Introduction
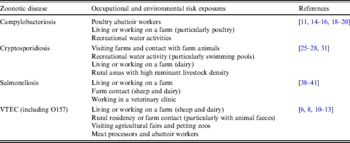
Each year, foodborne diseases account for an estimated 1·3 million cases in England and Wales and 76 million cases in the USA [Reference Adak, Long and O'Brien1, Reference Mead2], with four of the most important pathogens responsible for foodborne illnesses being zoonotic (Campylobacter spp., Salmonella spp., Cryptosporidium spp. and verocytotoxin-producing Escherichia coli (VTEC), particularly E. coli O157). In addition to causing acute diarrhoeal symptoms, infection may lead to more severe complications, e.g. haemolytic uraemic syndrome from E. coli O157, and Guillain–Barré syndrome from Campylobacter infection. Although many cases of human salmonellosis, campylobacteriosis, cryptosporidiosis and E. coli O157 infections are foodborne or waterborne, both outbreak and sporadic infections have been linked with the veterinary surgeries and the farming environment and a number of associated risk exposures have been identified (Table 1). Here we consider the environmental pathways associated with prolonged antigenic exposure and assess the role of occupational exposure in susceptibility to zoonotic pathogens. We discuss the significance of asymptomatic carriage in disease outbreaks, and explore the epidemiological implications of asymptomatic carriage on disease management.
Table 1. Occupational and environmental risk exposures associated with gastrointestinal zoonotic pathogens

VTEC, Verocytotoxin-producing Escherichia coli.
Zoonoses are infectious diseases that are transmissible from vertebrate animals to humans. In many countries, the reporting of most zoonotic illness has traditionally been voluntary and therefore laboratory-confirmed zoonotic cases probably account for only a small fraction of those occurring in the community. Farm workers, veterinarians and abattoir workers, who have more repeated contact with animals than almost any other occupational group, have a higher potential risk of contracting zoonotic illnesses. Seroprevalence studies have shown that these groups and their families are at risk of exposure to a significant number of zoonoses [3–Reference Whitney5]. However, frequent and recurrent occupational exposure to zoonoses can result in reduced occurrence of clinical illness due to a build-up of immunity; consequently it has been suggested that asymptomatic carriage of zoonoses is more likely in people whose occupation involves them working directly with domesticated or wild animals.
Despite the lack of clinical symptoms, individuals with apparent immunity can still be colonized by zoonotic pathogens [Reference Silvestro6], and could inadvertently facilitate disease transmission. A recent study from India demonstrated that children excreting viruses asymptomatically served as a significant source of infection because they were not restricted by illness [Reference Gladstone7]. The public health significance of this should not be underestimated as asymptomatically colonized individuals involved in the food supply chain will not necessarily alter their behaviour (e.g. due to diarrhoea) and could be responsible for the prolonged cycling and transmission of infectious diseases. The costs of illness to local health services and the wider economy associated with asymptomatic carriage are currently unknown. A better understanding of the scale of the role of asymptomatic carriage in disease burden would inform policy makers and allow a more accurate assessment of the value and cost-effectiveness of intervention strategies which would address it.
Recurrent occupational animal exposure and subclinical infection
E. coli O157
Circumstantial evidence suggests that occupational exposure to domesticated livestock can result in subclinical infection with VTEC. For example, a study in Canada found that 12% of dairy farm families possessed serum antibodies to the E. coli O157 lipopolysaccharide (LPS), although none of these subjects reported gastrointestinal symptoms at the time of sampling or a history of bloody diarrhoea or renal problems [Reference Wilson8]. Further evidence of asymptomatic carriage of VTEC in farm workers has led to the suggestion that a degree of immunity to clinical infection by E. coli O157 develops as a result of prolonged low-level exposure to less virulent VTEC strains [Reference Silvestro6]. This was supported by a retrospective serosurvey of healthy adult farm workers from the UK, which provided evidence of persisting antibodies to E. coli O157, particularly of the IgG class, suggesting long-term or repeated exposure to VTEC [Reference Evans9]. Further studies have shown elevated levels of antibodies to E. coli O157 LPS in dairy farm residents compared to urban residents [Reference Reymond10], and in farm-resident rural children compared to non-farm-resident children [Reference Belongia11]. Although the phenomenon of seropositivity and asymptomatic carriage of VTEC in farm workers has been well documented, the risk factors associated with carriage are still poorly understood [Reference Park12, Reference Quilliam13].
