INTRODUCTION
The influenza pandemic of 1918–1919 was one of the most lethal infectious disease events ever recorded. Evidence indicating protection from mortality during the 1918–1919 pandemic could inform public health preparations for future pandemics. Living in a rural setting has been found to be associated with reduced mortality during the 1918–1919 pandemic in a number of previous studies [Reference McSweeny1–3]. In British Commonwealth military populations in 1918 veterans appeared relatively protected from death due to influenza and pneumonia compared to recent recruits [Reference Shanks4]. Age is an important potential confounder considering the age-specific mortality observed during the 1918–1919 pandemic, when there was a peak in mortality centred around age 30 years [Reference Vaughn, Vaughn and Palmer5]. In this study data from both civilian and military populations from the same geographic areas were used to further investigate urban and rural differences in mortality, as well as the apparent protective effect due to time in military service, controlling both for age. The aim of this study was to investigate (1) whether higher mortality in urban civilian populations was due to the urban environment or due to intrinsic host susceptibility in people of urban origin; and (2) whether reduced mortality in military veterans was due to the same mechanism.
METHODS
We conducted analyses using six datasets concerning deaths during the 1918 influenza pandemic: three concerning civilian deaths and three concerning military deaths. Civilian data were available for the states of Indiana and Kansas, USA, and New South Wales (NSW), Australia. Military data were available for Indiana and Kansas, USA, and for Australian soldiers from NSW, Queensland and Victoria. Individual-level data were available for the Australian military cohort; aggregate-level data were available otherwise.
Civilian data
Data on civilian deaths that were due to influenza and pneumonia and occurred in adult males aged 18–44 years in Indiana and Kansas between September and December 1918 were available from a special survey by the US Census Bureau [6]. The number of civilians at risk was calculated from the 1920 US census. An individual was defined as an urban resident if they resided in a town with a population >10 000 in 1910; remaining individuals were defined as rural residents. The number of civilian deaths, and risk of death, due to influenza that occurred between January and September 1919 in NSW were taken directly from the report of the NSW Director-General of Public Health [3]. An individual was defined as an urban resident if they resided in the Sydney metropolitan district, and as a rural resident otherwise.
Military data
Military deaths due to influenza or pneumonia between October and December 1918 in soldiers recruited from Indiana and Kansas were taken from special memorial books issued by the respective states. The number of soldiers at risk was calculated from selective service records [7, 8]. A soldier was defined to be of urban origin if they were a resident of a town with population >25 000 in 1910, and to be of rural origin if they were a resident of a county which contained no towns with a population >10 000 in 1910.
Individual-level data for soldiers from NSW, Queensland and Victoria were extracted from a previous case-control study [Reference Shanks4]. All military deaths (cases) due to influenza or pneumonia between October 1918 and March 1919 are included. Controls were selected randomly from all Australian soldiers who survived the 1918–1919 pandemic period and returned to Australia. Individual-level records were used in this analysis if urban/rural origin could be estimated. A soldier was defined to be of urban origin if their place of enlistment was located within a central postcode of a major city, and of rural origin if their place of enlistment had the postcode of a country town.
Formal institutional ethical clearance was provided from the University of Queensland Human Research Ethics Committee number 2007001146 dated 29 August 2007.
Statistical analysis
For each dataset we computed the risk of mortality according to urban/rural origin, and calculated relative risk of death by urban/rural origin. All civilian data, and military data from the USA were available only as aggregate data, and definitions of urban/rural origin differ. For this reason, as well as the presumably different methods used for estimating both case numbers and denominators, no comparisons were attempted between populations, only within them.
We undertook a multivariable analysis using the Australian data as individual-level data were available. Urban/rural origin, length of time in the military, and birth year were included as covariables. Length of time in the military was categorized as either veteran (enlisted in 1914–1917) or non-veteran (enlisted in 1918). The years 1914–1917 were grouped together as previous analysis has shown that mortality from influenza or pneumonia was similar in soldiers recruited in each of these years, but much higher in soldiers recruited in 1918 [Reference Shanks4]. Birth year was categorized as 1888 or earlier, 1889–1891, and 1892 or later. We investigated the significance of the interaction between each pair of main effects in predicting mortality by adding the interaction term to a model involving all main effects and tested its significance using the likelihood ratio test. In the presence of interactions, stratified analyses were performed to determine the effect of urban/rural origin. We investigated the interaction between age and both urban/rural origin and veteran/non-veteran status to assess whether the effect of urban/rural origin or veteran status varied with birth year. We investigated the interaction between urban/rural origin and veteran/non-veteran status to assess whether these exposures might have separate effects on mortality. Data were analysed using Stata v. 11.1 (StataCorp, USA).
