Introduction
Comorbidity within mental disorder is common – individuals with one type of mental disorder often develop other types of mental disorders across their lifespan (Pincus et al., Reference Pincus, Tew and First2004; Maj, Reference Maj2005; Kessler et al., Reference Kessler, Cox, Green, Ormel, McLaughlin, Merikangas, Petukhova, Pine, Russo, Swendsen, Wittchen and Zaslavsky2011, Reference Kessler, Avenevoli, McLaughlin, Green, Lakoma, Petukhova, Pine, Sampson, Zaslavsky and Merikangas2012). Understanding patterns of comorbidity within mental disorders is essential if we wish to understand the influence of mental disorders on premature mortality (Plana-Ripoll et al., Reference Plana-Ripoll, Pedersen, Agerbo, Holtz, Erlangsen, Canudas-Romo, Andersen, Charlson, Christensen, Erskine, Ferrari, Iburg, Momen, Mortensen, Nordentoft, Santomauro, Scott, Whiteford, Weye, McGrath and Laursen2019a) and the contribution of mental disorders to the global burden of disease (Weye et al., Reference Weye, Christensen, Momen, Iburg, Plana-Ripoll and McGrath2020). Recently, we published a comprehensive study of pair-wise comorbidity within mental disorders based on Danish health registers (Plana-Ripoll et al., Reference Plana-Ripoll, Pedersen, Holtz, Benros, Dalsgaard, de Jonge, Fan, Degenhardt, Ganna, Greve, Gunn, Iburg, Kessing, Lee, Lim, Mors, Nordentoft, Prior, Roest, Saha, Schork, Scott, Scott, Stedman, Sorensen, Werge, Whiteford, Laursen, Agerbo, Kessler, Mortensen and McGrath2019b). That study found that receiving a diagnosis of a wide range of mental disorders were associated with significantly elevated risks of a subsequent diagnosis of a wide range of other types of mental disorder. In other words, lifetime comorbidity among mental disorders was pervasive. That study also presented age- and sex-specific hazard ratios (HRs) and cumulative incidence proportions (CIPs) for all disorder pairs studied. However, the study had several important limitations, including that it only examined broad ICD-10 F subchapter headings (e.g. mood disorders) rather than specific types of disorders (e.g. Major Depressive Episode, Bipolar Affective Disorder etc.) and was based on registers limited to cases diagnoses in hospital and outpatient settings (i.e. those who received treatment only from their general practitioners were not included). In addition, as Denmark is a wealthy country, estimates may not be generalisable to a wider range of sites.
We had the opportunity to address these gaps by examining data from the WHO World Mental Health (WMH) Surveys (Kessler et al., Reference Kessler, Aguilar-Gaxiola, Alonso, Chatterji, Lee and Ustun2009), a series of community epidemiological surveys that assessed lifetime prevalence of a wide range of both untreated and treated mental disorders in a representative household sample across a range of nations. The study aimed to examine pair-wise temporally-ordered lifetime comorbidity between all logically possible pairs of DSM-IV disorders (24 types) assessed in the WMH surveys and to generate age- and sex-specific HRs and CIPs for each of these pairs. Our study is observational, and thus we do not make any claim that prior mental disorders cause later mental disorders. Our guiding hypothesis is that comorbidity within mental disorders is pervasive. The data are available in an interactive data visualisation webpage (https://holtzy.github.io/Como-in-World-Heath-Survey/index.html).
Methods
Samples and procedures
Data came from 29 coordinated WMH Surveys conducted in 27 countries. Spain and Colombia have separate national and regional surveys. A total of 19 of these surveys were nationally representative, and several focused on selected urban or metropolitan areas within the country. These surveys included six lower-middle-income countries, seven upper-middle-income countries, and 16 high-income countries, according to the World Bank classification at the time the survey was conducted. In most countries, internal subsampling was used to reduce respondent burden and average interview time by dividing the interview into two parts (see Supplement for additional details).
Measures
All surveys used the WHO Composite International Diagnostic Interview (CIDI 3⋅0) (Kessler et al., Reference Kessler, Chiu, Demler, Merikangas and Walters2005), a validated, fully structured lay administered interview. Mental disorders were diagnosed using DSM-IV criteria. A total of 24 mental disorders were assessed, including lifetime mood disorders (Major Depressive Episode [MDE], Bipolar Disorder, Dysthymia), lifetime anxiety disorders (Panic Disorder, Generalised Anxiety Disorder [GAD], Social Phobia, Specific Phobia, Agoraphobia without Panic Disorder, Post-Traumatic Stress Disorder [PTSD], Obsessive-Compulsive Disorder [OCD], Child and Adult Separation Anxiety Disorder), lifetime impulse-control disorder (Intermittent Explosive Disorder, Conduct Disorder, Attention Deficit Hyperactivity Disorder, Oppositional Defiant Disorder, Anorexia Nervosa, Bulimia Nervosa, Binge Eating Disorder), lifetime substance-use disorder (Alcohol abuse and dependence, Drug abuse and dependence, Nicotine Dependence). CIDI organic exclusion rules were applied when making a diagnosis but hierarchy rules were not applied in this study.
The CIDI was developed as an interview to be conducted by trained laypersons. The questions and answers are standardised to a high level in order to reduce the interpretation by interviewers to a maximum extent. In the WMH surveys, all survey interviewers went through a two-week certification training course for CIDI 3.0 instrument prior to starting fieldwork. All interviewers have received the same training and adhere to the same protocol regarding contacts and interview administration. The trainers of the interviewers also attended a one-week training course carried out by WHO-certified trainers. Blinded clinical reappraisal interviews using SCID with CIDI found good concordance between diagnoses (Haro et al., Reference Haro, Arbabzadeh-Bouchez, Brugha, de Girolamo, Guyer, Jin, Lepine, Mazzi, Reneses, Vilagut, Sampson and Kessler2006).