Campylobacter
While increased anti-Campylobacter jejuni antibodies are often detected in the sera of individuals who work with poultry [Reference Jones and Robinson14, Reference Price15] the risk of developing Campylobacter infection is much greater in inexperienced or temporary poultry farm workers [Reference Ellis16, Reference Wilson17]. In a serological study of poultry abattoir workers, long-term occupational exposure was accompanied by high levels of C. jejuni-specific IgG antibodies [Reference Cawthraw18]. Eight of these abattoir workers tested positive for faecal excretion of C. jejuni, with seven of them apparently asymptomatic, despite evidence for persistent excretion for up to 6 weeks. Occupational exposure to farm animals (e.g. cattle, sheep, poultry) and farm residency have also been identified as significant risk factors for Campylobacter infection [Reference Kapperud19–Reference Eberhart-Phillips21]. However, it has also been suggested that occupational contact with livestock or their faeces can provide protection against Campylobacter disease [Reference Adak22]. This is supported by a study in rural Wisconsin, which showed that 59% of children possessed antibodies to C. jejuni, with farm-residency and increasing age independently associated with seropositivity, despite no corresponding increase in clinically recognized diarrhoeal illness compared to non-farm-resident children [Reference Belongia11]. Other factors associated with seropositivity included contact with cattle and sheep and drinking unpasteurized milk, which in previous studies has also been associated with elevated levels of antibodies and immunity to Campylobacter symptomatic infection [Reference Robinson and Jones23, Reference Blaser, Sazie and Williams24]. However, while frequent farm-related antigenic stimulation may offer a degree of protective immunity, this type of acquired immunity is often incomplete, dose-respondent, and can be overcome by exposure to novel antigenic serotypes.
Cryptosporidium
Infection with the protozoan parasite Cryptosporidium (Cr.) can cause gastrointestinal disease of clinical and economic significance in both humans and young farmed animals, with most human cases being caused by either Cr. hominis, or Cr. parvum. Several UK studies have provided evidence for the anthroponotic spread of Cr. hominis and the mainly zoonotic spread of Cr. parvum, with short visits to farms, handling cattle and touching farm animals being identified as independent risk factors [Reference Goh25–Reference Pollock27]. Furthermore, a quarter of all reported sporadic annual cases of Cr. parvum in England and Wales can be attributed to direct contact with farm animals [Reference Chalmers28]. Several seroepidemiological studies have found more positive subjects in rural settings than urban groups [e.g. 29, 30] and increased seroprevalence has been detected in dairy farmers compared to control subjects [Reference Lengerich31]. However, in a series of 790 sporadic cases in the UK between 2004 and 2006, only three cases were adults who had occupational farm contact (two farmers and one veterinary student), suggesting potential immunity in those frequently and historically exposed to animals and their faeces [Reference Chalmers28]. This contrasts with cryptosporidiosis outbreaks that regularly occur at swimming pools, day-care nurseries, open farms and similar settings which frequently involve children, and have been reported in veterinary students who have had limited prior exposure [Reference Gait32, Reference Chalmers and Davies33]. Frequent exposure through intermittent low-level contamination may lead to subclinical infection and some herd immunity [Reference Swift and Hunter34]. This is supported by evidence from a seroepidemiological study, which showed that people with high anti-cryptosporidial antibody levels were much less likely to self-report diarrhoeal disease than those with low levels of antibody [Reference Frost35]. Human infectivity studies have shown that although prior exposure does not provide complete protection against further infection, clinical symptoms are less severe [Reference Okhuysen36, Reference Chappell37] and age-related increases in seroprevalence appear to correlate well with the decline in incidence of clinical cryptosporidiosis [Reference Chappell37].
