walters and Forthofer1998). The current study adds new information, finding that greater levels of depression (but not anxiety) in early adulthood (aged 20–24) are associated with a lower likelihood of finding a long-term partner in the future. This finding is drawn from a sample that had no children or previous partner relationships at baseline (aged 20–24), and therefore (to some extent) confounding concerning premature/adolescent serious partner relationship formation is removed. Overall, the current findings align with research linking depression, social isolation and loneliness (Matthews et al., Reference Matthews, Danese, Wertz, Odgers, Ambler, Moffitt and Arseneault2016), as well as descriptive (i.e. cross-sectional) studies showing that those with poor mental health are less likely to be in partner relationships (Pearlin and Johnson, Reference Pearlin and Johnson1977; Stack and Eshleman, Reference Stack and Eshleman1998; Scott et al., Reference Scott, Wells, Angermeyer, Brugha, Bromet, Demyttenaere, de Girolamo, Gureje, Haro and Jin2010).
The findings regarding reduced relationship support and increased conflict point towards the pathways via which psychiatric symptoms and disorders may result in higher rates of separation and divorce (Kessler et al., Reference Kessler, Walters and Forthofer1998), offering potential avenues for further research and intervention. Previous research has shown that individuals with any mood disorder were 1.7 times more likely to subsequently separate/divorce and individuals with any anxiety disorder were 1.8 times more likely (Kessler et al., Reference Kessler, Walters and Forthofer1998). The current findings accord with hypotheses that decline in social support and rise in relationship conflict might explain this association. Most significantly, we find that early experiences of depression and anxiety – when young adults are not yet in a significant relationship – can influence the quality of relationships years later.
Strengths and limitations
The current study has significant strengths, including a large representative community-based sample, the range of socio-economic and health/lifestyle correlates adjusted over time (time-varying), the extensive prospective (rather than retrospective) follow-up period and the exploration of both depression and anxiety symptomology. However, several limitations must be acknowledged. Diagnostic measures were not available to capture diagnosis of a depressive or anxiety disorder at baseline, however, well-validated psychometric measures were used to assess levels of anxiety and depression. Although these scales have validated cut-points to determine a likely diagnosis of generalised anxiety and depressive disorder (Kiely and Butterworth, Reference Kiely and Butterworth2015), in the current analyses they were retained as continuous measures to maximise statistical power. Similarly, measures of relationship support and conflict were self-report and therefore represent participants' perceptions rather than an objective indicator. However, the exposure (baseline mental health) and the outcomes (relationship quality measures) were assessed at different points in time (up to 12 years apart), reducing the influence of ‘common method variable bias’. The current study did not investigate the mechanisms via which depression and/or anxiety experienced in early adulthood flow through to impact on relationship quality. These likely include ongoing psychological and interpersonal disruption in accordance with theories and evidence of stress generation (see Hammen, Reference Hammen2005, p. 303 for an overview). Including the idea that depressed or anxious individuals might select themselves into adverse environmental contexts and social relationships (Kendler et al., Reference Kendler, Karkowski and Prescott1999 in Hammen, Reference Hammen2005). Finally, although the prospective study design supports the hypothesis that experiences of depression and anxiety are linked to subsequent poor relationship quality, our findings are not sufficient to conclude this is a causal relationship and more studies are required. For example, it is possible that a negative predisposition or cognitive bias underlies the association between baseline depression and anxiety and follow-up negative perceptions of relationship quality – a plausible alternative explanation for the enduring effect after controlling for current symptomology.
The current study found that future relationship status and quality (i.e. levels of support and conflict) was associated with prior experiences of depression or anxiety in early adulthood. This finding, in conjunction with extant research demonstrating the adverse, far-reaching impacts of poor mental health, supports ongoing calls for a shift in focus from treatment to early intervention and prevention. Preventing mental health problems is critical, not only to reduce the need for (and costs associated with) treatment, but to prevent related social adversity across the lifespan. Engaged, supportive social relationships are an important indicator of quality of life (Helgeson, Reference Helgeson2003).
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796020000530.
Data
Data from the PATH project can be requested and research conducted in partnership with the PATH Research Committee (see https://rsph.anu.edu.au/research/projects/personality-total-health-path-through-life). The PATH study is jointly conducted by The Australian National University and The University of New South Wales.
Acknowledgements
The authors would like to thank past and present Chief Investigators and Administrators on the PATH Through Life Project and the PATH project participants. In particular, we thank the PATH Interviewers, Karen Maxwell and Trish Jacomb; and PATH Chief Investigators: Kaarin Anstey, Helen Christensen, Anthony Jorm, Bryan Rodgers, Andrew Mackinnon, Simon Easteal and Nicolas Cherbuin.
Financial support
The PATH Through Life Project has been supported by numerous grants provided by the Australian National Health and Medical Research Council (NHMRC) (973302, 179805 and 418039). In addition, this work was funded by a National Health and Medical Research Council (NHMRC) Early Career Fellowship (L.L., 1035803), and an Australian Research Council (ARC) Future Fellowship (P.B., FT13101444). The funding bodies played no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The PATH project was approved by the Human Research Ethics Committee of the Australian National University and all participants provided written informed consent.