Statistical analysis
We estimated the associations between all logically possible pair-wise DSM-IV disorders accounting for the temporality of these disorders. As the surveys were cross-sectional, temporality was established using retrospectively reported of age-of-onset for each disorder. We estimated the risk of reporting later disorder in those who were exposed to a disorder of interest (henceforth referred to as ‘prior disorder’). All prior disorders were treated as time-varying exposures when assessing the risk of a later disorder. Cox proportional hazards models with the age of onset of the prior disorder as a time-dependent covariate were used to calculate the HR of the first onset of later disorder associated with the prior disorder. We examined models that (i) adjusted for country, age-cohort (i.e. age-at-interview) and sex (‘Model A’), and (ii) adjusted for country, age-cohort, sex, type and number of mental disorders with onset preceding the prior disorder (‘Model B’). For overall HRs and the CIPs, we repeated the analysis to obtain sex-specific estimates. We further investigated if the associations between prior and later disorders differed by time since the onset of the prior disorder by estimating time-dependent HRs. For this analysis, we repeated models A and B using six dummy variables representing time since the exposure of prior disorder: 0–1, 1–2, 2–5, 5–10, 10–15, 15 years or more (in order to be comparable to the analysis by Plana-Ripoll et al. (Reference Plana-Ripoll, Pedersen, Holtz, Benros, Dalsgaard, de Jonge, Fan, Degenhardt, Ganna, Greve, Gunn, Iburg, Kessing, Lee, Lim, Mors, Nordentoft, Prior, Roest, Saha, Schork, Scott, Scott, Stedman, Sorensen, Werge, Whiteford, Laursen, Agerbo, Kessler, Mortensen and McGrath2019b)). All parameter estimates (beta) were exponentiated to obtain HRs. The cumulative incidence or cumulative failure probability curves were generated using the product limit approach (Kaplan and Meier, Reference Kaplan and Meier1958) by restricting the analysis to the subset of those with a prior disorder. These were stratified by sex and age of onset of the prior disorder (<20, 20–40, >40 years; consistent with the analysis by Plana-Ripoll et al. (Reference Plana-Ripoll, Pedersen, Holtz, Benros, Dalsgaard, de Jonge, Fan, Degenhardt, Ganna, Greve, Gunn, Iburg, Kessing, Lee, Lim, Mors, Nordentoft, Prior, Roest, Saha, Schork, Scott, Scott, Stedman, Sorensen, Werge, Whiteford, Laursen, Agerbo, Kessler, Mortensen and McGrath2019b)). Respondents were followed until they developed later disorder or until the time at an interview (censored). This allowed us to estimate the absolute risk of later disorder after developing the prior disorder. All analyses were performed using SAS 9.4. The Supplementary Material, and all the data management and analysis codes can be found on https://github.com/clim072/NB-COMO. An interactive webpage was also created to display all the results from this study https://holtzy.github.io/Como-in-World-Heath-Survey/index.html.
Results
Pair-wise associations between mental disorders
The characteristics of the sample are presented in Table 1. The estimates for the pair-wise comorbidity between mental disorders are presented in online Supplementary Fig. 1. A selection of the four panels is shown in Fig. 1. In the basic model adjusting for age-cohort, sex and country (model A; purple circles in the plots), all prior disorders were associated with an elevated risk of the onset of later disorders (a vertical line at HR = 1 representing ‘null effect’ is also plotted in each panel). For model B (orange triangles in the plots), the effect sizes attenuated substantially and the confidence intervals (CIs) included one for some disorder pairs (e.g. when alcohol or drug dependence was the prior disorder). However, in general, the overall pattern of the findings remained comparable between the two models. The sex-specific associations with adjustment for comorbidity (model B) are shown in online Supplementary Fig. 2. The median HR was 12.1 (mean = 14.4; range 5.2–110.8, interquartile range = 6.0–19.4). Some of the highest HRs were found between closely-related types of mental disorders. For example, prior MDE and later dysthymia (HR = 45.9, 95% CI = 40.5–51.9) and prior Bulimia Nervosa and later Binge Eating Disorder (HR = 62.3, 95% CI = 48.5–80.2).