Salmonella
The routes of zoonotic transfer of Salmonella spp. include direct contact with farm animals or their faeces and exposure to a number of companion animals, particularly reptiles. Consequently, occupational exposure has been demonstrated in farm workers [Reference Fone and Barker38, Reference Baker39] and veterinarians [Reference Cherry40, Reference Wright41], although the type of practice, i.e. small or large animal practice, will determine the Salmonella serotypes personnel are exposed to. Although secondary transmission of Salmonella is a recurrent problem in animals at veterinary clinics, there have been no direct studies on the levels of immunity in veterinary personnel; however, a stool sample from an asymptomatic employee during one outbreak of salmonellosis at a veterinary clinic in the USA was found to be positive for S. Typhimurium [Reference Wright41]. Clearly the risks for zoonotic transfer are high in veterinary workers, although a recent report indicated that veterinarians rarely use personal protective equipment or adopt infection control practices to protect themselves against zoonotic disease transmission [Reference Wright42]. It remains unclear whether the occupational exposure to zoonoses experienced by veterinary workers results in a form of protection; and although several studies have linked the zoonotic spread of Salmonella from farm animals to farm workers, intriguingly there are as yet no reports of asymptomatic carriage in farm workers. Whether this is due to a lack of cumulative exposure, through common antigens from the range of different Salmonella serotypes present in animals (as suggested for acquired immunity to E. coli O157 [Reference Silvestro6]), or whether this is simply because there is a paucity of studies clearly needs further epidemiological investigation.
Acquired immunity and environmental exposure
Exposure to potentially ‘unhygienic’ environments and the onset of protective immunity has been discussed in the context of many diseases. For example, evidence of acquired, exposure-related, immunity comes from travellers from Western countries who often suffer from ‘traveller's diarrhoea’ on arrival in a developing country [Reference Shlim43–Reference Havelaar45]; however, their duration of stay is linearly correlated with protection from infection, indicating a build-up of immunity over time [Reference Hoge46]. This supports a widely reported phenomenon in the abattoir industry where new employees with a lack of previous exposure to a range of zoonotic pathogens, almost inevitably report gastrointestinal illness in the first few days of employment, with far fewer cases occurring in longer-term employees [Reference Cawthraw18, Reference Hong47]. Although the implications of abattoir workers asymptomatically carrying gastrointestinal zoonotic pathogens is not as immediately serious as subclinical infection in other types of food handlers, e.g. during the preparation of ready-to-eat products, asymptomatic individuals may well be significantly facilitating the transmission of zoonotic pathogens into the food chain.
While few studies directly compare the prevalence of zoonoses within populations of developing and developed countries, there is evidence for increased asymptomatic carriage of gastrointestinal pathogens in developing nations [Reference Hellard48, Reference Haffejee, Windsor and Moosa49]. Environmental pathways associated with prolonged antigenic exposure include the recurring consumption of contaminated drinking water and lower levels of hygiene during food preparation together with an increased environmental burden. This makes recurring cycles of infection with a range of zoonoses in the developing world more likely, with many reports ascribing the asymptomatic carriage of particular zoonotic pathogens (e.g. Campylobacter) to this constant antigenic exposure [Reference Havelaar45]. Although microbial stimulation plays an important role in modulating and improving the immune response against future challenges by infective agents, the levels of immunity to zoonoses in the developing world are acquired at the expense of considerable infant and child mortality, often due to diarrhoeal diseases.
Asymptomatic Campylobacter infections are considered endemic in developing countries, with symptomatic infection limited to children aged <2 years. A considerable number of studies have reported that breastfeeding can induce basal immunity against certain zoonotic pathogens, e.g. Campylobacter [Reference Morrow50], and as breastfeeding is widespread in the developing world, this may play an important role in the level of subclinical infection in children and asymptomatic carriage within a community. Conversely, evidence suggests that asymptomatic breastfeeding mothers can transfer certain zoonoses to their baby either directly, e.g. brucellosis [Reference Tikare, Mantur and Bidari51, Reference Celebi52] or indirectly, e.g. Helicobacter pylori [Reference Clemens53].