RESULTS
Aggregated information was available on 602 798 civilian male adults and 50 979 soldiers from Indiana, and on 365 403 civilian male adults and 39 801 soldiers from Kansas. Individual-level information was available on 1482 Australian soldiers. Among civilian populations in Indiana, Kansas and NSW, urban residents experienced a significantly higher risk of mortality from influenza and pneumonia in 1918–1919 than did rural residents (Table 1). However, soldiers of urban origin, from both the USA and Australia, experienced significantly lower mortality than soldiers of rural origin (Tables 1 and 2). In a multivariable analysis, both urban origin (OR 0·65, 95% CI 0·53–0·81) and veteran status (OR 0·23, 95% CI 0·15–0·36) remained significantly associated with reduced mortality in Australian soldiers (Table 2). No interaction between urban/rural origin and veteran status was found (P=0·99). The odds of death in veterans of urban origin was 0·15 (95% CI 0·07–0·35) times lower than in non-veterans of rural origin, consistent with separate protection from urban origin and veteran status. No interaction was found between birth year and veteran status (P=0·29). There was a significant interaction between urban/rural origin and birth year (P=0·04). Upon stratification by birth year, the apparent protective effect of urban origin in soldiers from Queensland, NSW and Victoria appeared to be stronger in those born prior to 1889 (Table 3). The number of Australian soldiers in each subgroup of exposure category is given in Supplementary Table S1 (available online).
Table 1. Mortality (deaths per 1000 population) during the 1918–1919 influenza pandemic

RR, Relative risk; CI, confidence interval.
* Relative risk of death recorded as due to influenza or pneumonia from October to December 1918.
† Relative risk of death recorded as due to influenza from January to September 1919 (taken directly from [3]).
‡ Relative risk of death recorded as due to influenza or pneumonia between 15 September and 15 November 1918.
Table 2. Mortality recorded as due to influenza or pneumonia during the 1918–1919 influenza pandemic in soldiers from Queensland, New South Wales and Victoria
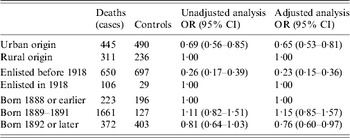
OR, Odds ratio; CI, confidence interval.
Table 3. Protective effect of urban origin against death recorded as due to influenza or pneumonia during the 1918–19 influenza pandemic in soldiers from Queensland, New South Wales and Victoria, stratified by birth year

OR, Odds ratio; CI, confidence interval.
* Odds ratio adjusted for veteran status.
DISCUSSION
In our analysis of three separate civilian populations, mortality due to influenza or pneumonia in late 1918 was lower in individuals of rural rather than urban residence, confirming previous observations. In our analysis of three separate military populations, mortality was higher in individuals of rural rather than urban origin, with all three studies exhibiting similar effect estimates. In the Introduction we posed the question: was higher mortality in civilian urban residents due to the urban environment or due to intrinsic host susceptibility in people of urban origin? In soldiers recruited from the same states as in the civilian analysis, those originating from urban areas had lower mortality. This implies that soldiers from urban backgrounds were intrinsically protected from death, as exposure to infectious agents would be expected to be similar for soldiers from both urban and rural backgrounds as they were mixed into various military units. Thus the mechanism underlying the lower mortality in civilian rural populations appears to be environmental, probably due to the relative social isolation in rural populations. In 1918 influenza spread effectively through all populations, with similar incidence in urban and rural areas [Reference Nishiura and Chowell2, Reference Frost and Sydenstricker9, Reference Sydenstricker10]. Exposure to respiratory bacteria, however, may have varied more between rural and urban settings, as closer contact with greater numbers of persons is generally required to transmit bacterial respiratory infections [Reference Ladhani11, 12]. As most respiratory bacterial disease appears due to newly acquired strains of bacteria [Reference Gray, Converse and Hugh13], this factor may account for the protective effect of the rural setting. Consistent with this idea, meningitis due to pneumococcus and Haemophilus influenzae was found to be higher in urban compared to rural Tennessee in the 1960s [Reference Floyd, Federspiel and Schaffner14].