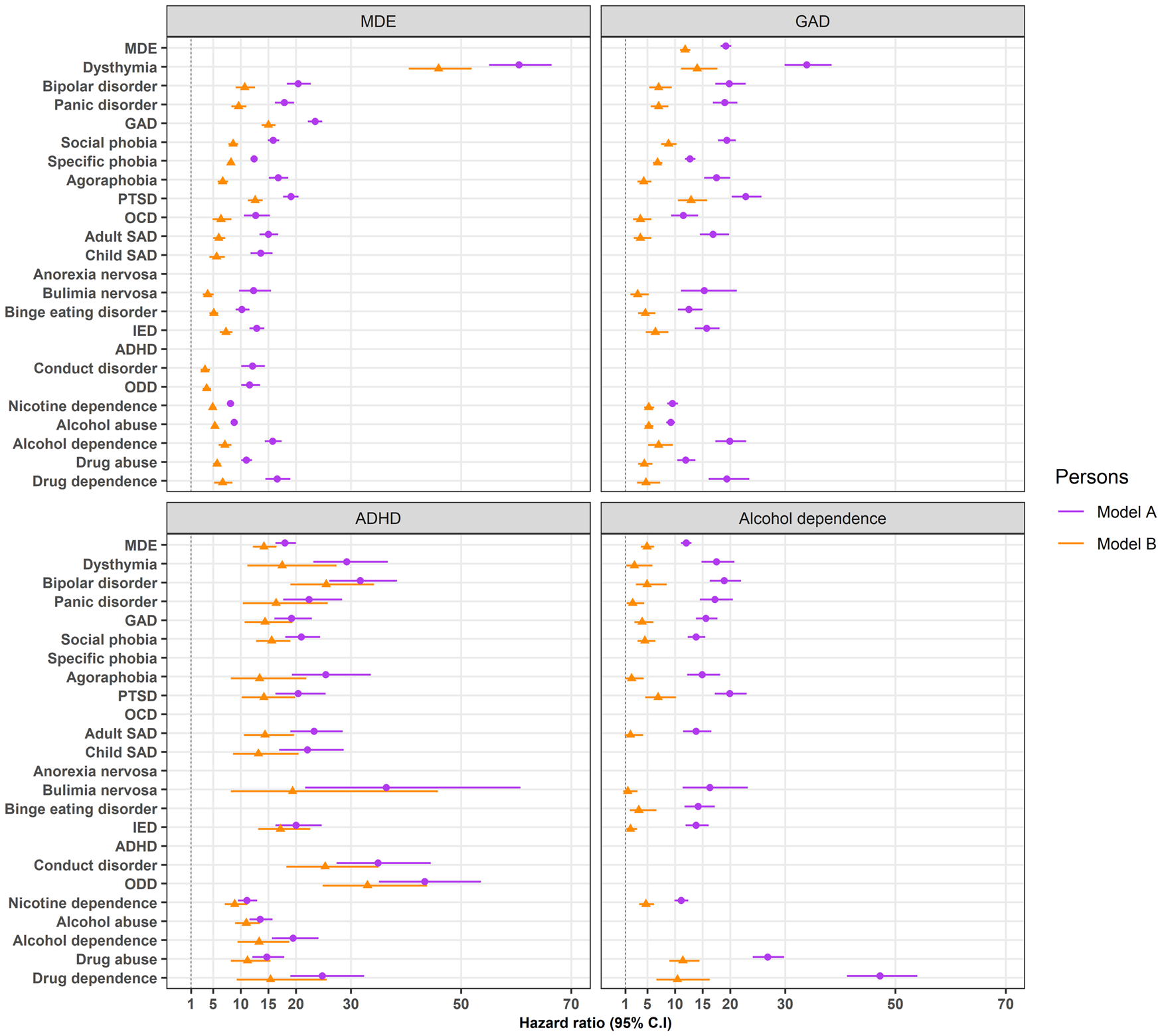
Fig. 1. Visualisation of several of the pair-wise associations between mental disorders
Table 1. WMH sample characteristics by World Bank income categoriesa
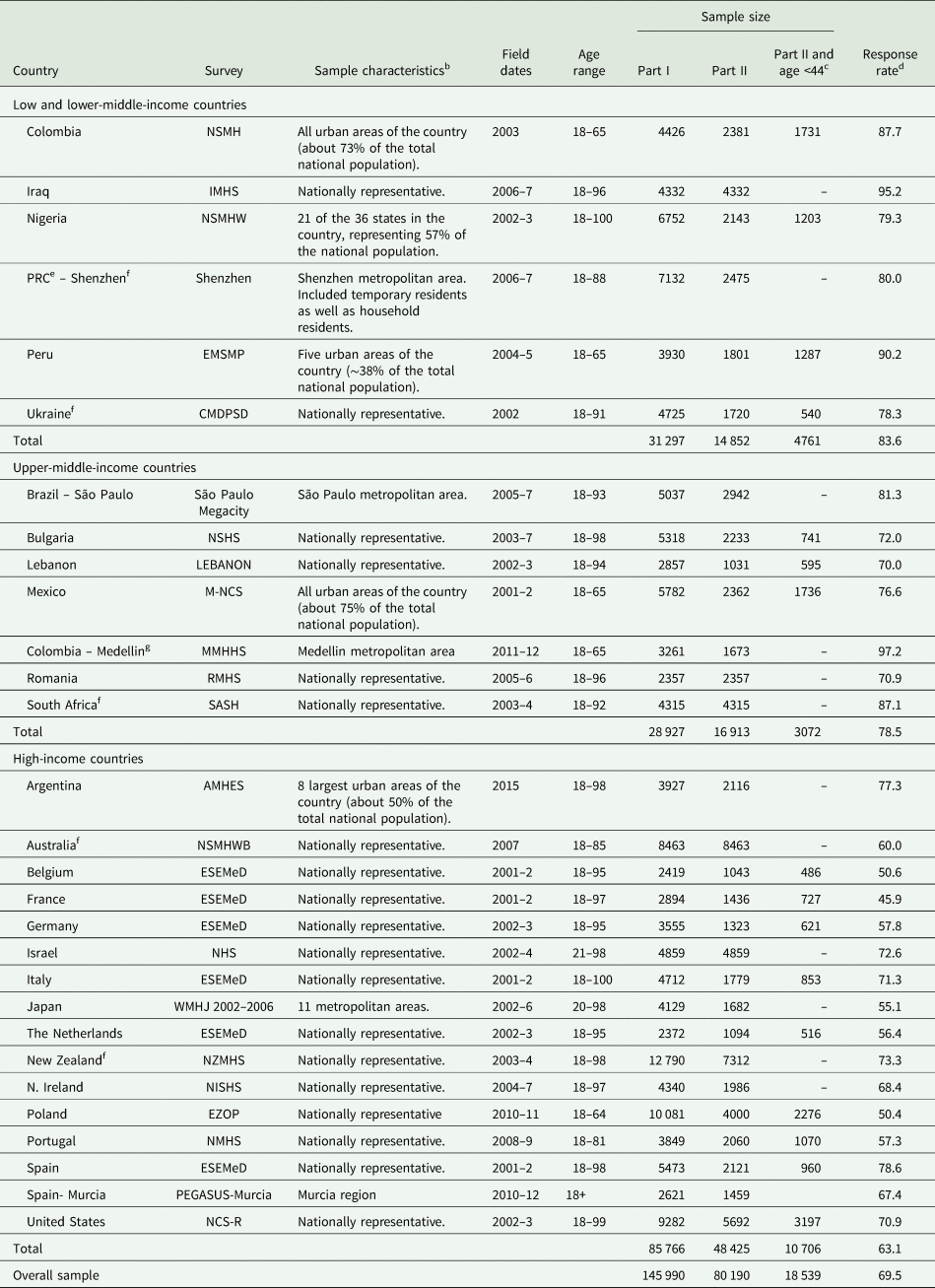
a The World Bank (2012) Data. Accessed 12 May 2012, at http://data.worldbank.org/country. Some of the WMH countries have moved into new income categories since the surveys were conducted. The income groupings above reflect the status of each country at the time of data collection. The current income category of each country is available at the preceding URL.