A large Iranian study conducted on faecal samples from children revealed that a significant proportion (7·2%) were asymptomatically shedding strains of enterotoxigenic E. coli (ETEC) known to cause diarrhoea [Reference Alikhani54]. A systematic review on the aetiological role of ETEC in children with diarrhoea in the developing world found that colonization in the 0–4 years age group was a significant risk factor for contracting diarrhoea [Reference Wenneras and Erling44]. There also existed high rates of ETEC in children aged >5 years; however, these children were asymptomatic with a notable decrease in the frequency of diarrhoea. Enterohaemorrhagic E. coli O157, which has recently become a serious zoonotic pathogen in industrialized nations, appears to be a relatively uncommon causative agent of illness in developing countries. Whether this is due to this particular strain of E. coli being relatively new, or whether people in developing countries have already acquired a significant amount of immunity to it clearly warrants further investigation.
Genetic variation in human populations also plays an important role in susceptibility to infectious diseases, with several genetically determined factors influencing susceptibility to specific infections, e.g. Norwalk virus [Reference Lindesmith55]. However, the role of genetic variation in determining resistance to infection by zoonotic pathogens remains unclear, although evidence from genetic epidemiological studies has demonstrated that immunity to disease usually arises from a complex interaction of environmental, pathogen and host genetic factors [Reference Burgner, Jamieson and Blackwell56]. Genetically controlled host defence factors can affect the susceptibility of individuals to zoonotic challenge, e.g. individuals unable to produce or respond to interferon-gamma [Reference Ottenhoff57]. Genetic factors can also alter innate immunity, e.g. the heterogeneous condition hypogammaglobulinaemia can lead to repeated infection and prolonged symptoms from a range of pathogens, including zoonoses [Reference Janssen58].
Comparing the incidence of zoonoses in immigrant and resident populations may help to understand acquired immunity, although these studies need to be treated with caution as they can often be influenced by confounding factors. An example of this occurred during the largest ever outbreak of Q fever in the UK, where no cases were reported in the local Asian community despite there being many cases in the same area in the non-Asian community [Reference Hawker59]. Although it was hypothesized that cultural factors partially explained this observation, serosurvey data provided evidence for an underlying immunity as many members of the Asian community had originated from areas of Pakistan with high rates of Coxiella burnetii infection in sheep [Reference Hawker59]. Factors other than environmental exposure can also affect susceptibility, e.g. socioeconomic status, which is an important co-factor for the prevalence of H. pylori in the US adult population [Reference Everhart60]. The available evidence for the occurrence of subclinical infections demonstrates that they can be multifactorial and may be related to the type or level of exposure, the presence of potential immunity in the host, or agent-specific factors, such as genotypic variation in virulence. Whatever the mechanism, the presence of subclinical zoonotic infections in human populations, together with associated asymptomatic carriage, gives rise to a number of important issues for the epidemiology and control of these diseases.
Community epidemiology and the public health significance of subclinical zoonotic infections in humans
The emergence of several zoonotic diseases of major public health significance, e.g. swine influenza A(H1N1), E. coli O157, vCJD, and SARS, have highlighted the importance of early surveillance. Essential to mitigating the spread of communicable diseases is the implementation of control measures, which includes horizon-scanning and risk assessment. However, the presence of subclinical cases can present a barrier to effective disease control as infections often escape detection. Subsequently, under-ascertainment of cases may underestimate the extent of an outbreak, and facilitate continued transmission, or lead to bias in an epidemiological investigation, e.g. by the misclassification of controls in case-control studies. Further, the presence of subclinical or mild infection in a proportion of hosts may provide an evolutionary advantage to an emerging pathogen, facilitating onward transmission within animal and/or human populations. Asymptomatic carriers can still excrete infective organisms, and may pass the infection on to others, although for gastrointestinal infections, transmission is more likely from clinical cases, especially where cases exhibit diarrhoea (Fig. 1).

Fig. 1. Infection pathways and potential for the maintenance of asymptomatic carriage of gastrointestinal zoonotic pathogens.