The second question we investigated was whether the reduced mortality in military veterans was a result of the same mechanism as the reduced mortality found in soldiers of urban origin. Our results suggest separate protective effects were associated with veteran status and urban origin in these soldiers. With the data available here it is not possible to determine the mechanisms of these apparent protective effects. It is likely that they were due to acquired immunity resulting from previous pathogen exposures, although whether this was from protection from influenza infection itself or from secondary bacterial infection is unclear. The protective effect associated with urban origin varied according to birth year, with the strongest association in the oldest soldiers (Table 3). This is consistent with protection resulting from exposure to influenza viruses circulating either before or during the 1889–1891 pandemic; however, it is also consistent with a gradual accumulation of immunity to either influenza or bacterial pneumonia in members of successive birth cohorts over time. The apparently separate protective effect associated with veteran status may have been due either to exposure to ‘herald’ waves of influenza transmission in late 1917 or early 1918, or possibly due to prior exposure to respiratory bacteria in the confined wartime conditions [Reference Crum15]. As the pandemic did not reach Australia until 1919, Australian soldiers already based overseas at the start of 1918 would have had a greater chance of exposure to herald waves than those who enlisted in 1918.
A key strength of this study is using the military setting to examine the difference in intrinsic host susceptibility between individuals of urban and rural origin, removing potential confounding due to differences in pathogen exposure in the civilian setting. Another strength compared to previous studies is adjustment for age, measured using categories of birth year, an important confounder for mortality during the 1918 pandemic. A limitation is that this study cannot specify the mechanisms of the observed protective effects, apart from differentiating between environmental and intrinsic host mechanisms. We have discussed how previous exposures to respiratory pathogens may explain the protective effects observed in soldiers. An alternative explanation for these effects would be differences in underlying health. Although we could not control directly for differences in underlying health in our study subjects, recruits underwent health screening before entry into the military, standardizing the level of background health to an extent. For Kansas and Indiana, rejection rates for recruits following medical examination were available and for both states rejection rates were higher in urban recruits, implying that if anything general health was worse in urban areas at the time, making this an unlikely cause for the intrinsic host protection seen in soldiers of urban origin. The protection in civilian populations afforded by rural environment was probably due to relative social isolation in rural populations. We were unable to control for air pollution in urban areas as a potential confounder. In the Australian military study, there is likely to have been some measurement error in assigning urban/rural origin according to the postcode of enlistment office, as rural residents may have travelled to cities to enlist. This error would have been similar in cases and controls, thus any resulting bias would have been non-differential. As the US population was becoming more urbanized with time, using 1920 census data for the denominators of the civilian mortality rates in 1918 may have relatively overestimated the mortality in the civilian rural population. This would not have changed the conclusions of the study.
Mortality during the 1918 pandemic varied substantially between different populations. This study demonstrates that both setting and intrinsic host factors reduced mortality. This has relevance for influenza control today, and is encouraging for pandemic planning. The protection given by rural setting suggests that social distancing interventions may protect against mortality rather than just delaying infection, possibly by reducing the risk of acquiring new respiratory bacteria while vulnerable following influenza infection. Our analysis of Australian soldiers suggests two separate intrinsic host factors were reducing mortality. These effects were probably due to immunity acquired from previous pathogen exposures. The substantial size of both of these protective effects makes them very relevant to pandemic planning, and justifies further study to elucidate the exact underlying mechanisms.
NOTE
Supplementary material accompanies this paper on the Journal's website (http://journals.cambridge.org/hyg).
ACKNOWLEDGEMENTS
We thank Alison MacKenzie of the Centre for Military and Veterans Health at the University of Queensland, Brisbane, Australia for her help with data management, and John Brundage of the US Armed Forces Health Surveillance Center, Silver Spring, MD, USA for his review of the manuscript.
The Armed Forces Health Surveillance Center, Silver Spring, MD of the United States Department of Defense (http://www.afhsc.mil) provided funding for this project under the Global Emerging Infectious Disease and Response System [I0010_09_OT], but had no role in study design, data collection, analysis, interpretation or decision to publish.
DECLARATION OF INTEREST
None.