b Most WMH surveys are based on stratified multistage clustered area probability household samples in which samples of areas equivalent to counties or municipalities in the US were selected in the first stage followed by one or more subsequent stages of geographic sampling (e.g. towns within counties, blocks within towns, households within blocks) to arrive at a sample of households, in each of which a listing of household members was created and one or two people were selected from this listing to be interviewed. No substitution was allowed when the originally sampled household resident could not be interviewed. These household samples were selected using area probability design in all countries other than France (where telephone directories were used to select households) and the Netherlands (where postal registries were used to select households). Several WMH surveys (Belgium, Germany, Italy) used municipal resident registries to select respondents without listing households. The Japanese sample is the only totally un-clustered sample, with households randomly selected in each of the 11 metropolitan areas and one random respondent selected in each sample household. 21 of the 30 surveys are based on nationally representative household samples.
c Argentina, Australia, Brazil, Colombia-Medellin, Iraq, Israel, Japan, New Zealand, Northern Ireland, PRC – Shenzhen, Romania, South Africa and Spain-Murcia did not have an age restricted Part 2 sample. All other countries, with the exception of Nigeria, PRC (B-WMH; S-WMH), and Ukraine (which were age restricted to ⩽39) were age restricted to ⩽44.
d The response rate is calculated as the ratio of the number of households in which an interview was completed to the number of households originally sampled, excluding from the denominator households known not to be eligible either because of being vacant at the time of initial contact or because the residents were unable to speak the designated languages of the survey. The weighted average response rate is 69.5%.
e People's Republic of China.
f For the purposes of cross-national comparisons we limit the sample to those 18+.
g Colombia moved from the ‘lower and lower-middle-income’ to the ‘upper-middle-income’ category between 2003 (when the Colombian National Study of Mental Health was conducted) and 2010 (when the Medellin Mental Health Household Study was conducted), hence Colombia's appearance in both income categories. For more information, please see footnote a.
Time-dependent associations between mental disorders
Online Supplementary Fig. 3 shows the time-dependent HRs for all disorder pairs. Figure 2 shows the HR of later disorder depending on a previous onset of the prior disorder and the time since the onset of the prior disorder after adjusting for the type and number of comorbid disorders (model B) for selected pairs. Generally, respondents had the highest HRs in the first 2 years after the onset of the prior disorder. The risk of developing later disorder then fell slowly over time or plateaued out after 10 years. For example, after adjusting for comorbidity, the risk of developing GAD is 55 times greater in the initial year after developing major depression compared to those without (HR = 55.1, 95% CI = 51.0–59.6). Between 2 and 5 years after, the risk decreased by half (HR = 27.4, 95% CI = 25.3–29.7) and by 15 years, the risk was about one-eight in those with major depression compared to those without (HR = 6.6, 95% = 5.7–7.7).