Person-to-person spread of zoonoses is most usually considered in the control of gastrointestinal infections such as Salmonella and E. coli O157. Horizontal transmission of E. coli O157 spread via the faecal–oral route, can occur in families and in the wider community. However, secondary transmission of salmonellosis during outbreaks may vary depending on the outbreak setting and the strain of pathogen, and is often dependent on the population at risk. In a large outbreak on the Navajo Nation Indian Reserve in the USA, which involved 3400 cases, no secondary infections were reported [Reference Horowitz61], whereas in hospital outbreaks in the UK during the 1980s person-to-person transmission was a significant factor [Reference Palmer and Rowe62]. Secondary transmission of E. coli O157 is relatively common [Reference Parry and Salmon63], and of 157 cases identified in a school outbreak in Wales, UK, 48 cases were attributed to secondary transmission [Reference Pennington64]. By contrast, person-to-person spread of Campylobacter is rare and family clusters are seldom seen [Reference Cowden65], and although secondary transmission following point-source outbreaks does occur, it is uncommon [Reference Evans66]. In a recent outbreak of E. coli O157 on a petting farm in the UK, of 93 cases of illness, 65 were attributed to primary infection, 13 to secondary infection and 15 were asymptomatic cases [67]. While it is theoretically possible that some of the secondary cases of infection could be linked to direct person-to-person spread from some of the asymptomatic cases, quantifying this risk during an outbreak scenario would prove very difficult. However, the potential for asymptomatic human carriage as an epidemiological variable should not be discounted [Reference David68].
Guidelines exist in the UK for the prevention of person-to-person spread of gastrointestinal infections in general [69], and E. coli O157 in particular [70]. These guidelines consider the public health management of cases and contacts and the control of secondary transmission. Special attention is given to hygiene precautions, such as hand washing, decontamination, exclusion from work, school and other institutional settings, and identifying population groups at greater risk of spreading infection, e.g. children aged <5 years attending pre-school facilities, people working with ready-to-eat food and health and social care staff who have direct contact with individuals, for whom a gastrointestinal infection could have serious consequences. Outbreaks in children's nurseries in which an explicit link between human asymptomatic carriers of E. coli O157 and person-to-person infection have been reported [Reference Al-Jader71]. Given the frequency of secondary transmission by E. coli O157, and the potential severity of outcomes of infection, the prompt separation of primary cases of E. coli O157 from young household contacts has been recommended [Reference Werber72].
The theoretical possibility of person-to-person infection from asymptomatic carriers poses a significant demand on the monitoring and control of disease outbreaks. Methicillin-resistant Staphylococcus aureus (MRSA) is an example of a disease with evidence of asymptomatic person-to-person infection, e.g. healthcare workers [Reference Albrich and Harbarth73], and recent reports also suggest a zoonotic pathway through professional contact with animals [Reference Voss74–Reference Huber76]. Asymptomatically colonized individuals can transmit MRSA to others [Reference Meier77], and in so doing can unknowingly act as reservoirs for the disease [Reference Albrich and Harbarth73], particularly in nosocomial situations [Reference Blok78–Reference Grundmann81]. Although the infection pathways for zoonotic MRSA transmission are different to E. coli O157, Salmonella, Campylobacter and Cryptosporidium, the role of occupational exposure, asymptomatic carriage and person-to-person spread of MRSA gives rise to a number of important implications relating to the control and surveillance of gastrointestinal zoonotic diseases.
Livestock farmers and veterinarians in this context are an occupational group analogous to healthcare workers and should be considered at risk of becoming asymptomatic carriers due to their regular handling of potentially infected animals. Therefore, protective measures for this group are important [Reference Garcia-Graells82]; although approaches proposed for healthcare workers in hospital settings, e.g. regular screening and decolonization of carriers [Reference Cookson83], would be impractical for workers in the livestock sector. Screening farmers for occupationally acquired diseases would be logistically problematical owing to the number of farms, their type and the practicality of regularly screening in geographically isolated locations. Veterinarians pose a potentially greater threat for the dispersal of these types of pathogen than farmers due to their multiple daily farm visits, and subsequently have greater potential for asymptomatic person-to-person contact within the more densely populated urban and semi-urban communities.
The importance of asymptomatic carriage in causing secondary infection was highlighted during a retrospective cohort study following an outbreak of E. coli O157 in the UK [Reference Werber72]. Although it would be fairly straightforward to set up a similar study to quantify the spread of zoonoses from primary symptomatic cases to asymptomatic secondary cases, future epidemiological investigations need to focus on quantifying the spread from asymptomatic carriers. However, identifying clinical cases that result from the secondary transmission from asymptomatic primary cases would be chronologically difficult during an outbreak setting, as the investigation usually begins with the symptomatic case.
Potential mitigation strategies
If asymptomatic carriers are a source of infection then there may be an economic case for identifying and treating asymptomatic carriage if the costs of screening and treatment are less than the costs of identifying and treating those individuals infected by asymptomatic hosts. One strategy to encourage high-risk occupational groups to seek tests and treatment would be to impose penalties and/or positive incentives. The latter could involve payment for regular screening for high-risk asymptomatic carriage groups such as veterinarians. However, surveillance of veterinarians and farmers may prove to be controversial and a need to adhere to strict confidentiality guidelines essential [Reference Catry84]. As a control measure the weekly self-screening of veterinarians appears to be technically feasible and coupled with an overall improvement in hygiene practices may provide sufficient protection from transmitting both clinical and subclinical infections [Reference Wright42, Reference Catry84]. Schemes which aim to reduce the risk posed by asymptomatic carriers in the food chain are mostly not predicated on the assumption that there is some intervention that will remove gastrointestinal zoonotic pathogens from asymptomatic hosts. Rather, those hosts are removed from food handling until such time as the organism can no longer be recovered from their stool. Such interventions are not available for all zoonoses, and even if they were, they would need to be taken regularly in order to counter host re-colonization. The imposition of any programme aimed at reducing the risk from asymptomatic carriers may be best focused on groups with a higher risk of transmitting zoonoses to others and lower probabilities of infection, e.g. farmers and veterinarians.
In theory, a prospective cohort study could be set up following a cohort of high-risk individuals (high risk of acquiring a zoonotic infection with a low risk of clinical symptoms, but a high risk of transmitting it on) and collecting detailed information about their contacts. In practice, this would probably need a large number of people, as risk of secondary spread would be low, and would therefore not be practical. Another approach would be to simply screen a healthy occupational cohort for markers of infection, screen the contacts of both positives and negatives and simply examine statistically whether contacts of positives are more likely to be positive. However, this would likely be confounded by the fact that contacts would have other common sources of infection, rather than linearly transmitting to each other.
The effective management of such diseases is contingent upon substantive empirical information underpinning policy decisions. The nature of emerging diseases often requires policy makers and scientists to make choices about disease control in the absence of hard empirical data. Although when the efficacy of a large number of intervention strategies requires such thorough evaluation the task can be cognitively taxing. To overcome such obstacles recent research has employed a range of innovative techniques including the market research tool ‘Best-Worst Scaling’ designed to facilitate the elicitation of opinion from both health experts and land managers. The common objective of such an approach is to identify interventions considered both effective in the control of pathogen movement within the wider environment and practical to implement [Reference Cross, Rigby and Edwards-Jones85]. The compliance of key stakeholders such as farmers and veterinarians, however, is critical to successful policy implementation.
This review has highlighted a number of important gaps in our knowledge about the significance of asymptomatic carriage and subclinical infection, and exposed a lack of understanding about the risks posed by subclinical infection in different parts of the food chain from field to fork. This includes the rate of asymptomatic carriage in different occupational groups (farmers, veterinarians, abattoir and processing workers, food manufacturers and handlers) and the risk of person-to-person transmission from asymptomatic carriers. It is therefore essential that future research is concentrated towards understanding the role occupational exposure and asymptomatic carriage play in outbreak scenarios and the epidemiological significance of subclinical infection in the community.
ACKNOWLEDGEMENTS
This research was undertaken as part of a project funded under the UK Research Councils’ Rural Economy and Land Use (Relu) programme entitled ‘Reducing E. coli O157 Risk in Rural Communities’ (RES-229-31-0003). Relu is funded jointly by the Economic and Social Research Council, the Biotechnology and Biological Sciences Research Council and the Natural Environment Research Council, with additional funding from the Department for Environment, Food and Rural Affairs and the Scottish Government.
DECLARATION OF INTEREST
None.