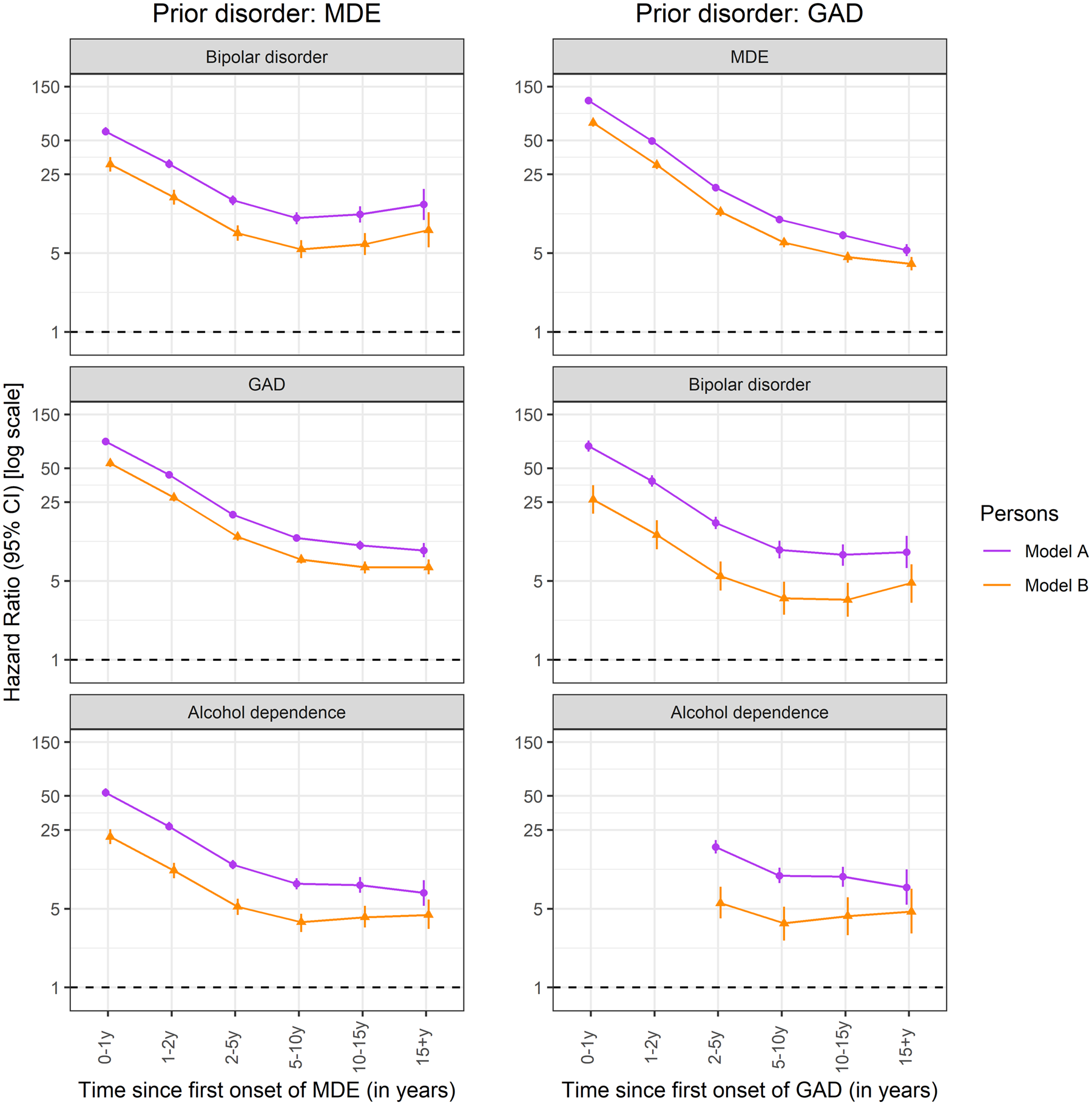
Fig. 2. Time-dependent (lagged) associations between prior disorders and subsequent later disorders.
Absolute risks
The absolute risks for all disorder pairs can be found in online Supplementary Fig. 4. Figure 3 shows the overall absolute risk of developing later disorder among respondents with a prior mental disorder for selected pairs. Each panel shows the overall absolute risks (solid orange line) and 95% CI (shaded area in grey – however often the line size masks the precise CIs). For many disorder pairs, the absolute risk of a subsequent disorder increased linearly and continued to increase over the period of observation (e.g. prior PTSD, and later MDE). Other disorder pairs have a small linear increase over the first few years, which then plateaued out over time (e.g. prior PTSD and later alcohol abuse) (see Fig. 3). The absolute risk of developing a subsequent disorder varies by sex in keeping with the sex ratio of the consistent mental disorders within the pairs (see online Supplementary Fig. 5). Interestingly, we found that the absolute risk of a subsequent disorder is generally higher among those who developed a prior disorder before 20 years of age (compared to those who have their onset 20 years or later, but who are followed up for a similar period) (see online Supplementary Fig. 6). Using Major Depressive Episode–Nicotine Dependence pair as an example, ~2% of the respondents developed nicotine dependence within 1 year of the onset of MDE. This risk increases to 22.7% 20 years after the initial onset of MDE and is higher for men (30.3%, 95% CI = 29.8–30.8) than for women (19.3%, 95% CI = 19.0–19.5%). The absolute risk of developing nicotine dependence 20 years after the initial onset of MDE is the highest in those with an early onset of MDE (onset of MDE aged <20 years = 32.7%, 95% CI = 32.3–33.1%). In those who have the onset of MDE between ages 20 and 40 years, the risk of nicotine dependence is 17⋅1% (95% CI = 16.8–17.4%). Finally, in those with the onset of MDE aged 40 years or older, the risk of nicotine dependence is only 7.0% (95% CI = 6.6–7.3%). (Note – these groups have each been followed for 20 years).
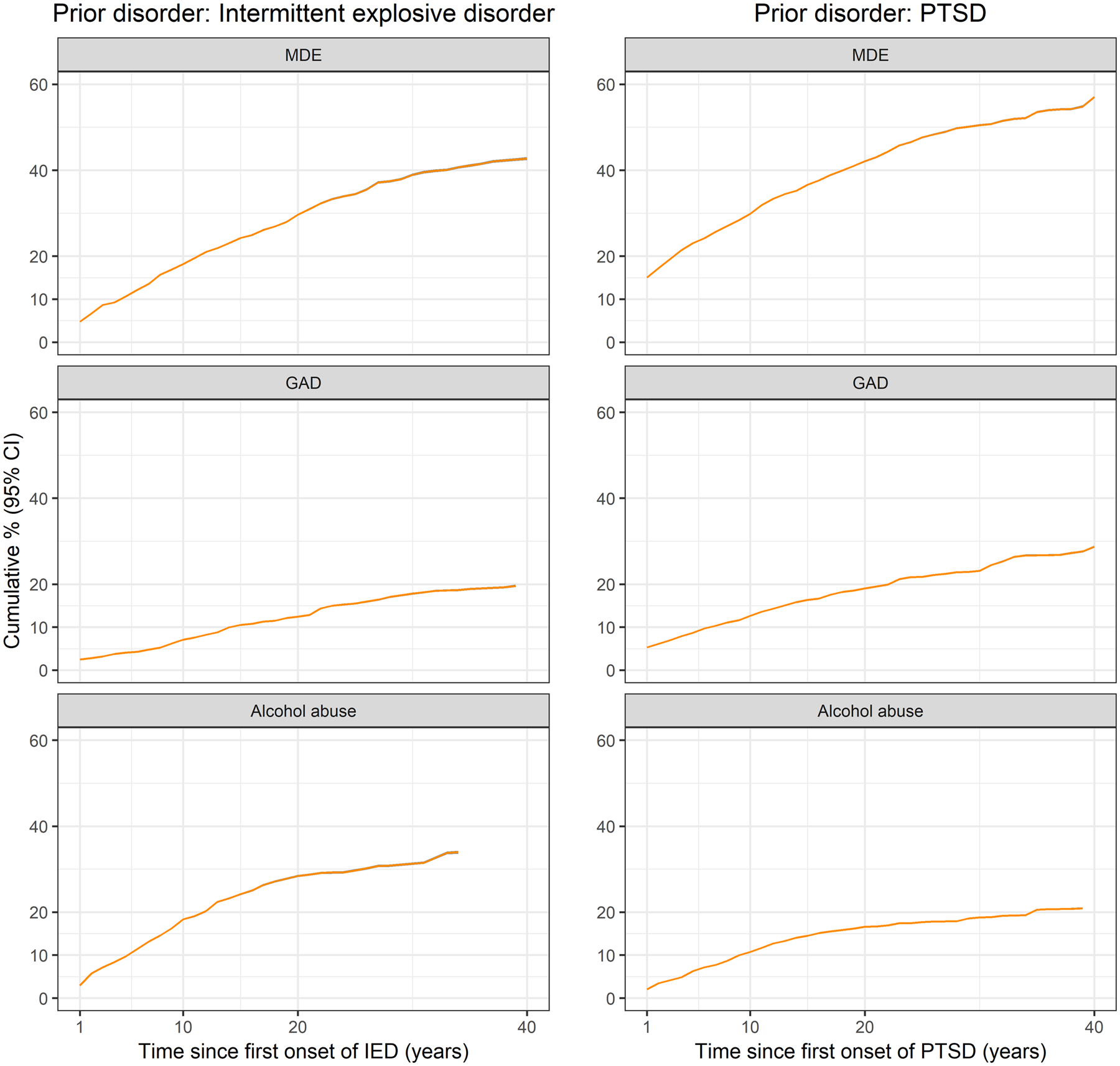
Fig. 3. Absolute risk of a subsequent disorder after developing a prior disorder.
Discussion
Based on survey data from many nations, we have provided a comprehensive map of pair-wise comorbidity within mental disorders. We confirm that the pair-wise comorbidity estimates from our cross-national study demonstrate the pervasive nature of comorbidity within mental disorders – the estimates were broadly consistent with those found in Danish registers (Plana-Ripoll et al., Reference Plana-Ripoll, Pedersen, Holtz, Benros, Dalsgaard, de Jonge, Fan, Degenhardt, Ganna, Greve, Gunn, Iburg, Kessing, Lee, Lim, Mors, Nordentoft, Prior, Roest, Saha, Schork, Scott, Scott, Stedman, Sorensen, Werge, Whiteford, Laursen, Agerbo, Kessler, Mortensen and McGrath2019b). The current study addresses several important gaps in the literature. First, in the current study, we provide estimates based on specific types of mental disorders as classified by DSM-IV criteria (our previous study was based on broad ICD-10 subchapters). Second, we demonstrate the very high risk of developing comorbidity between closely-related types of mental disorders. Third, the time-dependent HRs for the onset of each type of later-disorder show persistence over several decades. Finally, we confirm that some types of prior mental disorders were associated with appreciable absolute risks for later disorder over the following 30–40 years.
In keeping with prior studies based on the WMH Surveys, the increased risk of comorbidity was pervasive across all types of disorder pairs (Kessler et al., Reference Kessler, Chiu, Demler, Merikangas and Walters2005, Reference Kessler, Avenevoli, McLaughlin, Green, Lakoma, Petukhova, Pine, Sampson, Zaslavsky and Merikangas2012, Reference Krueger, Kotov, Watson, Forbes, Eaton, Ruggero, Simms, Widiger, Achenbach, Bach, Bagby, Bornovalova, Carpenter, Chmielewski, Cicero, Clark, Conway, DeClercq, DeYoung, Docherty, Drislane, First, Forbush, Hallquist, Haltigan, Hopwood, Ivanova, Jonas, Latzman, Markon, Miller, Morey, Mullins-Sweatt, Ormel, Patalay, Patrick, Pincus, Regier, Reininghaus, Rescorla, Samuel, Sellbom, Shackman, Skodol, Slade, South, Sunderland, Tackett, Venables, Waldman, Waszczuk, Waugh, Wright, Zald and Zimmermann2018). Despite the substantial methodological differences between the current study and the prior studies (e.g. international v. single nation; DSM-IV specific disorders v. ICD-10 broad subchapters; register-based diagnoses v. population-based survey), the overall pattern of findings was striking – each type of prior mental disorder was associated with an increased risk of most other types of mental disorders. In particular, we confirm very high risks for individuals with pairs of closely-related disorders (e.g. bulimia nervosa and subsequent binge eating disorder) (Kotov et al., Reference Kotov, Krueger and Watson2018). Closely-related disorders often share symptoms; thus, it is feasible that respondents may have an imperfect recall for the precise sequence of such disorders. Previous studies based on the WMH surveys have identified that people with one type of prior disorder (e.g. an internalising disorder) were more likely to develop subsequent additional internalising disorders (in contrast to subsequent externalising disorders) (Kessler et al., Reference Kessler, Cox, Green, Ormel, McLaughlin, Merikangas, Petukhova, Pine, Russo, Swendsen, Wittchen and Zaslavsky2011).
In keeping with our prior register-based study (Plana-Ripoll et al., Reference Plana-Ripoll, Pedersen, Holtz, Benros, Dalsgaard, de Jonge, Fan, Degenhardt, Ganna, Greve, Gunn, Iburg, Kessing, Lee, Lim, Mors, Nordentoft, Prior, Roest, Saha, Schork, Scott, Scott, Stedman, Sorensen, Werge, Whiteford, Laursen, Agerbo, Kessler, Mortensen and McGrath2019b), the time-dependent HRs between mental disorder pairs confirmed that the risk of later-disorder was substantially higher within the first 1–2 years after the onset of the prior-disorder (compared to longer intervals). The Danish study identified very large HRs within the first 6 months of the prior disorder, perhaps reflecting Berkson's bias (Snoep et al., Reference Snoep, Morabia, Hernández-Díaz, Hernán and Vandenbroucke2014). The current estimates within the first 6–12 months were more conservative and plausible. Mindful that the surveys were cross-sectional, and the recollection of lifetime psychiatric history may be imperfectly recalled (especially for long passed events), the two studies provide convergent evidence for the persistent nature of the increased risk of comorbidity. In general, regardless of the source of the data (longitudinal registers or cross-sectional recall), the risk of subsequent mental disorders remained persistently elevated over the entire period of observation (at least 15 years). These findings lend weight to the hypothesis that a wide spectrum of mental disorders has a shared risk factor background (which includes genetic and non-genetic factors) (Caspi and Moffitt, Reference Caspi and Moffitt2018; Hyman, Reference Hyman2019).
The study provides important new insights into the absolute risk of developing later disorders over several decades. For example, in those with prior MDE, the risk of subsequently developing GAD was appreciable, with absolute risks (and 95% CIs) at 5, 10 and 15 years of 8.9%, (8.8–9.0%), 11.4% (11.3–11.4%) and 13.6% (13.6–13.7%), respectively. Conversely, in those with prior GAD, the risk of subsequent MDE was even more pronounced with absolute risks (95% CIs) at 5, 10, 15 years of 28.2% (28.0–28.4%), 37.7% (37.5–38.0%) and 46.9% (46.6–47.1%). Finally, we note that people with early-onset mental disorders (<20 years) are more likely to develop other types of mental disorders within a set time frame, compared to those who have their first mental disorder at older ages. These findings are salient in light of recent increased investments in youth mental health services and clinical staging models (Iorfino et al., Reference Iorfino, Scott, Carpenter, Cross, Hermens, Killedar, Nichles, Zmicerevska, White, Guastella, Scott, McGorry and Hickie2019), and highlight the need to invest in programs that may reduce the burden of additional comorbidity in this vulnerable group (Kessler and Price, Reference Kessler and Price1993).
Our study has several important strengths. Surveys allow for the detection of both treated and untreated mental disorders (in contrast, the Danish register-based study was unable to identify mental disorders treated exclusively by primary practitioners, or those who did not seek treatment). Furthermore, the WMH surveys were based on the CIDI, which is designed to assess mental disorders against established diagnostic criteria, with quality control mechanisms related to training and interviewer fidelity. We know that the lifetime prevalence of mental disorders can vary between countries (Kessler et al., Reference Kessler, Angermeyer, Anthony, De Graaf, Demyttenaere, Gasquet, De Girolamo, Gluzman, Gureje, Haro, Kawakami, Karam, Levinson, Medina Mora, Oakley Browne, Posada-Villa, Stein, Adley Tsang, Aguilar-Gaxiola, Alonso, Lee, Heeringa, Pennell, Berglund, Gruber, Petukhova, Chatterji and Ustün2007) and broad socioeconomic and cultural factors impact on the profiles of some types of mental disorders (e.g. substance use disorders are less common in some countries). The current study included surveys from 27 nations, and analyses were adjusted by the site in order to focus on cross-national findings. We believe that the estimates from the current study are more generalisable across sites.
We wish to draw attention to several limitations. Despite the relatively large sample, for many disorder pairs we lacked sufficient power to generate reliable estimates, and (in contrast to the Danish study) were not able to generate age- and sex-specific estimates for many of the disorder pairs. Survey data relies on the respondent's memory and recall bias may result in a systematic bias against the recall of temporally distant events. Respondents interviewed as adults may conflate the age of onset of two or more disorders (especially if the disorders shared symptoms). In our study, this bias could inflate the number of ties (where respondents report the onset of two or more disorders during the year). While we used a conservative strategy to break ties, this bias cannot influence HRs estimates when the lag is 2 or more years. In addition, while we have the age of onset of each type of disorder, detailed information about the course of each disorder was not available. The surveys included in our analyses were conducted from 2001 to 2015, and it is feasible that the prevalence of the underlying disorders and related patterns of comorbidity may have changed over time. Finally, this study only concentrated on pairs of disorders (with and without adjustment for additional prior disorders). We plan to explore more complex permutations of comorbidity within mental disorders in future studies.
To the best of our knowledge, this is the first study to provide a comprehensive set of age- and sex-specific estimates of absolute risks of comorbidity within DSM-IV mental disorders. We have also provided an interactive data visualisation tool that may assist clinicians in planning management protocols and monitoring potential emergent comorbidity over time. These estimates may have clinical utility – they can remind the clinician to remain vigilant for the emergence of additional types of mental disorders. We hope that our findings will guide future hypothesis-driven research related to the mechanisms underlying the patterns of comorbidity within mental disorders.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796020000633.
Data
Due to data-sharing restrictions contained in some individual country agreements with the World Mental Health Surveys Initiative, sharing of the cross-national dataset is not possible.
Acknowledgements
We acknowledge the collaborators of the WHO World Mental Health Survey (see website for full details https://www.hcp.med.harvard.edu/wmh/).
Financial support
The World Health Organization World Mental Health (WMH) Survey Initiative is supported by the US National Institute of Mental Health (NIMH; R01 MH070884), the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864, and R01 DA016558), the Fogarty International Centre (FIRCA R03-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical Inc., GlaxoSmithKline and Bristol-Myers Squibb. We thank the staff of the WMH Data Collection and Data Analysis Coordination Centres for assistance with instrumentation, fieldwork, and consultation on data analysis. The Argentina survey – Estudio Argentino de Epidemiología en Salud Mental (EASM) – was supported by a grant from the Argentinian Ministry of Health (Ministerio de Salud de la Nación). The São Paulo Megacity Mental Health Survey is supported by the State of São Paulo Research Foundation (FAPESP) Thematic Project Grant 03/00204-3. The Bulgarian Epidemiological Study of common mental disorders EPIBUL is supported by the Ministry of Health and the National Centre for Public Health Protection. The Shenzhen Mental Health Survey is supported by the Shenzhen Bureau of Health and the Shenzhen Bureau of Science, Technology, and Information. The Colombian National Study of Mental Health (NSMH) is supported by the Ministry of Social Protection. Implementation of the Iraq Mental Health Survey (IMHS) and data entry were carried out by the staff of the Iraqi MOH and MOP with direct support from the Iraqi IMHS team with funding from both the Japanese and European Funds through United Nations Development Group Iraq Trust Fund (UNDG ITF). The World Mental Health Japan (WMHJ) Survey is supported by the Grant for Research on Psychiatric and Neurological Diseases and Mental Health (H13-SHOGAI-023, H14-TOKUBETSU-026, H16-KOKORO-013, H25-SEISHIN-IPPAN-006) from the Japan Ministry of Health, Labour and Welfare. The Lebanese Evaluation of the Burden of Ailments and Needs Of the Nation (L.E.B.A.N.O.N.) is supported by the Lebanese Ministry of Public Health, the WHO (Lebanon), National Institute of Health/Fogarty International Centre (R03 TW006481-01), anonymous private donations to IDRAAC, Lebanon and unrestricted grants from, Algorithm, AstraZeneca, Benta, Bella Pharma, Eli Lilly, Glaxo Smith Kline, Lundbeck, Novartis, OmniPharma, Pfizer, Phenicia, Servier, UPO. The Nigerian Survey of Mental Health and Wellbeing (NSMHW) is supported by the WHO (Geneva), the WHO (Nigeria), and the Federal Ministry of Health, Abuja, Nigeria. The Northern Ireland Study of Mental Health was funded by the Health & Social Care Research & Development Division of the Public Health Agency. The Peruvian World Mental Health Study was funded by the National Institute of Health of the Ministry of Health of Peru. The Polish project Epidemiology of Mental Health and Access to Care –EZOP Project (PL 0256) was supported by Iceland, Liechtenstein and Norway through funding from the EEA Financial Mechanism and the Norwegian Financial Mechanism. EZOP project was co-financed by the Polish Ministry of Health. The Portuguese Mental Health Study was carried out by the Department of Mental Health, Faculty of Medical Sciences, NOVA University of Lisbon, with the collaboration of the Portuguese Catholic University, and was funded by Champalimaud Foundation, Gulbenkian Foundation, Foundation for Science and Technology (FCT) and Ministry of Health. The Romania WMH study projects ‘Policies in Mental Health Area’ and ‘National Study regarding Mental Health and Services Use’ were carried out by National School of Public Health & Health Services Management (former National Institute for Research & Development in Health), with technical support of Metro Media Transilvania, the National Institute of Statistics-National Centre for Training in Statistics, SC, Cheyenne Services SRL, Statistics Netherlands and were funded by Ministry of Public Health (former Ministry of Health) with supplemental support of Eli Lilly Romania SRL. The South Africa Stress and Health Study (SASH) is supported by the US National Institute of Mental Health (R01-MH059575) and the National Institute of Drug Abuse with supplemental funding from the South African Department of Health and the University of Michigan. Dr Stein is supported by the Medical Research Council of South Africa (MRC). The Ukraine Comorbid Mental Disorders during Periods of Social Disruption (CMDPSD) study is funded by the US National Institute of Mental Health (RO1-MH61905). The US National Comorbidity Survey Replication (NCS-R) is supported by the National Institute of Mental Health (NIMH; U01-MH60220) with supplemental support from the National Institute of Drug Abuse (NIDA), the Substance Abuse and Mental Health Services Administration (SAMHSA), the Robert Wood Johnson Foundation (RWJF; Grant 044708) and the John W. Alden Trust. None of the funders had any role in the design, analysis, interpretation of results, or preparation of this paper.
Conflict of interest
In the past 3 years, Dr Kessler received support for his epidemiological studies from Sanofi Aventis; he was a consultant for Datastat Inc., Johnson & Johnson Wellness and Prevention, Sage Pharmaceuticals, Shire, Takeda; and served on an advisory board for the Johnson & Johnson Services Inc. Lake Nona Life Project. Dr Stein has received research grants or consultancy honoraria from Lundbeck and Sun.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000.






